Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Rina Fajri Nuwarda | -- | 4097 | 2022-10-03 06:37:35 | | | |
| 2 | Veysel Kayser | + 35 word(s) | 4132 | 2022-10-03 06:48:09 | | | | |
| 3 | Camila Xu | -35 word(s) | 4097 | 2022-10-08 03:37:30 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Nuwarda, R.F.; Ramzan, I.; Weekes, L.; Kayser, V. Vaccine Hesitancy. Encyclopedia. Available online: https://encyclopedia.pub/entry/28225 (accessed on 07 February 2026).
Nuwarda RF, Ramzan I, Weekes L, Kayser V. Vaccine Hesitancy. Encyclopedia. Available at: https://encyclopedia.pub/entry/28225. Accessed February 07, 2026.
Nuwarda, Rina Fajri, Iqbal Ramzan, Lynn Weekes, Veysel Kayser. "Vaccine Hesitancy" Encyclopedia, https://encyclopedia.pub/entry/28225 (accessed February 07, 2026).
Nuwarda, R.F., Ramzan, I., Weekes, L., & Kayser, V. (2022, October 03). Vaccine Hesitancy. In Encyclopedia. https://encyclopedia.pub/entry/28225
Nuwarda, Rina Fajri, et al. "Vaccine Hesitancy." Encyclopedia. Web. 03 October, 2022.
Copy Citation
Vaccination, despite being recognized as one of the most effective primary public health measures, is viewed as unsafe and unnecessary by an increasing number of individuals. Vaccination is one of the most significant public health achievements, having contributed to the eradication of smallpox and the control of many infectious diseases such as rubella, diphtheria, and polio globally.
vaccines
vaccine hesitancy
anti-vaccine movement
1. Definition and Theoretical Framework
Vaccination is one of the most significant public health achievements, having contributed to the eradication of smallpox and the control of many infectious diseases such as rubella, diphtheria, and polio globally. For many diseases, the success of this strategy is dependent on public acceptance of vaccination. While vaccination has been shown to be very effective in reducing the global burden of infectious diseases and deaths associated with vaccine-preventable diseases, concerns that undermine public trust and the acceptance of vaccines continue. If such confidence continues, there is a risk of the resurgence of vaccine-preventable diseases because of delays, rejections, and disruptions to vaccine development, delivery, availability, and further research [1][2][3].
The prevalence of vaccine hesitancy over several decades has led to it being listed as one of the top 10 global health threats by the World Health Organization (WHO) in 2019 [3][4]. In 2014, the WHO’s Strategic Advisory Group of Experts on Immunization (SAGE) defined vaccine hesitancy as: “Vaccine hesitancy refers to delay in acceptance or refusal of vaccines despite availability of vaccination services. Vaccine hesitancy is complex and context-specific, varying across time, place, and vaccines. It is influenced by factors such as complacency, convenience, and confidence” [5][6]. During the last decade, an important amount of research has been conducted regarding vaccine hesitance and the multiple factors influencing an individual’s decision to accept or not accept a vaccine. In this regard, the WHO Strategic Advisory Group of Experts on Immunization (SAGE) proposed three categories to study these factors: complacency (not viewing diseases as high-risk and vaccination as important), convenience (practical hurdles), and confidence (a lack of trust in vaccine safety and effectiveness), referred to as the 3Cs model. The concept of vaccine hesitancy does not apply in situations where vaccine uptake is low due to the unavailability of vaccines, lack of access to vaccines, unacceptable travel/distance to immunization clinics, and poor communication [5]. In 2016, a broader nomenclature spanning the dimensions of access, affordability, awareness, acceptance, and activation was suggested for the vaccine uptake determining factors, known as the 5As [7]. Based on both empirical and theoretical research, the 3Cs model was revised in 2018, emphasizing the importance of more than just the concept of confidence, and emerged as the 5Cs model: confidence, complacency, constraints (adjustment of the term convenience to now include both structural and psychological barriers), calculation (preference for deliberation), and collective responsibility (communal orientation) [8]. Figure 1 shows the adjustment of the vaccine hesitancy model from 3Cs to 5Cs.
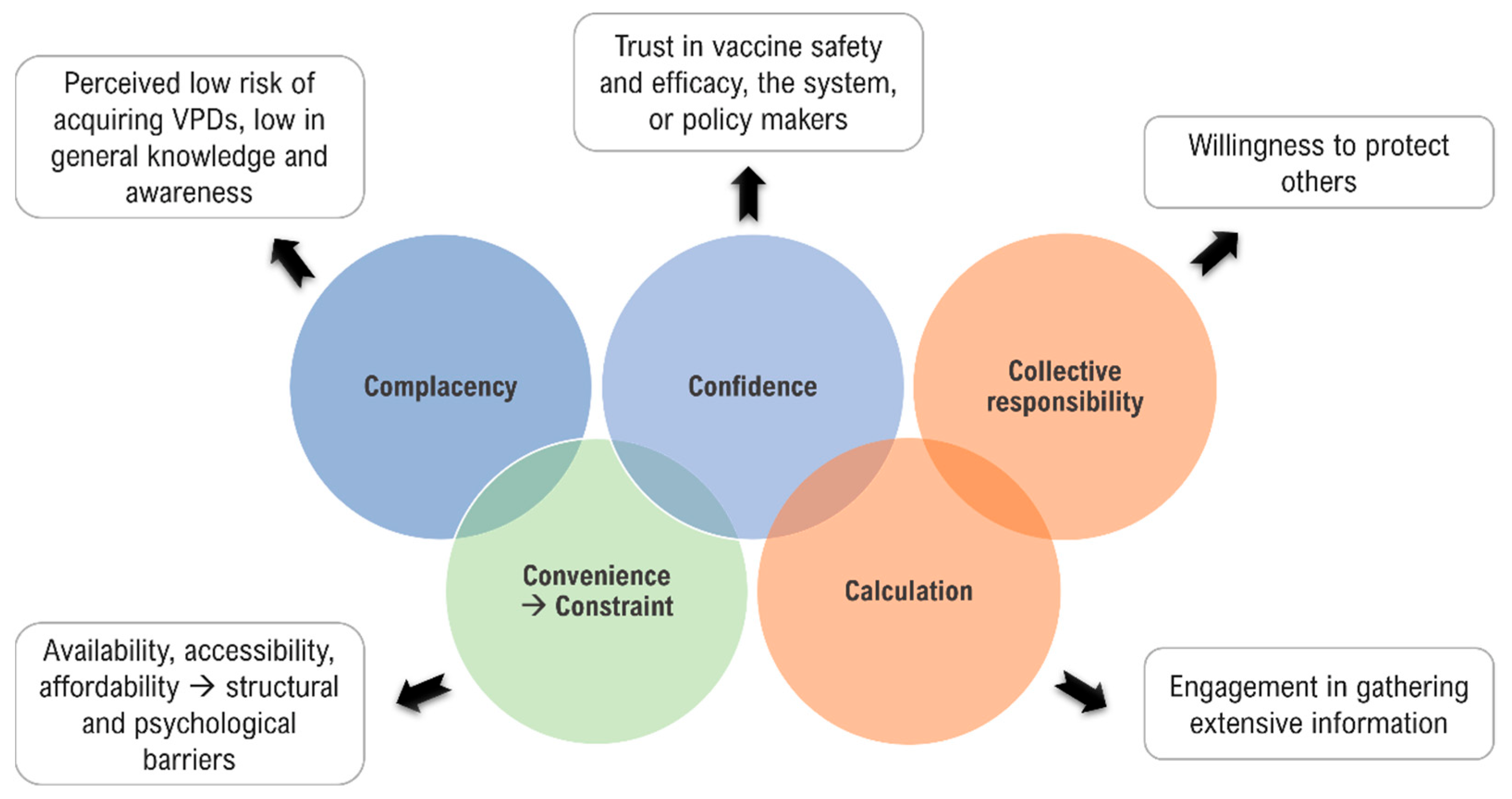
