
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Masaru Tanaka | -- | 1800 | 2022-10-24 12:26:49 | | | |
| 2 | Beatrix Zheng | + 27 word(s) | 1827 | 2022-10-25 03:16:49 | | | | |
| 3 | Beatrix Zheng | + 8 word(s) | 1835 | 2022-10-28 09:07:00 | | |
Video Upload Options
The blood–brain barrier (BBB) is poorly permeable to kynurenic acid (KYNA). The design of KYNA precursors that are highly penetrable across the BBB and convertible to an active form upon the entry has been under consideration. Another strategy is the administration of KYNA analogues that are highly penetrable to the BBB. The halogenation and conjugation of various side chains enables KYNA to cross the BBB easily, and the KYNA analogues have been shown to be more potent N-methyl-D-aspartate glutamatergic receptor (NMDAR) inhibitors. Meanwhile, inadequate nutritional status has been observed in patients with dementia. An active form of vitamin B6, pyridoxal 5′-phosphate (PLP) is a cofactor of KYN aminotransferas (KAT) enzymes, which are responsible for KYNA production. Therefore, vitamin B6 supplementation may be of important value to increase a level of KYNA in the brain. L-KYN is not only a precursor of KYNA, which is also produced at least partly from indole pyruvic acid (IPA) through redox reactions or the transamination of Tryptophan (TRP) . Little is studied about other routes of KYNA production and its influence on whole kynurenine (KYN) metabolism. In addition, D-enantiomers of amino acids and D-amino acid oxidase (DAAO) have been observed to contribute to L-amino acid concentration. D-TRP and D-KYN supplements and balancing the gastrointestinal microbiota responsible for conversion to L-enantiomers may be potential strategies to regulate KYN metabolism and maintain an adequate L-KYNA reservoir.
1. Prodrugs
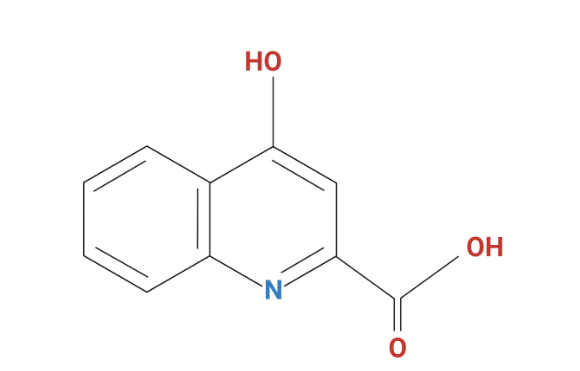
2. Kynurenic Acid Analogues
3. Kynurenine Aminotransferases Enzyme Potentiation
4. Indole-3-Pyruvic Acid Precursor and Reactive Oxygen Species
5. Amino Acid Oxidase and d-Amino Acids
References
- Sas, K.; Robotka, H.; Rózsa, É.; Ágoston, M.; Szénási, G.; Gigler, G.; Marosi, M.; Kis, Z.; Farkas, T.; Vécsei, L.; et al. Kynurenine diminishes the ischemia-induced histological and electrophysiological deficits in the rat hippocampus. Neurobiol. Dis. 2008, 32, 302–308.
- Kemp, J.A.; Foster, A.C.; Lesson, P.D.; Priestley, T.; Tridgett, R.; Iversen, L.L.; Woodruff, G.N. 7-Chlorokynurenic acid is a selective antagonist at the glycine modulatory site of the N-methyl-D-aspartate receptor complex. Proc. Natl. Acad. Sci. USA 1988, 85, 6547–6550.
- Vécsei, L.; Szalárdy, L.; Fülöp, F.; Toldi, J. Kynurenines in the CNS: Recent advances and new questions. Nat. Rev. Drug Discov. 2013, 12, 64–82.
- Gerhard, D.M.; Wohleb, E.S.; Duman, R.S. Emerging treatment mechanisms for depression: Focus on glutamate and synaptic plasticity. Drug Discov. Today 2016, 21, 454–464.
- VistaGen Reports Topline Phase 2 Results for AV-101 as an Adjunctive Treatment of Major Depressive Disorder. Available online: https://www.pharmasalmanac.com/articles/vistagen-reports-topline-phase-2-results-for-av-101-as-an-adjunctive-treatment-of-major-depressive-disorder (accessed on 4 December 2019).
- Fülöp, F.; Szatmári, I.; Vámos, E.; Zádori, D.; Toldi, J.; Vécsei, L. Syntheses, transformations and pharmaceutical applications of kynurenic acid derivatives. Curr. Med. Chem. 2009, 16, 4828–4842.
- Stone, T.W. Development and therapeutic potential of kynurenic acid and kynurenine derivatives for neuroprotection. Trends Pharmacol. Sci. 2000, 21, 149–154.
