
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Ashish Diwan | -- | 3426 | 2022-10-28 04:43:17 | | | |
| 2 | Catherine Yang | Meta information modification | 3426 | 2022-10-28 06:08:39 | | | | |
| 3 | Catherine Yang | -3 word(s) | 3423 | 2022-10-28 06:10:19 | | |
Video Upload Options
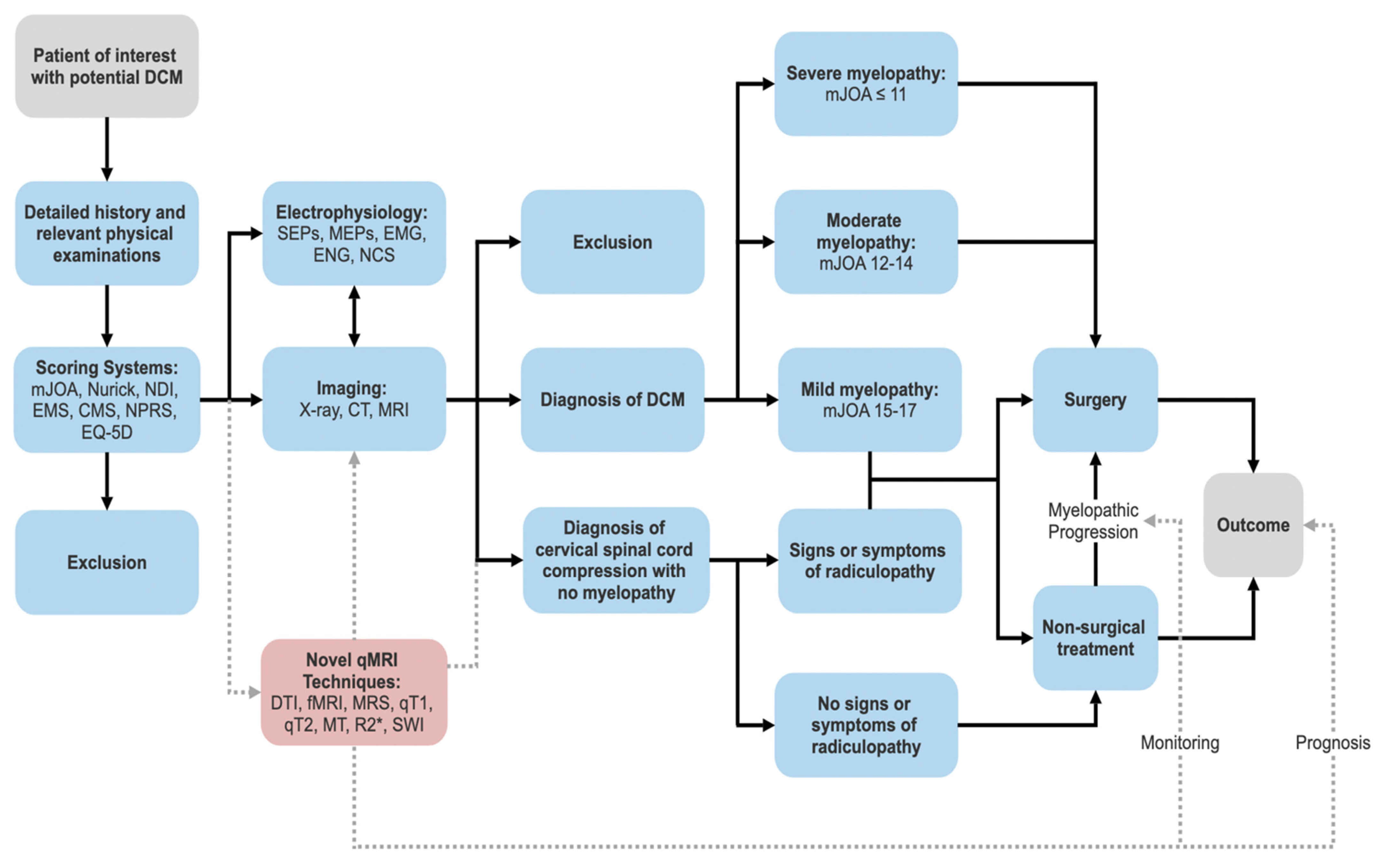
Degenerative cervical myelopathy (DCM) manifests as the primary cause of spinal cord dysfunction and is non-traumatic, chronic and progressive in nature. Decompressive surgery is typically utilised to halt further disability and neurological dysfunction and as such, early diagnosis and assessment is a vital means of slowing the disease process. Currently, there exists a plethora of methods for diagnosing DCM, each with their own unique limitations. The limitations of current diagnostic techniques and some novel quantitative MRI (qMRI) techniques for assessing spinal cord integrity in DCM were described here.
1. Epidemiology
2. Natural History
3. Current Diagnostic Options and Limitations
3.1. Clinical
| Presenting Symptoms | Physical Signs | |
|---|---|---|
| Neck |
|
|
| Upper Limb |
|
|
| Lower Limb |
|
|
| Urinary/defecatory |
|
|
3.2. Scoring Systems
Clinicians utilise scoring systems to categories the functional impairment of various conditions. Whilst different classifications may arise, there typically exists one standardised system for publications and treatments. This is not true for DCM; whereby different systems are utilised based upon preference. A 2016 systematic-review revealed that reported outcomes varied widely between studies of DCM [45]. Table 2 details the current most common classification systems, their benefits and limitations. The mJOA scale followed by the Nurick Grading system are the current most widely adopted measure for DCM patients [46].
However, the limitations covered in Table 2, are particularly problematic in mild DCM whereby strong floor and ceiling effects[e] in these scales inhibit ascertainment of more subtle neurological changes that provide information for decision-making in surgery [47]. As such, there exists the need to develop both a standardised scoring system and more sensitive and objective outcome instruments to enable more effective clinical assessment and efficient synthesis of research.
Table 2. Common classification systems used for DCM [48][49][50][51][52][53][54][55][56][57][58].