Figure 1. Vaccine hesitancy model: the 3Cs to 5Cs. In 2014, the WHO’s SAGE group determined factors that could influence vaccine hesitancy as the 3Cs: complacency, confidence, and convenience. The 3Cs model was revised in 2018 and became the 5Cs model, replacing convenience with constraint and adding calculation and collective responsibility (figure is adapted from text in reference [9]).
While the SAGE concept was recognized, the reasons for vaccine hesitancy were more complex and varied, with some focused on community issues and others on the systems and health practitioners. A lack of validated surveys assessing hesitation in low- and middle-income countries was another key finding. Therefore, the WHO, UNICEF, and partners formed a working group focused on behavioral and social drivers of vaccination. They developed and validated survey techniques to assess vaccine hesitancy in high-, middle-, and low-income countries. This working group created a behavioral and social driver framework with four components: thinking and feeling (perceived disease risk and vaccine confidence), social processes (social norms and provider recommendation), motivation (intention to obtain recommended vaccines), and practical issues (availability, affordability, ease of access, service quality, and respect from provider). The Royal Society of Canada (RSC) Task Force on COVID-19 sub-group on vaccine acceptance established a more comprehensive model that emphasized the complexity, interconnectedness, and diverse range of factor categories. This adapted framework focused on four primary domains that drove vaccine uptake, including trust in vaccines (people and communities, healthcare workers (HCWs), accurate and trustworthy vaccination knowledge, and the healthcare system and public health programs) [9].
As the WHO has recognized, vaccine hesitancy is one of the most serious threats to global health. Vaccine hesitancy can lead to the failure of either establishing or maintaining the longevity of herd immunity, which is the requirement for the vaccination of a large proportion of the total population. The main concern with vaccine hesitancy and insufficient herd immunity is that unvaccinated individuals can act as virus reservoirs. They can cause more outbreaks, delaying efforts to control the spread of a virus to the entire population [10]. Upon achieving herd immunity through safe and efficient vaccines, diseases become less prevalent. Additionally, achieving herd immunity also aims to keep vulnerable individuals who cannot be vaccinated (e.g., due to health issues such as vaccine allergies) safe and protected against diseases. Individuals can also be left vulnerable to infections (such as tetanus or shingles), for which no herd immunity exists [11]. The percentage of individuals who need to be immunized against diseases to achieve herd immunity varies with the disease; herd immunity for measles requires the vaccination of ~95% of a population, while, for polio, the threshold is ~80% [12].
2. Early Vaccine Hesitancy
Resistance to vaccination is not a recent occurrence. Since the first smallpox vaccine was developed by Edward Jenner in 1796, skepticism and suspicions about vaccines and the motivations behind their use have existed [13].
While Jenner is recognized as contributing to immunization and the eventual eradication of smallpox, variolation was practiced prior to his discovery. However, variolization during early times was neither safe nor consistent; poorly trained practitioners could misdiagnose a donor’s chickenpox lesions as smallpox lesions and there were concerns that recipients would catch disseminated smallpox, infect others or contract diseases such as syphilis [14].
Inoculation was initiated in America during the smallpox epidemic, which hit Boston and other parts of Massachusetts in 1721 [14]. Fatality rates of 2% in variolated versus 14.9% for those infected naturally were reported [15][16]. However, English doctors questioned the extent and longevity of this effect [14].
Edward Jenner advocated for using the milder cowpox virus in a child to stimulate an immune response in 1796 after observing that milkmaids rarely contracted smallpox. Jenner tested his hypothesis on his gardener’s son [17] and, subsequently, on 23 more individuals [18]. In 1797, he presented his experiment to the Royal Society, who rejected it, citing insufficient evidence and the revolutionary nature of his results.