- Foster, A.C.; Kemp, J.A.; Leeson, P.D.; Grimwood, S.; Donald, A.E.; Marschall, G.R.; Priestley, T.; Smith, J.D.; Carling, R.W. Kynurenic acid analogues with improved affinity and selectivity for the glycine site on the N-methyl-D-aspartate receptor from rat brain. Mol. Pharmacol. 1992, 41, 914–922.
- Leeson, P.D.; Baker, R.; Carling, R.W.; Curtis, N.R.; Moore, K.W.; Williams, B.J.; Foster, A.C.; Donald, A.E.; Kemp, J.A.; Marshall, G.R. Kynurenic acid derivatives. Structure-activity relationships for excitatory amino acid antagonism and identification of potent and selective antagonists at the glycine site on the N-methyl-D-aspartate receptor. J. Med. Chem. 1991, 34, 1243–1252.
- Wu, H.Q.; Rassoulpour, A.; Goodman, J.H.; Scharfman, H.E.; Bertram, E.H.; Schwarcz, R. Kynurenate and 7-Chlorokynurenate Formation in Chronically Epileptic Rats. Epilepsia 2005, 46, 1010–1016.
- Feng, B.; Tang, Y.; Chen, B.; Xu, C.; Wang, Y.; Dai, Y.; Wu, D.; Zhu, J.; Wang, S.; Zhou, Y.; et al. Transient increase of interleukin-1β after prolonged febrile seizures promotes adult epileptogenesis through long-lasting upregulating endocannabinoid signaling. Sci. Rep. 2016, 6, 21931.
- Ohtani, K.; Tanaka, H.; Yoneda, Y.; Yasuda, H.; Ito, A.; Nagata, R.; Nakamura, M. In vitro and in vivo antagonistic activities of SM-31900 for the NMDA receptor glycine-binding site. Brain Res. 2002, 944, 165–173.
- Chen, J.; Graham, S.; Moroni, F.; Simon, R. A Study of the Dose Dependency of a Glycine Receptor Antagonist in Focal lschemia. J. Pharmacol. Exp. Ther. 1993, 267, 937–941.
- Nichols, A.C.; Yielding, K.L. Anticonvulsant activity of 4-urea-5,7-dichlorokynurenic acid derivatives that are antagonists at the NMDA-associated glycine binding site. Mol. Chem. Neuropathol. 1998, 35, 1–12.
- Tabakoff, B. Method for Treating Chronic Pain. WO/2007/044682, 6 August 2007.
- Battaglia, G.; Russa, M.L.; Bruno, V.; Arenare, L.; Ippolito, R.; Copani, A.; Bonina, F.; Nicoletti, F. Systemically administered D-glucose conjugates of 7-chlorokynurenic acid are centrally available and exert anticonvulsant activity in rodents. Brain Res 2000, 860, 149–156.
- Füvesi, J.; Somlai, C.; Németh, H.; Varga, H.; Kis, Z.; Farkas, T.; Károly, N.; Dobszay, M.; Penke-Verdier, Z.S.; Penke, B.; et al. Comparative study on the effects of kynurenic acid and glucosamine- kynurenic acid. Pharmacol. Biochem. Behav. 2004, 77, 95–102.
- Zádori, D.; Nyiri, G.; Szonyi, A.; Szatmári, I.; Fülöp, F.; Toldi, J.; Freund, T.F.; Vécsei, L.; Klivényi, P. Neuroprotective effects of a novel kynurenic acid analogue in a transgenic mouse model of Huntington’s disease. J. Neural Transm. 2011, 118, 865–875.
- Marosi, M.; Nagy, D.; Farkas, T.; Kis, Z.; Rózsa, E.; Robotka, H.; Fülöp, F.; Vécsei, L.; Toldi, J. A novel kynurenic acid analogue: A comparison with kynurenic acid. An in vitro electrophysiological study. J. Neural Transm. (Vienna) 2009, 117, 183–188.
- Teleanu, D.M.; Chircov, C.; Grumezescu, A.M.; Volceanov, A.; Teleanu, R.I. Blood-Brain Delivery Methods Using Nanotechnology. Pharmaceutics 2018, 10, 269.
- Rossi, F.; Miggiano, R.; Ferraris, D.M.; Rizzi, M. The Synthesis of Kynurenic Acid in Mammals: An Updated Kynurenine Aminotransferase Structural KATalogue. Front. Mol. Biosci. 2019, 6, 7.
- Di Salvo, M.L.; Safo, M.K.; Contestabile, R. Biomedical aspects of pyridoxal 5’-phosphate availability. Front. Biosci. (Elite Ed) 2012, 4, 897–913.
- Parra, M.; Stahl, S.; Hellmann, H. Vitamin B6 and Its Role in Cell Metabolism and Physiology. Cells 2018, 7, 84.
- Porter, K.; Hoey, L.; Hughes, C.F.; Ward, M.; McNulty, H. Causes, Consequences and Public Health Implications of Low B-Vitamin Status in Ageing. Nutrients 2016, 8, 725.
