
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Sirius Huang | -- | 3605 | 2022-11-03 01:31:25 |
Video Upload Options
The “Selfish Brain” theory describes the characteristic of the human brain to cover its own, comparably high energy requirements with the utmost of priorities when regulating energy fluxes in the organism. The brain behaves selfishly in this respect. The "Selfish brain" theory amongst other things provides a possible explanation for the origin of obesity, the severe and pathological form of overweight. The Luebeck obesity and diabetes specialist Achim Peters developed the fundamentals of this theory between 1998 and 2004. The interdisciplinary “Selfish Brain: brain glucose and metabolic syndrome” research group headed by Peters and supported by the German Research Foundation (DFG) at the University of Luebeck has in the meantime been able to reinforce the basics of the theory through experimental research.
1. The Explanatory Power of the Selfish Brain Theory
1.1. Investigative Approach of the Selfish Brain Theory
The brain performs many functions for the human organism. Most are of a cognitive nature or concern the regulation of the motor system. A previously lesser investigated aspect of brain activity was the regulation of energy metabolism. The "Selfish Brain" theory shed new light on this function. It states that the brain behaves selfishly by controlling energy fluxes in such a way that it allocates energy to itself before the needs of the other organs are satisfied. The internal energy consumption of the brain is very high. Although its mass constitutes only 2% of the entire body weight,[1] it consumes 20% of the carbohydrates ingested over a 24-hour period.[2] This corresponds to 100 g of glucose per day, or half the daily requirement for a human being. A 30-year-old office worker with a body weight of 75 kg and a height of 1.85 m consumes approx. 200 g glucose per day.
Before now the scientific community assumed that the energy needs of the brain, the muscles and the organs were all met in parallel. The hypothalamus, an area of the upper brainstem, was thought to play a central role in regulating two feedback loops within narrow limits.
- The "lipostatic theory" established by Gordon C Kennedy in 1953 describes the fat deposition feedback system.[3] The hypothalamus receives signals from circulating metabolic products or hormones about how much adipose tissue there is in the body as well as its prevailing metabolic status. Using these signals the hypothalamus can adapt the absorption of nutrients so that the body’s fat depots remain constant, i.e. a "lipostasis" is achieved.
- The "glucostatic theory" developed in the same year by Jean Mayer describes the blood glucose feedback system.[4] According to this theory the hypothalamus controls the absorption of nutrients via receptors that measure the glucose level in the blood. In this way a certain glucose concentration is set by adjusting the intake of nutrients. Mayer also included the brain in his calculations. Although he considered that food intake served to safeguard the energy homoeostasis of the central nervous system, he did imply that the energy flux from the body to the brain was a passive process.
On the basis of these theories a number of international research groups still position the origin of obesity in a disorder in one of the two above described feedback systems. However, there are scenarios in weight regulation that can not be explained in this way. For example, upon inanition of the body (e.g. during fasting) almost all the organs such as the heart, liver, spleen and kidneys dramatically lose weight (approx. 40%) and the blood glucose concentration falls. During this time, however, the brain mass hardly changes (less than 2% on average).[5] A further example illustrates the inherent conflict between these two explanatory approaches: although large amounts of the appetite suppressing hormone leptin are released in obese individuals, they are still afflicted with a ravenous hunger once their blood glucose falls.
The "Selfish Brain" theory links in seamlessly with the traditions of the lipo- and glucostatic theories. What is new is that the “Selfish Brain” theory assumes there is another feedback control system that is supraordinate to the blood glucose and fat feedback control systems.
A feedback system is meant here in which the cerebral hemispheres, the integrating organ for the entire central nervous system,[6][7] control the ATP concentration (adenosine-triposphate - a form of energy currency for the organism) of the neurons (see 3). In this way the cerebral hemispheres ensure the primacy of the brain’s energy supply and are therefore considered in the "Selfish Brain" theory as wings of a central authority that governs energy metabolism. Whenever required the cerebral hemispheres direct an energy flux from the body to the brain to maintain its energy status. In contrast to the ideas of Jean Mayer, the "Selfish Brain" theory assumes an active "Energy on Demand" process. It is controlled by cerebral ATP sensors that react sensitively to changes in ATP in neurons over the entire brain.