Jenner’s eventual publication of the results drew immediate public criticism and significant opposition. The local clergy argued that mixing animal matter with human flesh was a direct violation of God’s will. Others expressed concerns that the vaccine would cause “Cow-Mania”, using illustrations of an ox-faced boy and an elderly lady who allegedly grew horns after being vaccinated [19].
The 1853, the British Compulsory Vaccination Act announced the smallpox vaccine to be mandatory for infants during their first 3 months of life, creating the world’s first mandatory vaccination program and sparking widespread resistance; riots broke out in several UK towns [20]. The 1867, the act prescribed the mandatory vaccination age to 14 years, with penalties for non-compliance. Opponents of the 1867 law cited concerns about personal freedom and choice, and, in response, the Anti-Compulsory Vaccination League was founded the same year in London.
Numerous anti-vaccination publications emerged in the 1870s and 1880s, and anti-vaccination movements started to appear across Europe. By 1872, vaccination rates in Stockholm had fallen to ~40%, compared to ~90% in the rest of Sweden. However, a major smallpox epidemic occurred in 1874 and a greater uptake of vaccination avoided a further epidemic [21][22].
Anti-vaccination sentiments also grew in the United States (US) towards the end of the 19th century. Anti-vaccination movements arose as states attempted to enforce or pass new vaccination laws. Anti-vaccination societies sprung up around the USA and activists succeeded in repealing mandatory vaccination laws in various states [21][22].
When smallpox hit Cambridge, Massachusetts, in 1902, the city’s health board mandated all adults to be vaccinated. In 1905, during Jacobson v Massachusetts, where a citizen challenged the state’s authority to restrict personal freedom for public health reasons, the US Supreme Court ruled that the state may be justified in restricting individual liberty under the pressure of great dangers to ensure public safety [23].
3. Vaccine Hesitancy and Anti-Vaccine Movement(s) in the Modern Era
Between 1920 and 1970, new vaccines for tuberculosis, yellow fever, whooping cough, tetanus, and polio were introduced, dramatically lowering childhood mortality. Polio, which either paralyzed and/or killed children, was a major public health focus in the 1950s. Significant declines in polio following the introduction of the Salk vaccine in 1954 bolstered public acceptance of vaccines in general [24][25]. However, since the beginning of vaccines being marketed, public concerns about their efficacy and overall safety have existed.
3.1. Polio Vaccine: The Cutter Incident and Simian Virus 40 (SV40)
Following the introduction of the polio vaccine, one of the worst catastrophes occurred in the US. In 1955, despite successful mandatory safety testing, several batches distributed to the public contained the active polio virus. Over 250 cases of polio were linked to Salk’s vaccine manufactured by a small, family-owned company (Cutter Laboratories) [26]. Several vaccine lots were released that did not contain a fully inactivated polio virus, but instead included a live, active polio virus. One hundred and twenty thousand children received this vaccine with active polio viruses; seventy thousand children contracted mild polio from the vaccine, two hundred became permanently disabled, and ten died. This Cutter incident provided the groundwork for distrust in the pharmaceutical industry [27]. While the vaccine was recalled, this incident changed the way vaccines were manufactured and regulated [26].
Another concern surfaced between 1955 and 1963, when it was estimated that 10–30% of polio vaccines in the US were contaminated with SV40, suspected to cause human cancers. This virus was present in monkey kidney cell cultures, used to produce polio vaccines at the time. Following this contamination, the testing of all new polio vaccine lots to ensure that they were free of SV40 was mandated. No vaccines are used currently that include the SV40 virus, although a direct link between contaminated polio vaccines and cancer was never demonstrated [26].
3.2. Swine Flu Vaccine and Guillain-Barré Syndrome (GBS)
In 1976, in response to a potential influenza pandemic, a campaign to encourage vaccination against swine flu was launched. Over 45 million individuals received the vaccine, and there was a slight increase in GBS cases (one additional GBS case per 100,000 individuals vaccinated) [28].
Subsequent research yielded inconsistent results: from no proven link [29][30][31] to a risk of one additional GBS case per million vaccinated persons [32][33]. This information is publicly available and included in the recommendations of the Centers for Disease Control and Prevention (CDC) for influenza vaccines [34]. An elevated risk of GBS following influenza infection, several times more than the risk following influenza vaccination, has been reported [35]. GBS complications from vaccinations are extremely rare, highlighting that education programs are required to assist individuals to appropriately assess the benefits of vaccination versus risks of potential harms [36].
3.3. The Diphtheria, Tetanus, and Pertussis (DTP) Vaccine Controversy
In the mid-1970s, there was controversy over the safety of the diphtheria, tetanus, and pertussis (DTP) vaccination program. After being used for more than 20 years, in 1974, a retrospective study was published which described 36 children who suffered severe neurological complications with DTP [37]. Tragic stories of profoundly retarded children allegedly harmed by the vaccine were dramatized in the media, and concerned parents formed the Association of Parents of Vaccine-Damaged Children (APVDC). The independent Joint Commission on Vaccination and Immunization (JCVI) launched the National Childhood Encephalopathy Study (NCES) to determine whether vaccination was associated with an increased risk of encephalopathy. The JCVI concluded that the risk was extremely low, but negative public sentiment and uncertainty within the medical profession led to a rapid decline in the immunization rate; shortly after, the first of three major epidemics of whooping cough broke out in the UK [38].
A second controversy with DTP vaccines arose in the US in 1982, and public opinion began to shift following an NBC documentary titled DPT: Vaccine Roulette and a book called A Shot in the Dark [39]. The documentary alleged that children exhibited seizures and permanent brain damage from the vaccine [25]. Seizures were a rare adverse reaction to the vaccine, but no long-term effects had been demonstrated. However, the documentary distorted research results to attack the vaccine’s safety, resulting in decreased vaccination rates and lawsuits against vaccine manufacturers. These controversies resulted in a decline in pertussis vaccine uptake in the UK from 81% in 1974 to 31% in 1980, leading to an outbreak of pertussis in the UK, which placed significant strain and pressure on the National Health System [40]. The Academy of Pediatrics and the CDC continued to advocate for vaccination, hence, the overall controversy and public outcry had less impact on immunization rates in the US compared with in the UK. In response, the National Childhood Vaccine Injury Act of 1986 was passed so that vaccine-related injury claims could be filed while protecting vaccine manufacturers [25][40]. The National Vaccine Injury Compensation Program (NVICP) was also established by the US Department of Health and Human Services (DHHS) in 1988, requiring individuals alleging harm from a covered vaccine to first file a claim with the US Court of Federal Claims [41].