|
System |
Description |
Benefits |
Limitations |
|
mJOA scale |
- 0–18. A lower score indicates a more severe deficit. - Normal: 18 - Upper-extremity function (5) - Lower-extremity function (7) - Sensory function (3) - Bladder function (3) |
- Good for assessing outcomes (post-operative). - Specific to DCM - Responsive to change - Commonly used in research - Clinician administered |
- No economic factors taken into consideration. - Poor sensitivity - Ceiling effect: hard to detect minor improvements in patients with mild disease - Modest intra-rater and inter-rater reliability (the minimum detectable change is two points). - Four categories are not equally weighted. |
|
Nurick scale |
- 0–5. A higher grade indicates a more severe deficit. - Myelopathy (6 points) |
- Good for evaluating economic situation in conjunction with gait function. - Specific to DCM - Commonly used in research - Consists of both impairment and disability components |
- Low sensitivity - Poor responsiveness with limited ability to detect change. - Less accurate for post-operative grading. - Cannot detect upper extremity dysfunction. |
|
NDI |
- 0–50. A higher grade indicates a more severe disability. - Neck disability (10 subsections) - 0 = no disability - Consists of: Pain intensity, personal care, lifting, reading, headaches, concentration, work, driving, sleeping, recreation |
- Fair interobserver reliability in patients that have cervical radiculopathy - Responsive to change - Incorporates various activities from daily living |
- Validity and reliability only evaluated in neck pain patients and cervical radiculopathy patients - Subjective; patient reported - Not specific to DCM
|
|
EMS |
- 5–18. A lower score indicates a more severe deficit. - Normal: 17+ |
- Good at evaluating clinical state and level of severity. - Better sensitivity towards functional deficits (as it assesses coordination and proprioception) |
- Not commonly used in research |
|
CMS |
- Upper/lower extremities are analysed separately 0–5 each. - A higher grade indicates a more severe deficit. |
- Good for evaluating upper/lower extremity function as they are elicited separately. - Good at evaluating clinical state and level of severity. |
- No economic factors taken into consideration. |
|
NPRS |
- 0–10. A higher score indicates a more severe disability |
- Simplicity and reproducibility - Sensitive to small changes - Valid |
- Not specific to DCM - Subjective - Suffers from the ceiling effect |
|
EQ-5D |
- A standardised measure of health status looking into mobility, self-care, activities of daily living, pain/discomfort, anxiety/depression. - Not measured on a numbered scale |
- Ease of completion - Sensitive to change - Useful for looking into health economic evaluations |
- Emotions and mood are limited to anxiety and depression - Quite global in nature - Overlooks some dimensions of quality of life (spiritual, social) - Does not include cognition - Not specific to DCM |
|
Additional scales that provide useful information in the context of DCM include the Myelopathy Disability Index, QuickDASH (assesses arm, shoulder and hand disability), the 30-Metre-Walk test, the Berg Balance Scale, GAITRite (a temporospatial gait analysis) and the Graded Redefined Assessment of Strength Sensibility and Prehension Myelopathy (GRASSP-M). |
|||
Abbreviations: CMS, Cervical Myelopathy Scale; DCM, degenerative cervical myelopathy; EMS, European Myelopathy Scale; mJOA, modified Japanese Orthopaedic Association; NDI, Neck Disability Index; NPRS, Numeric Pain Rating Scale.
3.3. Conventional MRI
Conventional MRI is the primary modality utilised for imaging in DCM as it enables high-resolution depiction of neural structures, bone and ligaments that are difficult to visualise in other scans [59]. Conventional MRI (such as T1-weighted and T2-weighted imaging) can characterise the degree and nature of degeneration (i.e., OPLL, spondylosis, disc herniation, hypertrophy of ligamentum flavum), identify spinal-cord compression, highlight changes in spinal-canal diameter, and detect changes in signal intensity [60][61][62]. MRI can also assist in ruling-out resembling differentials or other causes of myelopathy such as a tumour syringomyelia or demyelinating plaques [63][64][65]. CT myelography should be utilised in situations of MRI contraindication [66].
Identifying spinal-cord compression plays a pivotal role in treatment selection and outcome prediction and thus should be the foremost investigation. It is typically described based on the number of compression sites [67], appearance [68][69][70][71][72] or ratio between the anteroposterior diameter and the transverse diameter (CR = Compression Ratio) [66,67]. A maximum spinal-cord compression (MSCC) index has also been developed by Fehlings et al. as a measurement of spinal-cord compression [73]. The primary object of these methods is to determine severity of spinal-cord compression.
Measurements of the anterior-posterior diameter at the region of interest (ROI) can be undertaken to evaluate the degree of spinal-stenosis [67]. Similar to MSCC, Fehlings et al. have developed a protocol to assess the maximum canal compromise (MCC) post-traumatic cervical spine-injury [74]. This has been additionally utilised for degenerative conditions and functions by calculating the canal size at the ROI and analysing it in conjunction to the average canal size for levels above and below. Multi-level signal-intensity changes are suggestive of necrosis or cavitation in the spinal cord and lend to poorer surgical outcomes [75][76][77][78]. T2-hyperintensity in conjunction with T1-hypointensity is associated with greater clinical deterioration when compared to T2-hyperintensity alone due to signal changes in T1-weighted images indicative of more permanent insult [75][79][80][81][82].
Limitations: Findings on conventional MRI do not typically correlate well with the variable clinical presentations of DCM [65]. Although spinal-cord compression is a sensitive marker of myelopathy [83], approximately 5% of asymptomatic patients also present with it [65], thereby limiting its specificity. The supine patient positioning in conventional MRI hinders its utility in assessing alignment, providing only a superficial assessment for situations in which upright films are not available [84]. Conventional MRI is intrinsically limited in its capability to characterize tissue injury in the spinal-cord because of the lack of specificity in T1/T2WI signal-change and cannot highlight specific pathophysiological processes at a cellular level (demyelination, axonal loss, inflammation, oedema, gliosis and apoptosis) [59]. It also is not a good predictor of neurologic function before/after surgical intervention and has low sensitivity for structural spinal cord change in cervical myelopathy [59][75][85][86][87][88].
3.4. Plain Radiographs and Computed Tomography (CT)
Computed Tomography is useful for the study of bone anatomy and can aid in cases where spinal-fusion is being considered as a treatment. In cases where MRI is contraindicated (such as the presence of pacemakers or other internal metallic objects), CT is a valuable imaging alternative. Plain radiographs can provide useful information about spinal-canal stenosis, degenerating discs, degenerating joints, OPLL, vertebrae fusion, cervical-spine alignment and subluxation [63][64][89][90]. This can reveal scoliosis and loss of physiological cervical-lordosis and kyphosis. Lateral-films in cervical-flexion and extensions are utilised to evaluate instability of the cervical-spine. DCM patients frequently showcase increased C2-C7 Cobb angles, upper T1 slopes, lower C7 slopes and upper C7 slopes [91].
Limitations: Computed tomography suffers the same inability to characterise tissue injury that conventional MRI does [59]. In addition, a 2017 systematic-review found that the overall strength of evidence regarding the predictive value that CT parameters have for the clinical presentation or outcome of DCM is low [92]. There is also the issue of radiation exposure. Overall CT and plain radiographs play a more complementary role in DCM diagnosis, acting as an alternative to MRI and aiding in surgical-planning [93].
3.5. Electrophysiology
Several studies have indicated good correlation between electrophysiology and the severity of myelopathy, presenting it as a reliable predictor of surgical-outcomes [94]. Somatosensory evoked-potentials (SEPs) and motor evoked-potentials (MEPs) can be, respectively, utilised to detect central sensory conduction impairment and prolonged motor latency in DCM [63][94][95]. They are also useful in detecting subclinical degenerative spinal-cord compression in asymptomatic patients and are thus useful in early identification of patients likely to develop myelopathy [96][97][98][99]. Feng et al. reported a correlation between the SEP and a declining mJOA (a more severe deficit) in an investigation of progressive myelopathy [100]. Needle electromyography (EMG) is a highly sensitive indicator of anterior horn cells damage, which occurs due to compression and ischemia in DCM [101]. Nerve-conduction studies can also be used to rule out peripheral neuropathy and nerve-entrapment [63]. These techniques also allow other neuromuscular diseases that can mimic DCM to be ruled out (motor neurone disease, ALS) [102][103]. Apart from aiding in diagnosis and preoperative evaluation, electrophysiology facilitates longitudinal assessment. Capone et al. found that a decrease in central-motor conduction time for the tibialis-anterior muscle correlated with an increased mJOA score post-surgery. It therefore concluded that the beneficial effects of spinal-cord surgery could be detected with MEP, making it a useful tool in determining efficacy of post-operative rehabilitation[104].