The "Selfish Brain" theory combines the theories of Kennedy and Mayer, considering blood glucose and fat feedback control systems as a complex. This regulates the energy flux from the environment to the body, i.e. the intake of nutrients. It is regulated by a hypothalamic nucleus. Here as well there are sensors that record changes in both blood glucose[8] and fat depots, and which activate biochemical processes that maintain a certain body weight.[9]
For achieving their goal of maintaining energy homeostasis in the brain, the cerebral hemispheres depend on subordinate feedback loops, since these loops send signals for energy procurement to their control organ. If these signals are not processed correctly, e.g. due to impairments in the amygdala or hippocampus, the energy supply to the brain will not be endangered, but anomalies such as obesity can still result. The origin of this is not to be found in the blood glucose or fat feedback control systems, but much rather in the regulating instances within the cerebral hemispheres.
1.2. Energy Procurement by the Brain
The brain can cover its energy needs (particularly those of the cerebral hemispheres) either by allocation or nutrient intake. The corresponding signal to the subordinate regulatory system originates in the cerebral hemispheres. The most phylogenetically recent part of the brain is characterized by a high plasticity and a high capacity to learn with this process. It is always able to adapt its regulatory processes by processing responses from the periphery, memorizing the results of individual feedback loops and behaviors, and anticipating any possible build-ups.
Energy procurement by the brain is complicated by three factors. Firstly, the brain always requests energy whenever it is needed. It can only store energy in a very restricted form. Peters therefore refers to this as an "energy on demand" system. Secondly, the brain is almost exclusively dependent on glucose as an ATP-substrate. Lactate and betahydroxybutyric acid can also be considered as substrates, but only under certain conditions, e.g. with considerable stress levels or malnutrition. Thirdly, the brain is separated from the rest of the body’s circulation by the blood-brain-barrier. The blood glucose has to be brought there via a special, insulin-independent transporter.
1.3. The Healthy and the Diseased Brain: Energy Supply through Allocation or Food Intake
Allocation represents the way a healthy brain secures its energy supply when acutely needed. It diverts blood glucose from the periphery and leads it across the blood-brain-barrier. An important role here is played by the stress system, whose neural pathways lead directly to the organs (heart, muscle, adipose tissue, liver, pancreas, etc.) and which also acts indirectly on these organs via the bloodstream by the stress hormones adrenaline and cortisol. This system ensures that the glucose is transported to the brain, and that uptake by the musculature and the adipose tissue is reduced. In order to achieve that, the release of insulin and its effect on organs is halted.
The acute supply of energy to the brain from the intake of nutrients presents problems for the organism. In the event of an emergency food intake is only activated if allocation is insufficient, and must be taken as a sign of disease. In this case the required energy can not be requested from the body, and it can only be taken directly from the environment. This pathology is due to defects lying within the control centers of the brain such as the hippocampus, amygdala and hypothalamus. These may be due to mechanical (tumors, injuries), genetic defects (lacking brain-derived neurotrophic factor (BDNF) receptors or leptin receptors), faulty programming (post-traumatic stress disorder, conditioning of eating behavior, advertising for sweets) or false signals may arise due to the influence of antidepressants, drugs, alcohol, pesticides, saccharin or viruses.
Such disorders can have a negative impact on a number of behavioral types:
- Eating behavior (eating, drinking)
- Social behavior (e.g. dealing with conflicts, sexuality)
- Behavior during food procurement (movement, orientation)
Diseases can then result. The "Selfish Brain” research group has concentrated above all on obesity as a pathology.
The following applies irrespective of the nature of energy provision: the brain never gives up on being selfish. Peters therefore differentiates the healthy from the diseased brain through its ability to compete for its energy requirements even under adverse conditions where there are excessive demands from the body. He contraposes the "selfish brain with high fitness" that can tap the bodies energy reserves even in times of short food supply at the expense of the body mass, and the "selfish brain with low fitness", that is unable to do this, and which instead takes in additional food and bears the risk of developing obesity.