3.4. The Measles, Mumps, and Rubella (MMR) Vaccine Controversy
In 1998, Andrew Wakefield, a British gastroenterologist, and his colleagues published a report in The Lancet, alleging that the MMR vaccine caused autism in 12 children [42]. Despite the small case numbers and lack of supportive laboratory evidence, it sparked widespread media coverage, leading to a drop in MMR vaccination [43]. Large epidemiological studies over the following decade consistently found no evidence of a link between the MMR vaccine and autism [44][45][46]. Wakefield’s findings have never been replicated and, in 2004, he refused to join 10 of his co-authors in retracting the paper [47].
In 2010, The Lancet retracted the paper citing several inconsistencies. The UK’s General Medical Council (GMC) found that Wakefield’s subjects were carefully chosen, and some of Wakefield’s research was funded by lawyers for parents involved in lawsuits against vaccine manufacturers, revealing serious conflicts of interest [48].
In 1998, Wakefield highlighted that the MMR vaccine might be directly linked to inflammatory bowel disease and the subsequent development of autism in young children, and he believed that giving children only one dose of measles, mumps, and rubella may be safer [49]. Even as Wakefield sowed such fear, he was well aware that his own laboratory had refuted his central hypothesis that the measles virus caused bowel disease and autism [50]. Wakefield also filed patent applications with the London Patent Office nine months earlier for a new single measles vaccine, as well as various treatments and even “cures” for inflammatory bowel disease and autism. Scientists unanimously concluded that his ideas and suggested remedies lacked scientific credibility [49]. In 2006, The Sunday Times reported that Wakefield had been paid approximately half a million GBP by British litigation lawyers trying to establish that vaccination was harmful, with the hidden payments beginning two years prior to The Lancet paper [51].
In 2008, measles was declared endemic in England and Wales for the first time in 14 years. The UK’s Health Protection Agency linked this outbreak to a drop in MMR vaccination rates [52]. Wakefield’s personal campaign continued, going beyond initial MMR vaccines to criticizing the CDC in his controversial film Vaxxed [53]. Wakefield’s anti-vaccine stance is believed to have contributed to the 2015 California measles outbreak, infecting more than 130 individuals, as well as the 2017 outbreak in Minnesota [54].
3.5. Thiomersal Controversy
Thiomersal, used as a preservative in some vaccines, has also been at the center of the vaccination–autism controversy since the 1990s due to its mercury content [55]. The first serious concerns about its safety arose in the 1970s, as individuals became more aware of the dangers of organic mercury poisoning. The toxicity of ethylmercury used in thiomersal compared with methylmercury (the chemical linked to poisonings), which varies by one methyl side chain, is significantly lower. While the more toxic methylmercury is an industrial pollutant and can be found in fish, ethylmercury has been condemned by association despite the consensus view that it is safe when used in low concentrations [55].
Thiomersal is used in concentrations from 0.003% to 0.01% as a vaccine preservative [56]. In infants, the administration of vaccines containing thiomersal does not elevate mercury blood levels above safe levels [57]. Although there was no evidence that low thiomersal doses in vaccines caused any harm or for their supposed link with autism, in the US in 1999, the Public Health Service, the American Academy of Pediatrics, and vaccine manufacturers agreed that, as a precaution, thiomersal should be reduced or eliminated from vaccines. They also urged physicians to postpone the birth dose of hepatitis B vaccines in children not at risk of contracting the disease [58]. The decision to remove thiomersal sent mixed messages about vaccine safety; it also confused medical professionals and frightened parents, who then assumed that thiomersal was being targeted because it was harmful, breaking their trust in vaccine regulation. In 2000, parents formed several advocacy groups, believing that thiomersal was to blame for their children’s autism. Politicians also used the thiomersal controversy for political gain; in 2004, California governor, Arnold Schwarzenegger, prohibited thiomersal-containing influenza vaccines; other states, including Delaware, Illinois, Missouri, New York, and Washington, soon followed [59][60]. In the US, thiomersal was removed from all childhood vaccines by 2001, with the exception of the flu vaccine, which requires preservation as it is available in multi-dose vials [55].
The timeline of vaccine skepticism, from the early discoveries of vaccines to the controversies that surround vaccination in the modern era was depicted in Figure 2.