Limitations: Electrophysiology provides no anatomical information and thus cannot determine the exact location of the lesion [105]. Although some evidence exists to justify the effectiveness of electrophysiology in predicting operative outcomes, the area remains to be better defined. A systematic review found a decrease in electrophysiology publications compared with other domains of DCM, suggesting a declining interest in this area [106]. Additional studies would be required before it can be universally recommended.
4. Novel qMRI Modalities and Parameters
[108][109][110][111][112][115][116][117][118][119][120][121][122][123][124][125][126].
|
Sequence |
Function |
Quantitative Metrics |
|
|
Quantitative T1/T2 Mapping |
Calculates the T1/T2 time of certain tissues and displays them on a parametric map. Reveals information about microstructural changes related to water, lipid, protein and iron content of tissues. |
T1/T2 relaxation time |
|
|
DWI |
DTI |
Estimates the integrity of tissue microstructure through the modelling of water diffusion within the tissue. |
FA [f], ADC, MD [g] |
|
DTT |
Tracks nerve fibres based on their FA values and can be elicited when fibres become interrupted, distorted or disorientated depending on the severity of spinal compression. |
Volume and number of fibres |
|
|
DBSI |
Quantifies axonal injury, inflammation and demyelination in DCM |
Axonal injury, inflammation, demyelination. |
|
|
fMRI (BOLD) |
Measures neuronal activity through associated changes detected in blood flow |
FC, VOA |
|
|
MT |
Provides information on the spinal cord structural integrity and derive information regarding myelination status |
MTR |
|
|
MRS |
Sensitive to metabolic changes that occur in pathology, reflecting important underlying biological mechanisms |
Metabolite concentrations |
|
|
T2*-weighted imaging |
Quantifies observable or effective T2 and is utilised to detect deoxyhaemoglobin, hemosiderin or methemoglobin in tissues and lesions. |
R2* (=1/T2*) |
|
|
SWI/QSM |
Sensitive to compounds that distort the magnetic field and alter phase of tissue and is therefore commonly used to detect blood products/haemorrhage and calcium |
Tissue susceptibility |
|
Abbreviations: ADC, apparent diffusion coefficient; BOLD, blood oxygen level dependent; DBSI, diffusion basis spectrum imaging; DCM, degenerative cervical myelopathy; DTI, diffusion tensor imaging; DTT, diffusion tensor tractography; DWI, diffusion weighted imaging; FA, fractional anisotropy; FC, functional connectivity; fMRI, functional magnetic resonance imaging; MD, mean diffusivity; MRS, magnetic resonance spectroscopy; MT, magnetisation transfer; MTR, magnetisation transfer ratio; QSM, quantitative susceptibility mapping; SWI, susceptibility weighted imaging; VOA, volume of activation. [f] Fractional anisotropy (FA): Water molecules diffuse differently along tissues depending on its type, integrity, architecture, and presence of barriers. Fractional anisotropy is a value between 0 and 1 which indicates the degree to which diffusion of water is limited to one axis; [g] Apparent diffusion coefficient (ADC)/mean diffusivity (MD): measures of the average magnitude of water diffusion within a tissue.
References
- The Lancet Neurology. A focus on patient outcomes in cervical myelopathy. Lancet Neurol. 2019, 18, 615.
- Tracy, J.A.; Bartleson, J. Cervical spondylotic myelopathy. Neurology 2010, 16, 176–187.
- Ide, M.; Ogata, H.; Tokuhiro, A.; Takechi, H. Spinal cord injuries in Okayama Prefecture: An epidemiological study 88–89. J. UOEH 1993, 15, 209–215.
- McKinley, W.O.; Seel, R.T.; Hardman, J.T. Nontraumatic spinal cord injury: Incidence, epidemiology, and functional outcome. Arch. Phys. Med. Rehabil. 1999, 80, 619–623.
- New, P.W. Functional outcomes and disability after nontraumatic spinal cord injury rehabilitation: Results from a retrospective study. Arch. Phys. Med. Rehabil. 2005, 86, 250–261.
- New, P.W.; Rawicki, H.B.; Bailey, M.J. Nontraumatic spinal cord injury: Demographic characteristics and complications. Arch. Phys. Med. Rehabil. 2002, 83, 996–1001.
- New, P.W.; Cripps, R.A.; Lee, B.B. Global maps of non-traumatic spinal cord injury epidemiology: Towards a living data repository. Spinal Cord 2014, 52, 97–109.
- Biering-Sørensen, F.; Pedersen, V.; Clausen, S. Epidemiology of spinal cord lesions in Denmark. Spinal Cord 1990, 28, 105–118.
- Ronen, J.; Goldin, D.; Bluvshtein, V.; Fishel, B.; Gelernter, I.; Catz, A. Survival after nontraumatic spinal cord lesions in Israel. Arch. Phys. Med. Rehabil. 2004, 85, 1499–1502.
- Catz, A.; Goldin, D.; Fishel, B.; Ronen, J.; Bluvshtein, V.; Gelernter, I. Recovery of neurologic function following nontraumatic spinal cord lesions in Israel. Spine 2004, 29, 2278–2282.
- Citterio, A.; Franceschini, M.; Spizzichino, L.; Reggio, A.; Rossi, B.; Stampacchia, G.; Mielolesioni, G.I.S.E. Nontraumatic spinal cord injury: An Italian survey. Arch. Phys. Med. Rehabil. 2004, 85, 1483–1487.
- Scivoletto, G.; Farchi, S.; Laurenza, L.; Molinari, M. Traumatic and non-traumatic spinal cord lesions: An Italian comparison of neurological and functional outcomes. Spinal Cord 2011, 49, 391–396.
- Schönherr, M.; Groothoff, J.; Mulder, G.; Eisma, W. Rehabilitation of patients with spinal cord lesions in The Netherlands: An epidemiological study. Spinal Cord 1996, 34, 679–683.
- Buchan, A.; Fulford, G.; Harris, P.; Jellinek, E.; Kerr, W.; Kirkland, I.; Newsam, J.; Stark, G. A preliminary survey of the incidence and aetiology of spinal paralysis. Spinal Cord 1972, 10, 23–28.
- New, P.W.; Farry, A.; Baxter, D.; Noonan, V. Prevalence of non-traumatic spinal cord injury in Victoria, Australia. Spinal Cord 2013, 51, 99–102.
- Nouri, A.; Tetreault, L.; Singh, A.; Karadimas, S.K.; Fehlings, M.G. Degenerative cervical myelopathy: Epidemiology, genetics, and pathogenesis. Spine 2015, 40, E675–E693.
- Tu, J.; Vargas Castillo, J.; Das, A.; Diwan, A.D. Degenerative Cervical Myelopathy: Insights into Its Pathobiology and Molecular Mechanisms. J. Clin. Med. 2021, 10, 1214.
- Badhiwala, J.H.; Witiw, C.D.; Nassiri, F.; Akbar, M.A.; Mansouri, A.; Wilson, J.R.; Fehlings, M.G. Efficacy and safety of surgery for mild degenerative cervical myelopathy: Results of the AOSpine North America and international prospective multicenter studies. Neurosurgery 2019, 84, 890–897.