- Hughes, C.F.; Ward, M.; Tracey, F.; Hoey, L.; Molloy, A.M.; Pentieva, K.; McNulty, H. B-Vitamin Intake and Biomarker Status in Relation to Cognitive Decline in Healthy Older Adults in a 4-Year Follow-Up Study. Nutrients 2017, 9, 53.
- Ford, A.H.; Almeida, O.P. Effect of Vitamin B Supplementation on Cognitive Function in the Elderly: A Systematic Review and Meta-Analysis. Drugs Aging 2019, 36, 419–434.
- Smith, A.D.; Refsum, H.; Bottiglieri, T.; Fenech, M.; Hooshmand, B.; McCaddon, A.; Miller, J.W.; Rosenberg, I.H.; Obeidi, R. Homocysteine and Dementia: An International Consensus Statement. J. Alzheimers Dis. 2018, 62, 561–570.
- Nye, C.; Brice, A. Combined vitamin B6-magnesium treatment in autism spectrum disorder. Cochrane Database Syst. Rev. 2005, 4, CD003497.
- Ishii, K.; Ogaya, T.; Song, Z.; Iizuka, H.; Fukushima, T. Changes in the plasma concentrations of D-kynurenine and kynurenic acid in rats after intraperitoneal administration of tryptophan enantiomers. Chirality 2010, 22, 901–906.
- Bartolini, B.; Corniello, C.; Sella, A.; Somma, F.; Politi, V. The enol tautomer of indole-3-pyruvic acid as a biological switch in stress responses. Adv. Exp. Med. Biol. 2003, 527, 601–608.
- Hardeland, R. Melatonin and other tryptophan metabolites: Rhythms outside the animal world and some novel, presumably universal pathways. In Comparative Aspects of Circadian Rhythms; Fanjul-Moles, M.L., Ed.; Rans World Research Network: Kerala, India, 2008; pp. 1–17.
- Zsizsik, B.K.; Hardeland, R. Formation of kynurenic and xanthurenic acids from kynurenine and 3-hydroxykynurenine in the dinoflagellate Lingulodinium polyedrum: Role of a novel, oxidative pathway. Comp. Biochem. Physiol. C Toxicol. Pharmacol. 2002, 133, 383–392.
- Blanco Ayala, T.; Lugo Huitrón, R.; Carmona Aparicio, L.; Ramírez Ortega, D.; González Esquivel, D.; Pedraza Chaverrí, J.; Pérez de la Cruz, G.; Ríos, C.; Schwarcz, R.; Pérez de la Cruz, V. Alternative kynurenic acid synthesis routes studied in the rat cerebellum. Front. Cell Neurosci. 2015, 9, 178.
- Ramos-Chávez, L.A.; Lugo Huitrón, R.; González Esquivel, D.; Pineda, B.; Ríos, C.; Silva-Adaya, D.; Sánchez-Chapul, L.; Roldán-Roldán, G.; Pérez de la Cruz, V. Relevance of Alternative Routes of Kynurenic Acid Production in the Brain. Oxid. Med. Cell Longev. 2018, 2018, 5272741.
- Mothet, J.P.; Parent, A.T.; Wolosker, H.; Brady, R.O., Jr.; Linden, D.J.; Ferris, C.D.; Rogawski, M.A.; Snyder, S.H. D-Serine is an endogenous ligand for the glycine site of the N-methyl-D-aspartate receptor. Proc. Natl. Acad. Sci. USA 2000, 97, 4926–4931.
- Bastings, J.J.A.J.; van Eijk, H.M.; Olde Damink, S.W.; Rensen, S.S. D-Amino Acids in Health and Disease: A Focus on Cancer. Nutrients 2019, 11, 2205.
- Loh, H.H.; Berg, C.P. Production of D-kynurenine and other metabolites from D-tryptophan by the intact rabbit and by rabbit tissue. J Nutr 1971, 101, 465–475.
- Mason, M.; Berg, C.P. The metabolism of D- and L-tryptophan and D- and L-kynurenine by liver and kidney preparations. J. Biol. Chem. 1952, 195, 515–524.
- Fukushima, T.; Sone, Y.; Mitsuhashi, S.; Tomiya, M.; Toyo’oka, T. Alteration of kynurenic acid concentration in rat plasma following optically pure kynurenine administration: A comparative study between enantiomers. Chirality 2009, 21, 468–472.
- Wang, X.D.; Notarangelo, F.M.; Wang, J.Z.; Schwarcz, R. Kynurenic acid and 3-hydroxykynurenine production from D-kynurenine in mice. Brain Res. 2012, 1455, 1–9.
- Notarangelo, F.M.; Wang, X.D.; Horning, K.J.; Schwarcz, R. Role of D-amino acid oxidase in the production of kynurenine pathway metabolites from d-tryptophan in mice. J. Neurochem. 2016, 136, 804–814.