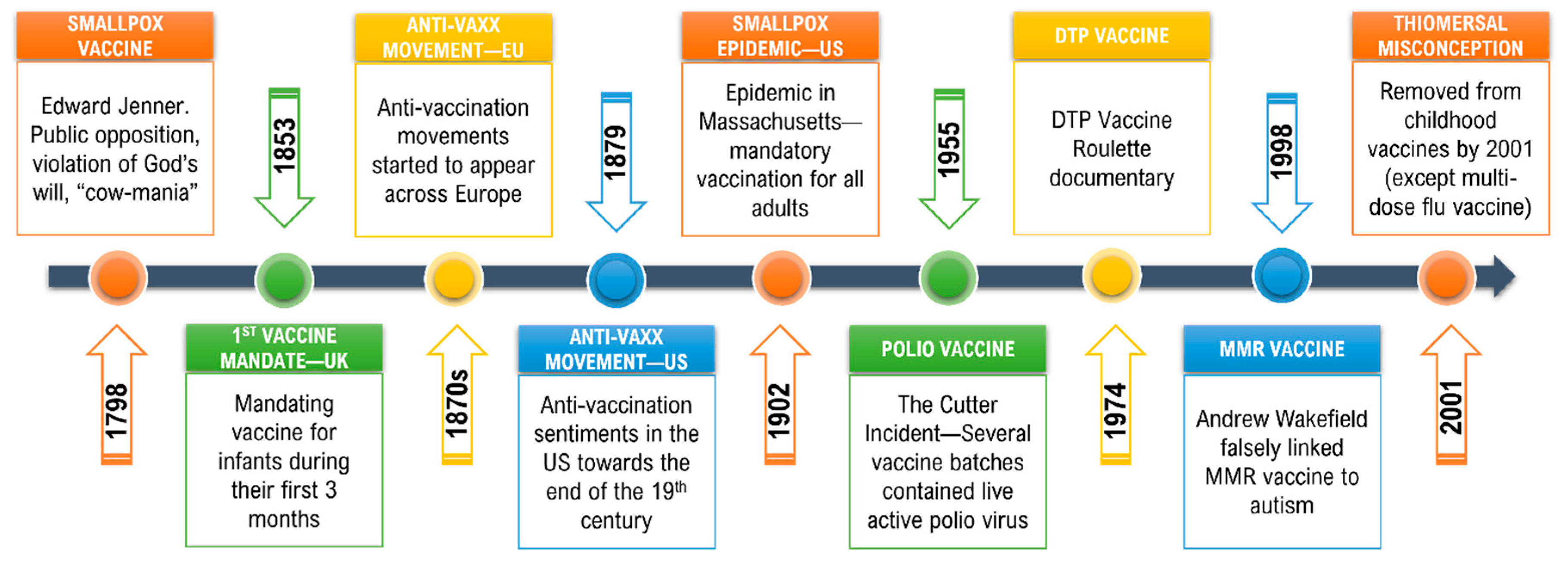
Figure 2. Vaccine hesitancy timeline: early hesitancy and modern controversies. Vaccination resistance existed since the discovery of vaccines, and public trust in their efficacy and overall safety has been challenged by various controversies up until the modern era.
4. Drivers of Vaccine Hesitancy
Decision making about vaccines and vaccination programs at a personal or populational level is complex, with a wide range of socio-demographic, attitudinal, and knowledge-based factors being important [61][62]. Attitudinal factors, such as one’s cultural and religious beliefs, the perception of risk or harm, and the behaviors of oneself and others, play critical and interconnected roles in decision making. Prior vaccine behavior and the impacts of vaccine mandates are additional factors that can predict vaccine uptake. COVID-19 vaccination has been specifically connected to political affiliation, ideological and partisan factors, information (including mis-information and dis-information), and satisfaction with government decision making on other aspects of COVID-19 prevention strategies and/or management [63].
4.1. Heuristics and Vaccine Hesitancy
The role of cognitive biases in human decision making is a key element that needs consideration. Individuals use heuristics to simplify specific problems when determining decisions [64]. A heuristic is a mental shortcut that allows people to solve issues and determine intuitive decisions rapidly [65]. If the correct variables initiate these heuristics, they can be quite useful. When a heuristic approach is employed while under the influence of wrong circumstances, it leads to systemic errors or cognitive biases in decision making [64].
The number of cognitive biases that affect vaccine hesitancy can be categorized into three groups based on the criteria that are common to each group [64]. Group one includes cognitive biases caused by vaccine-related information processing, which are strongly dependent on the message, its content, and pertinent aspects, such as the framing effect, availability bias, and authority bias. Group two involves cognitive biases triggered during vaccination decision making; uncertainty in the vaccine decision-making process, omission bias, risk perception of the decision maker, and ambiguity where there is preference to choose a known risk to an unknown one regardless of the outcome are among several factors that have the greatest influence on individual decisions. Group three cognitive biases have one thing in common: they all have a pre-existing belief about vaccination that has a bigger impact on actions than the content of the information that is available or provided. These examples include shared information bias, belief bias, and the false consensus effect [64].
4.2. Concerns Regarding Vaccine Safety and Efficacy
The success of vaccination programs means that fewer lay individuals and health professionals have first-hand experience or knowledge of the risks of vaccine-preventable diseases (VPDs). Consequently, attention is now often focused on the risk or perceived risk of vaccines or vaccination, rather than on the risk of infectious diseases [66].
The lack of trust in vaccination has been reinforced by several high-profile examples, in particular the paper by Wakefield, which proposed a link between autism and the MMR vaccine [67]. Although the paper was retracted and Wakefield’s findings proven to be flawed, it had long-term impacts on vaccine compliance [67].
Omission bias, the tendency to regard the negative consequences of an action (commission) as being worse than the negative consequences of inaction (omission) even when the latter affects more individuals or occurs more often [68], is suggested to play a role in vaccine hesitancy [69]. Some individuals believe it is more detrimental to vaccinate a child when the vaccination may cause harm than not to vaccinate, despite the fact that vaccination generally reduces the risk of harm [69]. One possible explanation for this decision is that vaccines are administered as preventive measures to healthy individuals; thus, their benefits can only be estimated accurately at the population level, whereas their risks (real or alleged) can be seen at the individual level [66].
4.3. Internet and Social Media Influence
The internet and social media are used to communicate, study, and influence individual and populational decisions regarding vaccines and vaccination. A study analyzed and identified the most common health mis-information issues on social media and found that 43% of mis-information was about vaccines [70]. Those who cite the internet as their primary source of vaccine information are more likely to refuse or delay vaccination [71][72][73]. Social media algorithms are designed to help users by filtering content to reflect an individual’s prior search patterns. It predicts and determines decisions on which material would be best to offer based on one’s prior behavior. As a result, if a person searches or follows sites or individuals that are linked to vaccine hesitancy or refusal, they are more likely to see similar content in their future searches [74]. Additionally, the internet does not determine much distinction between the quality and reliability of information provided by a healthcare expert or a lay person [74]. Hence, the internet and social media platforms have become major channels for the distribution of inaccurate data or mis-information about vaccines and vaccinations, and this is widely exploited [75][76][77][78]. For example, from surveys on social media platforms in the US and UK, it is known that there has been a widespread dissemination of false information about the pandemic, including that 5G mobile networks are linked to the virus, that vaccine trial participants have died after receiving a candidate COVID-19 vaccine, and that the pandemic is a conspiracy or a bio-weapon [79][80][81]. Such information can exacerbate pre-existing anxieties, sowing doubts and cynicisms about new vaccines and threatening the public acceptance of vaccines.