- Badhiwala, J.H.; Wilson, J.R. The natural history of degenerative cervical myelopathy. Neurosurg. Clin. 2018, 29, 21–32.
- Nakamura, K.; Kurokawa, T.; Hoshino, Y.; Saita, K.; Takeshita, K.; Kawaguchi, H. Conservative treatment for cervical spondylotic myelopathy: Achievement and sustainability of a level of “no disability”. J. Spinal Disord. 1998, 11, 175–179.
- Clarke, E.; Robinson, P.K. Cervical myelopathy: A complication of cervical spondylosis. Brain 1956, 79, 483–510.
- Bednarík, J.; Kadanka, Z.; Vohánka, S.; Stejskal, L.; Vlach, O.; Schröder, R. The value of somatosensory-and motor-evoked potentials in predicting and monitoring the effect of therapy in spondylotic cervical myelopathy: Prospective randomized study. Spine 1999, 24, 1593.
- Kadanka, Z.; Mareš, M.; Bednarík, J.; Smrcka, V.; Krbec, M.; Stejskal, L.; Chaloupka, R.; Dagmar, S.; Novotný, O.; Urbánek, I. Approaches to spondylotic cervical myelopathy: Conservative versus surgical results in a 3-year follow-up study. Spine 2002, 27, 2205–2210.
- Kadaňka, Z.; Bednařík, J.; Novotný, O.; Urbánek, I.; Dušek, L. Cervical spondylotic myelopathy: Conservative versus surgical treatment after 10 years. Eur. Spine J. 2011, 20, 1533–1538.
- Kadaňka, Z.; Bednařík, J.; Voháňka, S.; Vlach, O.; Stejskal, L.; Chaloupka, R.; Filipovičová, D.; Šurelová, D.; Adamová, B.; Novotný, O. Conservative treatment versus surgery in spondylotic cervical myelopathy: A prospective randomised study. Eur. Spine J. 2000, 9, 538–544.
- Kadaňka, Z.; Mareš, M.; Bednařík, J.; Smrčka, V.; Krbec, M.; Chaloupka, R.; Dušek, L. Predictive factors for mild forms of spondylotic cervical myelopathy treated conservatively or surgically. Eur. J. Neurol. 2005, 12, 16–24.
- Matsumoto, M.; Toyama, Y.; Ishikawa, M.; Chiba, K.; Suzuki, N.; Fujimura, Y. Increased signal intensity of the spinal cord on magnetic resonance images in cervical compressive myelopathy: Does it predict the outcome of conservative treatment? Spine 2000, 25, 677–682.
- Sampath, P.; Bendebba, M.; Davis, J.D.; Ducker, T.B. Outcome of patients treated for cervical myelopathy: A prospective, multicenter study with independent clinical review. Spine 2000, 25, 670–676.
- Matsumoto, M.; Chiba, K.; Ishikawa, M.; Maruiwa, H.; Fujimura, Y.; Toyama, Y. Relationships between outcomes of conservative treatment and magnetic resonance imaging findings in patients with mild cervical myelopathy caused by soft disc herniations. Spine 2001, 26, 1592–1598.
- Yoshimatsu, H.; Nagata, K.; Goto, H.; Sonoda, K.; Ando, N.; Imoto, H.; Mashima, T.; Takamiya, Y. Conservative treatment for cervical spondylotic myelopathy: Prediction of treatment effects by multivariate analysis. Spine J. 2001, 1, 269–273.
- Sumi, M.; Miyamoto, H.; Suzuki, T.; Kaneyama, S.; Kanatani, T.; Uno, K. Prospective cohort study of mild cervical spondylotic myelopathy without surgical treatment. J. Neurosurg. Spine 2012, 16, 8–14.
- Shimomura, T.; Sumi, M.; Nishida, K.; Maeno, K.; Tadokoro, K.; Miyamoto, H.; Kurosaka, M.; Doita, M. Prognostic factors for deterioration of patients with cervical spondylotic myelopathy after nonsurgical treatment. Spine 2007, 32, 2474–2479.
- Oshima, Y.; Seichi, A.; Takeshita, K.; Chikuda, H.; Ono, T.; Baba, S.; Morii, J.; Oka, H.; Kawaguchi, H.; Nakamura, K. Natural course and prognostic factors in patients with mild cervical spondylotic myelopathy with increased signal intensity on T2-weighted magnetic resonance imaging. Spine 2012, 37, 1909–1913.
- Rhee, J.; Tetreault, L.A.; Chapman, J.R.; Wilson, J.R.; Smith, J.S.; Martin, A.R.; Dettori, J.R.; Fehlings, M.G. Nonoperative versus operative management for the treatment degenerative cervical myelopathy: An updated systematic review. Glob. Spine J. 2017, 7, 35S–41S.
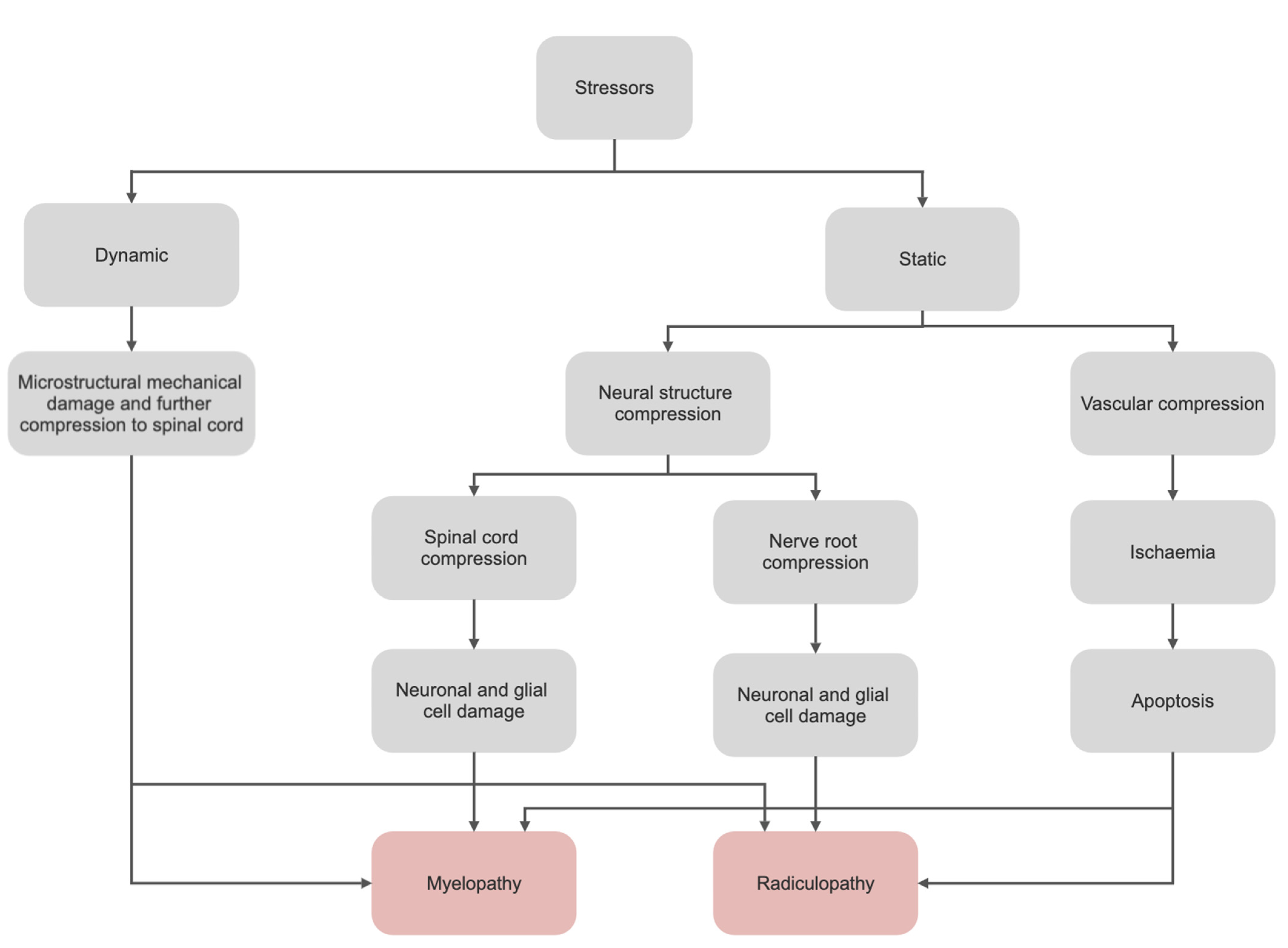
- Karadimas, S.; Erwin, W.; Ely, C.; Dettori, J.; Fehlings, M. Pathophysiology and natural history of cervical spondylotic myelopathy. Spine 2013, 38, S21–S36.