1.4. Obesity - A Build-Up in the Supply Chain
The "Selfish Brain" theory can be considered as a new way to understand obesity.[10][11] Disorders in the control centers of the brain such as the hippocampus, amygdala and hypothalamus are thought to underlie this, as outlined above. Whatever the type of disruption that exists, it entails that the energy procurement for the brain is accomplished less by allocation and more by the intake of nutrients even though the muscles have no additional energy requirement. If one imagines the energy supply of the human organism as a supply-chain that passes from the outside world with its numerous options for nutrient intake via the body to the brain as the end user and control organ, then obesity can be considered as being caused by a build-up in this supply-chain. This is characterized by an excessive accumulation of energy in the adipose tissue or blood. An allocation failure is expressed as a weakening of the sympathetic nervous system (SNS). The result is that energy intended for the brain mainly enters buffer storage areas, i.e. the adipose tissue and the musculature. Only a small proportion reaches the brain. In order to cover its huge energy needs the brain commands the individual to consume more food. The accumulation process escalates, and the buffer storage areas are continuously filled up. This leads to the development of obesity. In many cases, at a time which is dependent on an affected individual's personal disposition, obesity can also be overlain by a diabetes mellitus. In such a situation the adipose tissue and musculature can no longer accept any energy, and the energy then accumulates in the blood so that hyperglycemia results.
2. Work on the "Selfish Brain" Theory
2.1. The Basics of the Theory
In 1998 Achim Peters drafted the basic version of the “Selfish Brain" theory and formulated its axioms. In his explanation of the “Selfish Brain” theory he referred to approx. 5000 published citations from classical endocrinology and diabetology and the modern neurosciences, but argued both mathematically (using differential equations) and system theoretically. That was a novel methodological approach for diabetology. The regulation of adenosine tripophoshate content plays a central role (a type of energy currency for the organism) in the brain.
Peters assumes a double feedback structure, where the ATP content in the neurons of the brain is stabilized by measurements from two sensors of differing sensitivity that produce the raw energy request signals. The more sensitive sensor records ATP deficits and induces an allocation signal for glucose that is compensated for by requests from the body. The other less sensitive sensor is only activated with glucose excesses and conveys a signal to halt the brain glucose allocation. The optimal ATP quantity is determined by the balance between these receptor signals.
Peters considers that the stress system also operates according to this double feedback structure, which is also closely related to the supply of glucose to the brain. If an individual is confronted with a stress-inducing stimulus, it responds with an increased central-nervous information processing and along with that an increased glucose requirement in the brain. The hormone cortisol, important for regulating stress reactions, and the hormone adrenaline, important for glucose procurement, are released from the adrenal glands. The amount of cortisol that is released is also determined by a balance between a sensitive and a less sensitive sensor, just as is the case with the control of ATP content. This process is terminated if the stress system returns to a resting state.
This model underlies the axioms for the “Selfish Brain" theory as developed by Peters:
- The ATP content in the brain is held constant within tight limits, irrespective of the state of the body
- The stress system strives to return to a resting state
2.2. Integrative Power of the “Selfish Brain" Theory
The "Selfish Brain" theory is an integrated concept, since from a methodological standpoint it can be seen as a union of two separate research directions. On the one hand it integrates peripheral metabolism research which investigates how energy metabolism functions through intake of nutrients into the organs of the body. On the other it incorporates the results of the brain metabolism expert Luc Pellerin from the University of Lausanne, who found that the neurons in the brain are supplied with energy via their neighboring astrocytes whenever required. This requirement oriented principle for the nerve cells is termed "Energy on demand".
With this approach the "Selfish Brain" theory recognizes the description of two ends of a supply chain. The brain doesn’t just control the supply chain, but it is also its end consumer, and not the body through which the supply chain passes. The priority of the brain implies that the regulation of energy supply in a human organism is accomplished by the demand rather than the supply principle: Energy is ordered when it is needed.