4.4. Mandatory Vaccination and Public Health Policies
Preserving vaccine-acquired herd immunity against an infectious disease requires vaccination coverage above particular threshold values in a population [82]. Vaccination policies vary considerably around the globe; some countries emphasize educating their citizens and allowing individuals to choose, while others mandate immunizations to ensure a high vaccine coverage. A good example for the latter is mandating vaccination in children for a number of diseases as a condition of school entry [83]. Nonetheless, despite being effective, mandatory vaccination policies have long been controversial, widely criticized as an authoritarian measure, and are not accepted by some individuals or in some societies [84].
According to Kennedy et al. [85], a parent’s objection to mandatory vaccination is linked with negative attitudes and views towards the safety and efficacy of vaccines. Additionally, a vaccine mandate induces frequently observed reflections, such as “it is my body, my choice”, as well as widely accepted notions such as “the child’s body can protect itself without vaccination”, referring to a natural immunity being better than the immunity from vaccination. This is only true for some diseases. Disease severity varies among individuals, but some infections, such as rabies, can be fatal in almost all cases. In the absence of lived experience, some parents underestimate the direct threat to their child’s health of contracting VPDs [85]. Another US study by McCoy regarding opposition to vaccine mandates suggested that social factors that form Americans’ opinions about vaccine safety are not the same as the factors that determine their views on whether vaccination should be compulsory. The reason may potentially be due to some conservatives who hold political beliefs that governments should play a limited role and the primacy of individual liberty/freedom [86].
References
- The COCONEL Group. A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. Lancet Infect Dis. 2020, 20, 769–770.
- Dubé, E. Addressing vaccine hesitancy: The crucial role of healthcare providers. Clin. Microbiol. Infect. 2017, 23, 279–280.
- Hou, Z.; Tong, Y.; Du, F.; Lu, L.; Zhao, S.; Yu, K.; Piatek, S.J.; Larson, H.J.; Lin, L. Assessing COVID-19 Vaccine Hesitancy, Confidence, and Public Engagement: A Global Social Listening Study. J. Med. Internet Res. 2021, 23, e27632.
- WHO. Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 1 September 2021).
- WHO. Report of the Strategic Advisory Group of Experts (SAGE) Working Group on Vaccine Hesitancy. Available online: https://www.who.int/immunization/sage/meetings/2014/october/SAGE_working_group_revised_report_vaccine_hesitancy.pdf (accessed on 1 September 2021).
- Wagner, A.L.; Masters, N.B.; Domek, G.J.; Mathew, J.L.; Sun, X.; Asturias, E.J.; Ren, J.; Huang, Z.; Contreras-Roldan, I.L.; Gebremeskel, B.; et al. Comparisons of Vaccine Hesitancy across Five Low- and Middle-Income Countries. Vaccines 2019, 7, 155.
- Thomson, A.; Robinson, K.; Vallée-Tourangeau, G. The 5As: A practical taxonomy for the determinants of vaccine uptake. Vaccine 2016, 34, 1018–1024.
- Betsch, C.; Schmid, P.; Heinemeier, D.; Korn, L.; Holtmann, C.; Böhm, R. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PLoS ONE 2018, 13, e0208601.
- MacDonald, N.E.; Dube, E.; Comeau, J.L. Have vaccine hesitancy models oversimplified a complex problem to our detriment? The Adapted Royal Society of Canada vaccine uptake framework. Vaccine 2022, 40, 3927–3930.
- Dhama, K.; Sharun, K.; Tiwari, R.; Dhawan, M.; Emran, T.B.; Rabaan, A.A.; Alhumaid, S. COVID-19 vaccine hesitancy—Reasons and solutions to achieve a successful global vaccination campaign to tackle the ongoing pandemic. Hum. Vaccines Immunother. 2021, 17, 3495–3499.
- Jacobson, R.M.; St. Sauver, J.L.; Finney Rutten, L.J. Vaccine Hesitancy. Mayo Clin. Proc. 2015, 90, 1562–1568.
- WHO. Coronavirus Disease (COVID-19): Herd Immunity, Lockdowns and COVID-19. Available online: https://www.who.int/news-room/questions-and-answers/item/herd-immunity-lockdowns-and-covid-19 (accessed on 19 January 2022).
- Callender, D. Vaccine hesitancy: More than a movement. Hum. Vaccines Immunother. 2016, 12, 2464–2468.
- Riedel, S. Edward Jenner and the history of smallpox and vaccination. In Baylor University Medical Center Proceedings; Taylor & Francis: Abingdon-on-Thames, UK, 2005; Volume 18, pp. 21–25.
- Best, M.; Neuhauser, D.; Slavin, L. “Cotton Mather, you dog, dam you! I’l inoculate you with this; with a pox to you”: Smallpox inoculation, Boston, 1721. Qual. Saf. Health Care 2004, 13, 82.
- Best, M.; Katamba, A.; Neuhauser, D. Making the right decision: Benjamin Franklin’s son dies of smallpox in 1736. Qual. Saf. Health Care 2007, 16, 478–480.
- Stewart, A.J.; Devlin, P.M. The history of the smallpox vaccine. J. Infect. 2006, 52, 329–334.