- Tetreault, L.A.; Karadimas, S.; Wilson, J.R.; Arnold, P.M.; Kurpad, S.; Dettori, J.R.; Fehlings, M.G. The natural history of degenerative cervical myelopathy and the rate of hospitalization following spinal cord injury: An updated systematic review. Glob. Spine J. 2017, 7, 28S–34S.
- Kalsi-Ryan, S.; Karadimas, S.K.; Fehlings, M.G. Cervical spondylotic myelopathy: The clinical phenomenon and the current pathobiology of an increasingly prevalent and devastating disorder. Neuroscientist 2013, 19, 409–421.
- Tetreault, L.; Goldstein, C.L.; Arnold, P.; Harrop, J.; Hilibrand, A.; Nouri, A.; Fehlings, M.G. Degenerative cervical myelopathy: A spectrum of related disorders affecting the aging spine. Neurosurgery 2015, 77, S51–S67.
- Davies, B.M.; Munro, C.F.; Kotter, M.R. A novel insight into the challenges of diagnosing degenerative cervical myelopathy using web-based symptom Checkers. J. Med. Internet Res. 2019, 21, e10868.
- Davies, B.M.; Mowforth, O.D.; Smith, E.K.; Kotter, M.R. Degenerative cervical myelopathy. BMJ 2018, 360, k186.
- Tetreault, L.; Kopjar, B.; Nouri, A.; Arnold, P.; Barbagallo, G.; Bartels, R.; Qiang, Z.; Singh, A.; Zileli, M.; Vaccaro, A. The modified Japanese Orthopaedic Association scale: Establishing criteria for mild, moderate and severe impairment in patients with degenerative cervical myelopathy. Eur. Spine J. 2017, 26, 78–84.
- Harrop, J.S.; Naroji, S.; Maltenfort, M.; Anderson, D.G.; Albert, T.; Ratliff, J.K.; Ponnappan, R.K.; Rihn, J.A.; Smith, H.E.; Hilibrand, A. Cervical myelopathy: A clinical and radiographic evaluation and correlation to cervical spondylotic myelopathy. Spine 2010, 35, 620–624.
- Iyer, A.; Azad, T.D.; Tharin, S. Cervical spondylotic myelopathy. Clin. Spine Surg. 2016, 29, 408–414.
- Cook, C.E.; Wilhelm, M.; Cook, A.E.; Petrosino, C.; Isaacs, R. Clinical tests for screening and diagnosis of cervical spine myelopathy: A systematic review. J. Manip. Physiol. Ther. 2011, 34, 539–546.
- Davies, B.M.; McHugh, M.; Elgheriani, A.; Kolias, A.G.; Tetreault, L.A.; Hutchinson, P.J.; Fehlings, M.G.; Kotter, M.R. Reported outcome measures in degenerative cervical myelopathy: A systematic review. PLoS ONE 2016, 11, e0157263.
- Kopjar, B.; Tetreault, L.; Kalsi-Ryan, S.; Fehlings, M. Psychometric properties of the modified Japanese Orthopaedic Association scale in patients with cervical spondylotic myelopathy. Spine 2015, 40, E23–E28.
- Badhiwala, J.H.; Witiw, C.D.; Nassiri, F.; Akbar, M.A.; Mansouri, A.; Wilson, J.R.; Fehlings, M.G. Efficacy and safety of surgery for mild degenerative cervical myelopathy: Results of the AOSpine North America and international prospective multicenter studies. Neurosurgery 2019, 84, 890–897.
- Tu, J.; Vargas Castillo, J.; Das, A.; Diwan, A.D. Degenerative Cervical Myelopathy: Insights into Its Pathobiology and Molecular Mechanisms. J. Clin. Med. 2021, 10, 1214.
- Revanappa, K.K.; Rajshekhar, V. Comparison of Nurick grading system and modified Japanese Orthopaedic Association scoring system in evaluation of patients with cervical spondylotic myelopathy. Eur. Spine J. 2011, 20, 1545–1551.
- Vitzthum, H.-E.; Dalitz, K. Analysis of five specific scores for cervical spondylogenic myelopathy. Eur. Spine J. 2007, 16, 2096–2103.
- Herdmann, J.; Linzbach, M.; Krzan, M.; Dvorak, J.; Bock, W. The European myelopathy score. In Cerebellar Infarct. Midline Tumors. Minimally Invasive Endoscopic Neurosurgery (MIEN); Springer: Berlin/Heidelberg, Germany, 1994; pp. 266–268.
- Lebl, D.R.; Hughes, A.; Cammisa, F.P., Jr.; O’leary, P.F. Cervical spondylotic myelopathy: Pathophysiology, clinical presentation, and treatment. HSS J. 2011, 7, 170–178.
- Singh, A.; Tetreault, L.; Casey, A.; Laing, R.; Statham, P.; Fehlings, M.G. A summary of assessment tools for patients suffering from cervical spondylotic myelopathy: A systematic review on validity, reliability and responsiveness. Eur. Spine J. 2015, 24, 209–228.
- Furlan, J.C.; Craven, B.C. Psychometric analysis and critical appraisal of the original, revised, and modified versions of the Japanese Orthopaedic Association score in the assessment of patients with cervical spondylotic myelopathy. Neurosurg. Focus 2016, 40, E6.
- Zhou, F.; Zhang, Y.; Sun, Y.; Zhang, F.; Pan, S.; Liu, Z. Assessment of the minimum clinically important difference in neurological function and quality of life after surgery in cervical spondylotic myelopathy patients: A prospective cohort study. Eur. Spine J. 2015, 24, 2918–2923.