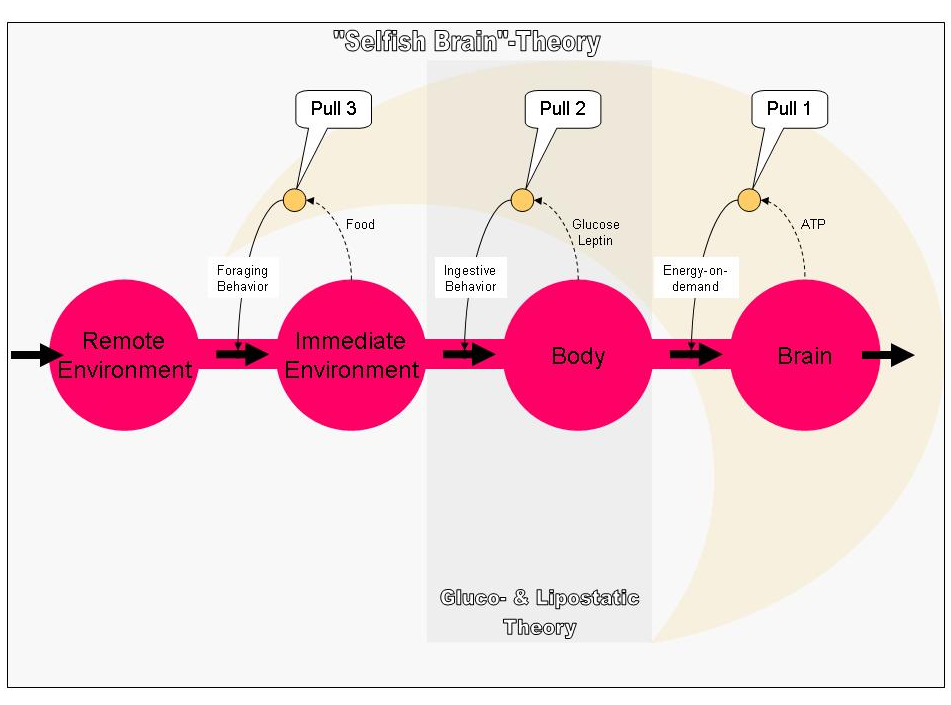
Fig. 1: Energy supply chain of the "Selfish Brain". If the ATP concentration drops in the nerve cells of the brain, a cerebral mechanism is (pull 1) set in motion which increases the energy flux directed from the body to the brain according to the "Energy on demand" principle. (solid arrows show stimulation, interrupted arrows inhibition; yellow means: "belongs to the controlling brain parts "). If the energy content in the body falls (blood, adipose tissue), the falling glucose and the falling adipose tissue hormone leptin induce another cerebral mechanism (pull 2). This entails that more energy is absorbed from the immediate environment into the body (ingestion behavior). When the available supplies in the immediate vicinity disappear, a further cerebral mechanism (pull 3) initiates moving and exploration, i.e. foraging for food. The glucostatic and the lipostatic theories describe the second step in this supply chain (area with dark grey background). The "Selfish Brain" theory links to the two traditional theories and expands them by considering the brain as an end consumer in a continuous supply chain (light gray). https://handwiki.org/wiki/index.php?curid=1633167
2.3. The Founding of the "Selfish Brain" Research Group
After the axioms were formulated in 1998 Achim Peters sought experts in other specialties to develop his "Selfish Brain" theory further. Already at an early stage he had matched up his ideas with the views of other leading international scientists. Amongst them was the Swiss brain metabolism specialist Luc Pellerin, the renowned obesity expert Denis G. Baskin, the internationally famous stress researcher Mary Dallman and the renowned neurobiologist Larry W. Swanson. At the University of Luebeck Achim Peters compared his findings with the well-known neuroendocrinologist Prof. Dr. Horst Lorenz Fehm. A year later in 1999 an intensive collaboration was started with the psychiatrist and psychotherapist Prof. Dr. Ulrich Schweiger who also worked at the University of Luebeck.
In 2004 the interdisciplinary research group: "Selfish Brain: brain glucose and metabolic syndrome" supported by the German Research Foundation (DFG) was officially founded. Achim Peters was appointed to a professorship that was especially created for the group. He also succeeded in winning over additional reputable scientists for the project, including Prof. Dr. Rolf Hilgenfeld, an eminent SARS expert and the developer of one of the first inhibitors of the virus. At this time the research group consists of 18 scientific subproject investigators from a number of specialties including internal medicine, psychiatry, neurobiology, molecular medicine and mathematics. The advisory committee includes Professors Luc Pellerin, Denis Baskin and Mary Dallman under its ranks.
2.4. "Train the Brain": a Therapy of Obesity Based on the "Selfish Brain" Theory
According to the “Selfish Brain” theory obesity can also be attributed to psychological causes. Poor coping strategies in stress situations represent one of these. An association was found between the tendency to evade conflict, and the habit of reducing psychological stress by immediately consuming sweets. The direct supply of glucose circumvents the glucose procurement from the body that would otherwise occur with a normal allocation process following the release of the stress hormone adrenaline. An existing allocation problem with obesity can be made even worse by such bad behavior. The stress system can also be weakened further because it may forget how to react autonomously.