- Lantos, J.D.; Jackson, M.A.; Opel, D.J.; Marcuse, E.K.; Myers, A.L.; Connelly, B.L. Controversies in Vaccine Mandates. Curr. Probl. Pediatric Adolesc. Health Care 2010, 40, 38–58.
- Eisen, E.X. “The Mark of the Beast” Georgian Britain’s Anti-Vaxxer Movement. Available online: https://publicdomainreview.org/essay/the-mark-of-the-beast-georgian-britains-anti-vaxxer-movement (accessed on 3 September 2021).
- Durbach, N. ‘They Might As Well Brand Us’: Working-Class Resistance to Compulsory Vaccination in Victorian England. Soc. Hist. Med. 2000, 13, 45–63.
- Prabhu, M. The Long View: Ye Olde Anti-Vaxxers. Available online: https://www.gavi.org/vaccineswork/long-view-ye-olde-anti-vaxxers (accessed on 3 September 2021).
- Grignolio, A.; Rundo, J. Vaccines: Are they Worth a Shot? Springer International Publishing: Berlin, Germany, 2018.
- Mariner, W.K.; Annas, G.J.; Glantz, L.H. Jacobson v Massachusetts: It’s not your great-great-grandfather’s public health law. Am. J. Public Health 2005, 95, 581–590.
- Nature. Nature Milestones in Vaccine. Available online: https://www.nature.com/immersive/d42859-020-00005-8/index.html (accessed on 22 September 2021).
- Pennington, M. Vaccine Hesitancy: A Story as Old as Vaccines Themselves. Available online: https://www.criver.com/eureka/vaccine-hesitancy-story-old-vaccines-themselves (accessed on 22 September 2021).
- CDC. Historical Vaccine Safety Concerns. Available online: https://www.cdc.gov/vaccinesafety/concerns/concerns-history.html (accessed on 22 October 2021).
- Boom, J.A.; Cunningham, R.M. Understanding and Managing Vaccine Concerns; Springer International Publishing: Berlin, Germany, 2014; p. 42.
- CDC. Guillain-Barré Syndrome and Vaccines. Available online: https://www.cdc.gov/vaccinesafety/concerns/guillain-barre-syndrome.html#:~:text=Over%2045%20million%20people%20were,got%20the%20swine%20flu%20vaccine. (accessed on 19 January 2022).
- Wang, D.J.; Boltz, D.A.; McElhaney, J.; McCullers, J.A.; Webby, R.J.; Webster, R.G. No evidence of a link between influenza vaccines and Guillain-Barre syndrome-associated antiganglioside antibodies. Influenza Other Respir. Viruses 2012, 6, 159–166.
- Ghaderi, S.; Gunnes, N.; Bakken, I.J.; Magnus, P.; Trogstad, L.; Håberg, S.E. Risk of Guillain-Barré syndrome after exposure to pandemic influenza A(H1N1)pdm09 vaccination or infection: A Norwegian population-based cohort study. Eur. J. Epidemiol. 2016, 31, 67–72.
- Baxter, R.; Bakshi, N.; Fireman, B.; Lewis, E.; Ray, P.; Vellozzi, C.; Klein, N.P. Lack of association of Guillain-Barré syndrome with vaccinations. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2013, 57, 197–204.
- Juurlink, D.N.; Stukel, T.A.; Kwong, J.; Kopp, A.; McGeer, A.; Upshur, R.E.; Manuel, D.G.; Moineddin, R.; Wilson, K. Guillain-Barré syndrome after influenza vaccination in adults: A population-based study. Arch. Intern. Med. 2006, 166, 2217–2221.
- Lasky, T.; Terracciano, G.J.; Magder, L.; Koski, C.L.; Ballesteros, M.; Nash, D.; Clark, S.; Haber, P.; Stolley, P.D.; Schonberger, L.B.; et al. The Guillain-Barré syndrome and the 1992–1993 and 1993–1994 influenza vaccines. N. Engl. J. Med. 1998, 339, 1797–1802.
- CDC. Vaccine Information Statement: Influenza Vaccine. Available online: https://www.cdc.gov/vaccines/hcp/vis/vis-statements/flu.pdf (accessed on 20 January 2022).
- Vellozzi, C.; Iqbal, S.; Broder, K. Guillain-Barré Syndrome, Influenza, and Influenza Vaccination: The Epidemiologic Evidence. Clin. Infect. Dis. 2014, 58, 1149–1155.
- Babazadeh, A.; Mohseni Afshar, Z.; Javanian, M.; Mohammadnia-Afrouzi, M.; Karkhah, A.; Masrour-Roudsari, J.; Sabbagh, P.; Koppolu, V.; Vasigala, V.K.; Ebrahimpour, S. Influenza Vaccination and Guillain-Barré Syndrome: Reality or Fear. J. Transl. Int. Med. 2019, 7, 137–142.
- Kulenkampff, M.; Schwartzman, J.S.; Wilson, J. Neurological complications of pertussis inoculation. Arch. Dis. Child. 1974, 49, 46–49.
- Baker, J.P. The pertussis vaccine controversy in Great Britain, 1974–1986. Vaccine 2003, 21, 4003–4010.
- Coulter, H.L.; Fisher, B.L. DPT, a Shot in the Dark; Harcourt Brace Jovanovich: New York, NY, USA, 1985.
- Gangarosa, E.J.; Galazka, A.M.; Wolfe, C.R.; Phillips, L.M.; Miller, E.; Chen, R.T.; Gangarosa, R.E. Impact of anti-vaccine movements on pertussis control: The untold story. Lancet 1998, 351, 356–361.
- Vaccine Injury Compensation Programs. Available online: https://www.historyofvaccines.org/content/articles/vaccine-injury-compensation-programs (accessed on 22 October 2021).
- Wakefield, A.J.; Murch, S.H.; Anthony, A.; Linnell, J.; Casson, D.M.; Malik, M.; Berelowitz, M.; Dhillon, A.P.; Thomson, M.A.; Harvey, P.; et al. RETRACTED: Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet 1998, 351, 637–641.