- Singh, A.; Crockard, H. Comparison of seven different scales used to quantify severity of cervical spondylotic myelopathy and post-operative improvement. J. Outcome Meas. 2001, 5, 798–818.
- Iohom, G. Chapter 11—Clinical Assessment of Postoperative Pain. In Postoperative Pain Management; Shorten, G., Carr, D.B., Harmon, D., Puig, M.M., Browne, J., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2006; pp. 102–108.
- Balestroni, G.; Bertolotti, G. EuroQol-5D (EQ–5D): An instrument for measuring quality of life. Monaldi Arch. Chest Dis. 2012, 78, 155–159.
- Nouri, A.; Martin, A.R.; Mikulis, D.; Fehlings, M.G. Magnetic resonance imaging assessment of degenerative cervical myelopathy: A review of structural changes and measurement techniques. Neurosurg. Focus 2016, 40, E5.
- Nagata, K.; Kiyonaga, K.; Ohashi, T.; Sagara, M.; Miyazaki, S.; Inoue, A. Clinical value of magnetic resonance imaging for cervical myelopathy. Spine 1990, 15, 1088–1096.
- Sun, Q.; Hu, H.; Zhang, Y.; Li, Y.; Chen, L.; Chen, H.; Yuan, W. Do intramedullary spinal cord changes in signal intensity on MRI affect surgical opportunity and approach for cervical myelopathy due to ossification of the posterior longitudinal ligament? Eur. Spine J. 2011, 20, 1466–1473.
- Yang, Y.-M.; Yoo, W.-K.; Yoo, J.H.; Kwak, Y.H.; Oh, J.-K.; Song, J.-S.; Kim, S.W. The functional relevance of diffusion tensor imaging in comparison to conventional MRI in patients with cervical compressive myelopathy. Skelet. Radiol. 2017, 46, 1477–1486.
- Tracy, J.A.; Bartleson, J. Cervical spondylotic myelopathy. Neurology 2010, 16, 176–187.
- Tetreault, L.; Goldstein, C.L.; Arnold, P.; Harrop, J.; Hilibrand, A.; Nouri, A.; Fehlings, M.G. Degenerative cervical myelopathy: A spectrum of related disorders affecting the aging spine. Neurosurgery 2015, 77, S51–S67.
- Harrop, J.S.; Naroji, S.; Maltenfort, M.; Anderson, D.G.; Albert, T.; Ratliff, J.K.; Ponnappan, R.K.; Rihn, J.A.; Smith, H.E.; Hilibrand, A. Cervical myelopathy: A clinical and radiographic evaluation and correlation to cervical spondylotic myelopathy. Spine 2010, 35, 620–624.
- Houser, O.W.; Onofrio, B.M.; Miller, G.M.; Folger, W.N.; Smith, P.L. Cervical spondylotic stenosis and myelopathy: Evaluation with computed tomographic myelography. In Mayo Clinic Proceedings; Elsevier: Amsterdam, The Netherlands, 1994; Volume 69, pp. 557–563.
- Yoshimatsu, H.; Nagata, K.; Goto, H.; Sonoda, K.; Ando, N.; Imoto, H.; Mashima, T.; Takamiya, Y. Conservative treatment for cervical spondylotic myelopathy: Prediction of treatment effects by multivariate analysis. Spine J. 2001, 1, 269–273.
- Shimomura, T.; Sumi, M.; Nishida, K.; Maeno, K.; Tadokoro, K.; Miyamoto, H.; Kurosaka, M.; Doita, M. Prognostic factors for deterioration of patients with cervical spondylotic myelopathy after nonsurgical treatment. Spine 2007, 32, 2474–2479.
- Takahashi, M.; Yamashita, Y.; Sakamoto, Y.; Kojima, R. Chronic cervical cord compression: Clinical significance of increased signal intensity on MR images. Radiology 1989, 173, 219–224.
- Suzuki, A.; Daubs, M.D.; Inoue, H.; Hayashi, T.; Aghdasi, B.; Montgomery, S.R.; Ruangchainikom, M.; Hu, X.; Lee, C.J.; Wang, C.J. Prevalence and motion characteristics of degenerative cervical spondylolisthesis in the symptomatic adult. Spine 2013, 38, E1115–E1120.
- Muhle, C.; Metzner, J.; Weinert, D.; Falliner, A.; Brinkmann, G.; Mehdorn, M.H.; Heller, M.; Resnick, D. Classification system based on kinematic MR imaging in cervical spondylitic myelopathy. Am. J. Neuroradiol. 1998, 19, 1763–1771.
- Kang, Y.; Lee, J.; Koh, Y.; Hur, S.; Kim, S.; Chai, J. New MRI grading system for the cervical canal stenosis. AJR Am. J. Roentgenol. 2011, 197, W134–W140.
- Furlan, J.C.; Kailaya-Vasan, A.; Aarabi, B.; Fehlings, M.G. A novel approach to quantitatively assess posttraumatic cervical spinal canal compromise and spinal cord compression: A multicenter responsiveness study. Spine 2011, 36, 784–793.
- Fehlings, M.G.; Rao, S.C.; Tator, C.H.; Skaf, G.; Arnold, P.; Benzel, E.; Dickman, C.; Cuddy, B.; Green, B.; Hitchon, P. The optimal radiologic method for assessing spinal canal compromise and cord compression in patients with cervical spinal cord injury: Part II: Results of a multicenter study. Spine 1999, 24, 605–613.
- Nouri, A.; Martin, A.R.; Kato, S.; Kermani, H.R.; Riehm, L.; Fehlings, M.G. The Relationship Between MRI Signal Intensity Changes, Clinical Presentation and Surgical Outcome in Degenerative Cervical Myelopathy: Analysis of a Global Cohort. Spine J. 2017, 17, S133–S134.
- Uchida, K.; Nakajima, H.; Takeura, N.; Yayama, T.; Guerrero, A.R.; Yoshida, A.; Sakamoto, T.; Honjoh, K.; Baba, H. Prognostic value of changes in spinal cord signal intensity on magnetic resonance imaging in patients with cervical compressive myelopathy. Spine J. 2014, 14, 1601–1610.
- Papadopoulos, C.A.; Karonis, P.; Papagelopoulos, P.J.; Karampekios, S.; Hadjipavlou, A.G. Surgical Decompression for Cervical Spondylotic Myelopathy: Correlation between Operative Outcomes and MRI of the Spinal Cord; SLACK Incorporated: Thorofare, NJ, USA, 2004.
- de Rota, J.J.F.; Meschian, S.; de Rota, A.F.; Urbano, V.; Baron, M. Cervical spondylotic myelopathy due to chronic compression: The role of signal intensity changes in magnetic resonance images. J. Neurosurg. Spine 2007, 6, 17–22.
- Mastronardi, L.; Elsawaf, A.; Roperto, R.; Bozzao, A.; Caroli, M.; Ferrante, M.; Ferrante, L. Prognostic relevance of the postoperative evolution of intramedullary spinal cord changes in signal intensity on magnetic resonance imaging after anterior decompression for cervical spondylotic myelopathy. J. Neurosurg. Spine 2007, 7, 615–622.