These relationships have led to the development of an innovative multidisciplinary psychiatric and internal medical program at the University of Luebeck for obesity therapy. Prof. Dr. Ulrich Schweiger of the Clinic for Psychiatry and Psychotherapy led by Prof. Dr. F. Hohagen has been a key player in this development. In close cooperation with Schweiger, the internist Achim Peters derived a therapeutic concept from the “Selfish Brain” theory that was fixed on both feelings and coordinated behavior emanating from the brain. The aim of this therapy is to modify the settings and behaviors coded in the emotional memory centers of the brain that have become habit. "Train the Brain" is the catchphrase describing these therapeutic measures that may be enabled by the unusual plasticity and learning-capacity of the brain. It might just simply involve the practicing of eating behaviors that can be tolerated from a health perspective, and combining this with a reduction in detrimental habits. However, it could also involve the modification of behaviors associated with the handling of conflicts and other stress situations. According to the view of the “Selfish Brain” research group, if defective allocation is compensated for chronically by immediately consuming foodstuffs, a risk arises that eating will become the only reaction to a situation that requires a considerably more complex social behavior. The therapy of obesity therefore has both a physiological and a psychological component: It is not just the ability to allocate that must be restored, but actions and behaviors in everyday life.
2.5. Experimental Evidence─ the Theory’s Scope of Validity
In the first DFG funding period from 2004 to 2007 researchers from the Clinical Research Group “Selfish Brain: brain glucose and metabolic syndrome" expanded the scope of validity of the “Selfish Brain" theory in central aspects by carrying out experiments on healthy and diseased test subjects. The researchers in Luebeck found the following key results regarding the axioms of the theory:[12][13][14][15]
- The brain maintains its own glucose content "selfishly"
- The brain is always supplied with a greater energy share than the body in extreme stress situations
- In overweight individuals the brain’s energy distribution mechanism is disrupted
- With chronic stress loads the energy flux between the brain and the body is diverted, a phenomenon that leads to the development of overweight
- Nerve cells record their ATP content using two sensors of differing sensitivity
- The resting state of the stress system is fine-tuned with the help of two cortisol receptors of differing sensitivity
The special position of the brain during inanition (due to fasting or tumor disease) was already confirmed experimentally over 80 years ago: The body mass reduces, but the mass of the brain hardly reduces, if at all (see 3). Recently this axiom of the selfish brain theory was supported by work at the University of Luebeck involving state-of-the-art magnetic resonance procedures, e.g. during metabolic stress. The ATP content in the brain and musculature of test subjects was examined by a magnetic resonance technique while either an energy deficit or surplus was induced in the blood by insulin or glucose injection. In both situations a sufficiently high ATP-concentration was measured in the brain. The measured high-energy-rich substances changed throughout to the benefit of the brain and to the disadvantage of the body cells. The glucose-supply of the brain had priority despite the physical stress that was being endured (see 11).
Some of the results were presented at the international congress organized by the "Selfish Brain” research group at the 23 and 24 February 2006 in Luebeck as well as at a press conference aimed at both specialists and the wider public.
In the second funding period that has been running since the end of 2007, the clarification of the following questions has now become the focus of interest:
- How does the reward system of the "Selfish Brain" function and how does it lead amongst obese individuals to a faulty programming of energy management?
- How can the redirection of metabolic fluxes be learned and trained?
- How does "comfort feeding" affect stress reactions?
- How is the glucose requirement of the brain increased in stress situations?
- What does the molecular supply chain with which brain cells request glucose when needed look like?
- Can viruses block this supply chain for the brain cells?
References
- "Selfish brain theory". Prog. Brain Res. 153: 129–40. 2006. doi:10.1016/S0079-6123(06)53007-9. PMID 16876572. https://dx.doi.org/10.1016%2FS0079-6123%2806%2953007-9
- "Power of a human brain". http://hypertextbook.com/facts/2001/JacquelineLing.shtml.
- Kennedy 1953.
- Mayer 1953.
- Krieger 1921.
- Peters, Schweiger & Pellerin 2004.
- Peters, Pellerin & Dallman 2007.
- Burdakov, Jensen & Alexopoulos 2006.
- Morton et al. 2006.
- Wang & Mariman 2008.
- Kaulen 2008.
- Peters et al. 2007.
- Oltmanns, Melchert & Scholand-Engler 2008.
- Steinkamp et al. 2007.
- Schweiger, Greggersen & Rudolf 2008.