- Yagi, M.; Ninomiya, K.; Kihara, M.; Horiuchi, Y. Long-term surgical outcome and risk factors in patients with cervical myelopathy and a change in signal intensity of intramedullary spinal cord on magnetic resonance imaging. J. Neurosurg. Spine 2010, 12, 59–65.
- Yukawa, Y.; Kato, F.; Yoshihara, H.; Yanase, M.; Ito, K. MR T2 image classification in cervical compression myelopathy: Predictor of surgical outcomes. Spine 2007, 32, 1675–1678.
- Nouri, A.; Tetreault, L.; Côté, P.; Zamorano, J.J.; Dalzell, K.; Fehlings, M.G. Does magnetic resonance imaging improve the predictive performance of a validated clinical prediction rule developed to evaluate surgical outcome in patients with degenerative cervical myelopathy? Spine 2015, 40, 1092–1100.
- Kato, F.; Yukawa, Y.; Suda, K.; Yamagata, M.; Ueta, T. Normal morphology, age-related changes and abnormal findings of the cervical spine. Part II: Magnetic resonance imaging of over 1200 asymptomatic subjects. Eur. Spine J. 2012, 21, 1499–1507.
- Wessberg, P.; Danielson, B.I.; Willén, J. Comparison of Cobb angles in idiopathic scoliosis on standing radiographs and supine axially loaded MRI. Spine 2006, 31, 3039–3044.
- Cowley, P. Neuroimaging of spinal canal stenosis. Magn. Reson. Imaging Clin. 2016, 24, 523–539.
- Karpova, A.; Arun, R.; Kalsi-Ryan, S.; Massicotte, E.M.; Kopjar, B.; Fehlings, M.G. Do quantitative magnetic resonance imaging parameters correlate with the clinical presentation and functional outcomes after surgery in cervical spondylotic myelopathy? A prospective multicenter study. Spine 2014, 39, 1488–1497.
- Li, F.; Chen, Z.; Zhang, F.; Shen, H.; Hou, T. A meta-analysis showing that high signal intensity on T2-weighted MRI is associated with poor prognosis for patients with cervical spondylotic myelopathy. J. Clin. Neurosci. 2011, 18, 1592–1595.
- Tetreault, L.A.; Dettori, J.R.; Wilson, J.R.; Singh, A.; Nouri, A.; Fehlings, M.G.; Brodt, E.D.; Jacobs, W.B. Systematic review of magnetic resonance imaging characteristics that affect treatment decision making and predict clinical outcome in patients with cervical spondylotic myelopathy. Spine 2013, 38, S89–S110.
- Taylor, A. Mechanism and treatment of spinal-cord disorders associated with cervical spondylosis. Lancet 1953, 261, 717–720.
- Xing, R.; Zhou, G.; Chen, Q.; Liang, Y.; Dong, J. MRI to measure cervical sagittal parameters: A comparison with plain radiographs. Arch. Orthop. Trauma Surg. 2017, 137, 451–455.
- Scheer, J.K.; Tang, J.A.; Smith, J.S.; Acosta, F.L.; Protopsaltis, T.S.; Blondel, B.; Bess, S.; Shaffrey, C.I.; Deviren, V.; Lafage, V. Cervical spine alignment, sagittal deformity, and clinical implications: A review. J. Neurosurg. Spine 2013, 19, 141–159.
- Waly, F.J.; Abduljabbar, F.H.; Fortin, M.; Nooh, A.; Weber, M. Preoperative computed tomography myelography parameters as predictors of outcome in patients with degenerative cervical myelopathy: Results of a systematic review. Glob. Spine J. 2017, 7, 521–528.
- Naderi, S.; Özgen, S.; Pamir, M.N.; Özek, M.M.; Erzen, C. Cervical spondylotic myelopathy: Surgical results and factors affecting prognosis. Neurosurgery 1998, 43, 43–49.
- Nardone, R.; Höller, Y.; Brigo, F.; Frey, V.; Lochner, P.; Leis, S.; Golaszewski, S.; Trinka, E. The contribution of neurophysiology in the diagnosis and management of cervical spondylotic myelopathy: A review. Spinal Cord 2016, 54, 756–766.
- Bischoff, C.; Meyer, B.U.; Machetanz, J.; Conrad, B. The value of magnetic stimulation in the diagnosis of radiculopathies. Muscle Nerve: Off. J. Am. Assoc. Electrodiagn. Med. 1993, 16, 154–161.
- Bednařík, J.; Kadaňka, Z.; Voháňka, S.; Novotný, O.; Šurelová, D.; Filipovičová, D.; Prokeš, B. The value of somatosensory and motor evoked potentials in pre-clinical spondylotic cervical cord compression. Eur. Spine J. 1998, 7, 493–500.
- Bednařík, J.; Sládková, D.; Kadaňka, Z.; Dušek, L.; Keřkovský, M.; Voháňka, S.; Novotný, O.; Urbánek, I.; Němec, M. Are subjects with spondylotic cervical cord encroachment at increased risk of cervical spinal cord injury after minor trauma? J. Neurol. Neurosurg. Psychiatry 2011, 82, 779–781.
- Bednarik, J.; Kadanka, Z.; Dusek, L.; Kerkovsky, M.; Vohanka, S.; Novotny, O.; Urbanek, I.; Kratochvilova, D. Presymptomatic spondylotic cervical myelopathy: An updated predictive model. Eur. Spine J. 2008, 17, 421–431.
- Wilson, J.R.; Barry, S.; Fischer, D.J.; Skelly, A.C.; Arnold, P.M.; Riew, K.D.; Shaffrey, C.I.; Traynelis, V.C.; Fehlings, M.G. Frequency, timing, and predictors of neurological dysfunction in the nonmyelopathic patient with cervical spinal cord compression, canal stenosis, and/or ossification of the posterior longitudinal ligament. Spine 2013, 38, S37–S54.
- Feng, X.; Hu, Y.; Ma, X. Progression Prediction of Mild Cervical Spondylotic Myelopathy by Somatosensory-evoked Potentials. Spine 2020, 45, E560–E567.
- Dvorak, J.; Sutter, M.; Herdmann, J. Cervical myelopathy: Clinical and neurophysiological evaluation. Aging Spine 2005, 12, 99–105.
- Tsiptsios, I.; Fotiou, F.; Sitzoglou, K.; Fountoulakis, K. Neurophysiological investigation of cervical spondylosis. Electromyogr. Clin. Neurophysiol. 2001, 41, 305–313.
- Liu, H.; MacMillian, E.L.; Jutzeler, C.R.; Ljungberg, E.; MacKay, A.L.; Kolind, S.H.; Mädler, B.; Li, D.K.; Dvorak, M.F.; Curt, A. Assessing structure and function of myelin in cervical spondylotic myelopathy: Evidence of demyelination. Neurology 2017, 89, 602–610.
- Capone, F.; Tamburelli, F.C.; Pilato, F.; Profice, P.; Ranieri, F.; Di Iorio, R.; Iodice, F.; Musumeci, G.; Di Lazzaro, V. The role of motor-evoked potentials in the management of cervical spondylotic myelopathy. Spine J. 2013, 13, 1077–1079.
- Michaud, J. Chapter 11—Peripheral Nerves. In Essential Applications of Musculoskeletal Ultrasound in Rheumatology; Wakefield, R.J., D’Agostino, M.A., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2010; pp. 121–136.
- Mowforth, O.D.; Davies, B.M.; Goh, S.; O’Neill, C.P.; Kotter, M.R. Research inefficiency in degenerative cervical myelopathy: Findings of a systematic review on research activity over the past 20 years. Glob. Spine J. 2020, 10, 476–485.
- Ellingson, B.M.; Cohen-Adad, J. Chapter 3.1—Diffusion-Weighted Imaging of the Spinal Cord. In Quantitative MRI of the Spinal Cord; Cohen-Adad, J., Wheeler-Kingshott, C.A.M., Eds.; Academic Press: San Diego, CA, USA, 2014; pp. 123–145.
- Grabher, P.; Mohammadi, S.; Trachsler, A.; Friedl, S.; David, G.; Sutter, R.; Weiskopf, N.; Thompson, A.J.; Curt, A.; Freund, P. Voxel-based analysis of grey and white matter degeneration in cervical spondylotic myelopathy. Sci. Rep. 2016, 6, 1–10.
- Grabher, P.; Mohammadi, S.; David, G.; Freund, P. Neurodegeneration in the Spinal Ventral Horn Prior to Motor Impairment in Cervical Spondylotic Myelopathy. J. Neurotrauma 2017, 34, 2329–2334.
- Martin, A.R.; De Leener, B.; Cohen-Adad, J.; Cadotte, D.W.; Nouri, A.; Wilson, J.R.; Tetreault, L.; Crawley, A.P.; Mikulis, D.J.; Ginsberg, H. Can microstructural MRI detect subclinical tissue injury in subjects with asymptomatic cervical spinal cord compression? A prospective cohort study. BMJ Open 2018, 8, e019809.
- Yoo, W.-K.; Kim, T.H.; Hai, D.M.; Sundaram, S.; Yang, Y.M.; Park, M.S.; Kim, Y.C.; Kwak, Y.H.; Ohn, S.H.; Kim, S.W. Correlation of magnetic resonance diffusion tensor imaging and clinical findings of cervical myelopathy. Spine J. 2013, 13, 867–876.
- Martin, A.R.; De Leener, B.; Cohen-Adad, J.; Kalsi-Ryan, S.; Cadotte, D.W.; Wilson, J.R.; Tetreault, L.; Nouri, A.; Crawley, A.; Mikulis, D.J. Monitoring for myelopathic progression with multiparametric quantitative MRI. PLoS ONE 2018, 13, e0195733.
- Wang, K.; Chen, Z.; Zhang, F.; Song, Q.; Hou, C.; Tang, Y.; Wang, J.; Chen, S.; Bian, Y.; Hao, Q. Evaluation of DTI parameter ratios and diffusion tensor tractography grading in the diagnosis and prognosis prediction of cervical spondylotic myelopathy. Spine 2017, 42, E202–E210.
- Zhang, H.; Guan, L.; Hai, Y.; Liu, Y.; Ding, H.; Chen, X. Multi-shot echo-planar diffusion tensor imaging in cervical spondylotic myelopathy: A longitudinal study. Bone Jt. J. 2020, 102, 1210–1218.
- Nouri, A.; Martin, A.R.; Kato, S.; Kermani, H.R.; Riehm, L.; Fehlings, M.G. The Relationship Between MRI Signal Intensity Changes, Clinical Presentation and Surgical Outcome in Degenerative Cervical Myelopathy: Analysis of a Global Cohort. Spine J. 2017, 17, S133–S134.
- Martin, A.R.; Aleksanderek, I.; Cohen-Adad, J.; Tarmohamed, Z.; Tetreault, L.; Smith, N.; Cadotte, D.W.; Crawley, A.; Ginsberg, H.; Mikulis, D.J. Translating state-of-the-art spinal cord MRI techniques to clinical use: A systematic review of clinical studies utilizing DTI, MT, MWF, MRS, and fMRI. NeuroImage Clin. 2016, 10, 192–238.
- Martin, A.; De Leener, B.; Cohen-Adad, J.; Cadotte, D.; Kalsi-Ryan, S.; Lange, S.; Tetreault, L.; Nouri, A.; Crawley, A.; Mikulis, D. Clinically feasible microstructural MRI to quantify cervical spinal cord tissue injury using DTI, MT, and T2*-weighted imaging: Assessment of normative data and reliability. Am. J. Neuroradiol. 2017, 38, 1257–1265.
- Summers, P.E.; Brooks, J.C.W.; Cohen-Adad, J. Chapter 4.1—Spinal Cord fMRI. In Quantitative MRI of the Spinal Cord; Cohen-Adad, J., Wheeler-Kingshott, C.A.M., Eds.; Academic Press: San Diego, CA, USA, 2014; pp. 221–239.
- Solanky, B.S.; De Vita, E. Chapter 5.1—Single Voxel MR Spectroscopy in the Spinal Cord: Technical Challenges and Clinical Applications. In Quantitative MRI of the Spinal Cord; Cohen-Adad, J., Wheeler-Kingshott, C.A.M., Eds.; Academic Press: San Diego, CA, USA, 2014; pp. 267–290.
- Laule, C.; MacKay, A. Chapter 3.5—T2 Relaxation. In Quantitative MRI of the Spinal Cord; Cohen-Adad, J., Wheeler-Kingshott, C.A.M., Eds.; Academic Press: San Diego, CA, USA, 2014; pp. 181–206.
- Kim, M.; Cercignani, M. Chapter 3.4—Magnetization Transfer. In Quantitative MRI of the Spinal Cord; Cohen-Adad, J., Wheeler-Kingshott, C.A.M., Eds.; Academic Press: San Diego, CA, USA, 2014; pp. 164–180.
- Brooks, J.C.W. Chapter 4.2—Physiological Noise Modeling and Analysis for Spinal Cord fMRI. In Quantitative MRI of the Spinal Cord; Cohen-Adad, J., Wheeler-Kingshott, C.A.M., Eds.; Academic Press: San Diego, CA, USA, 2014; pp. 240–257.
- Assaf, Y.; Alexander, D.C. Chapter 3.3—Advanced Methods to Study White Matter Microstructure. In Quantitative MRI of the Spinal Cord; Cohen-Adad, J., Wheeler-Kingshott, C.A.M., Eds.; Academic Press: San Diego, CA, USA, 2014; pp. 156–163.
- Abdel-Aziz, K.; Ciccarelli, O. Chapter 1.1—Rationale for Quantitative MRI of the Human Spinal Cord and Clinical Applications. In Quantitative MRI of the Spinal Cord; Cohen-Adad, J., Wheeler-Kingshott, C.A.M., Eds.; Academic Press: San Diego, CA, USA, 2014; pp. 3–21.
- Chavhan, G.B.; Babyn, P.S.; Thomas, B.; Shroff, M.M.; Haacke, E.M. Principles, techniques, and applications of T2 *-based MR imaging and its special applications. Radiographics 2009, 29, 1433–1449.
- Battiston, M.; Schneider, T.; Prados, F.; Grussu, F.; Yiannakas, M.C.; Ourselin, S.; Gandini Wheeler-Kingshott, C.A.; Samson, R.S. Fast and reproducible in vivo T1 mapping of the human cervical spinal cord. Magn. Reson. Med. 2018, 79, 2142–2148.