- DeStefano, F.; Chen, R.T. Negative association between MMR and autism. Lancet 1999, 353, 1987–1988.
- Taylor, B.; Miller, E.; Lingam, R.; Andrews, N.; Simmons, A.; Stowe, J. Measles, mumps, and rubella vaccination and bowel problems or developmental regression in children with autism: Population study. BMJ 2002, 324, 393.
- Klein, K.C.; Diehl, E.B. Relationship between MMR vaccine and autism. Ann. Pharmacother. 2004, 38, 1297–1300.
- Madsen, K.M.; Hviid, A.; Vestergaard, M.; Schendel, D.; Wohlfahrt, J.; Thorsen, P.; Olsen, J.; Melbye, M. A Population-Based Study of Measles, Mumps, and Rubella Vaccination and Autism. N. Engl. J. Med. 2002, 347, 1477–1482.
- Godlee, F.; Smith, J.; Marcovitch, H. Wakefield’s article linking MMR vaccine and autism was fraudulent. BMJ 2011, 342, c7452 .
- Eggertson, L. Lancet retracts 12-year-old article linking autism to MMR vaccines. Can. Med. Assoc. J. 2010, 182, E199–E200.
- Berger, A. Dispatches. MMR: What They Didn’t Tell You. BMJ 2004, 329, 1293.
- Brian Deer’s Film on Andrew Wakefield. Available online: https://briandeer.com/wakefield-deer.htm (accessed on 20 January 2022).
- Deer, B. MMR Doctor Given Legal Aid Thousands. Available online: https://web.archive.org/web/20070223155047/http://www.timesonline.co.uk/tol/newspapers/sunday_times/britain/article1265373.ece (accessed on 20 January 2022).
- Ghebrehewet, S.; Hayhurst, G.; Keenan, A.; Moore, H. Outbreak of measles in Central and Eastern Cheshire, UK, October 2008–February 2009. Epidemiol. Infect. 2013, 141, 1849–1856.
- Omer, S.B. The Discredited Doctor Hailed by the Anti-Vaccine Movement. Available online: https://www.nature.com/articles/d41586-020-02989-9 (accessed on 23 September 2021).
- Quick, J.D.; Larson, H. The Vaccine-Autism Myth Started 20 Years Ago. Here’s Why It Still Endures Today. Available online: https://time.com/5175704/andrew-wakefield-vaccine-autism/ (accessed on 23 September 2021).
- Sutherland, A. The Thimerosal Controversy; Virginia Tech: Blacksburg, VI, USA, 2013.
- Targonski, P.V.; Ovsyannikova, I.G.; Tosh, P.K.; Jacobson, R.M.; Poland, G.A. Chapter 91—Vaccines. In Pharmacology and Therapeutics; Waldman, S.A., Terzic, A., Egan, L.J., Elghozi, J.-L., Jahangir, A., Kane, G.C., Kraft, W.K., Lewis, L.D., Morrow, J.D., Zingman, L.V., et al., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2009; pp. 1247–1268.
- FDA. Thimerosal in Vaccines Questions and Answers. Available online: https://www.fda.gov/vaccines-blood-biologics/vaccines/thimerosal-vaccines-questions-and-answers#:~:text=As%20a%20vaccine%20preservative%2C%20thimerosal,mercury%20per%200.5%20mL%20dose (accessed on 20 January 2022).
- CDC. Thimerosal in vaccines: A joint statement of the American Academy of Pediatrics and the Public Health Service. MMWR Morb. Mortal. Wkly. Rep. 1999, 48, 563–565.
- Offit, P.A. Thimerosal and Vaccines—A Cautionary Tale. N. Engl. J. Med. 2007, 357, 1278–1279.
- Dube, N. Mercury-Free Vaccine Legislation in Other States. Available online: https://www.cga.ct.gov/2010/rpt/2010-R-0352.htm (accessed on 20 January 2022).
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J. Strategies for addressing vaccine hesitancy—A systematic review. Vaccine 2015, 33, 4180–4190.
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.D.; Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine 2014, 32, 2150–2159.
- Kennedy, E.B.; Daoust, J.F.; Vikse, J.; Nelson, V. “Until I Know It’s Safe for Me”: The Role of Timing in COVID-19 Vaccine Decision-Making and Vaccine Hesitancy. Vaccines 2021, 9, 1417.
- Azarpanah, H.; Farhadloo, M.; Vahidov, R.; Pilote, L. Vaccine hesitancy: Evidence from an adverse events following immunization database, and the role of cognitive biases. BMC Public Health 2021, 21, 1686.
- Luz, P.M.; Nadanovsky, P.; Leask, J. How heuristics and cognitive biases affect vaccination decisions. Cad. Saude Publica 2020, 36 (Suppl. S2).
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J. Vaccine hesitancy: An overview. Hum. Vaccin. Immunother. 2013, 9, 1763–1773.
- Petrelli, F.; Contratti, C.M.; Tanzi, E.; Grappasonni, I. Vaccine hesitancy, a public health problem. Ann. Ig. 2018, 30, 86–103.
- Spranca, M.; Minsk, E.; Baron, J. Omission and commission in judgment and choice. J. Exp. Soc. Psychol. 1991, 27, 76–105.
- Ritov, I.; Baron, J. Reluctance to vaccinate: Omission bias and ambiguity. J. Behav. Decis. Mak. 1990, 3, 263–277.
- Suarez-Lledo, V.; Alvarez-Galvez, J. Prevalence of Health Misinformation on Social Media: Systematic Review. J. Med. Internet Res. 2021, 23, e17187.
- Brunson, E.K. The Impact of Social Networks on Parents’ Vaccination Decisions. Pediatrics 2013, 131, e1397.
- Betsch, C.; Sachse, K. Jekyll or Mr. Hyde? (How) the Internet influences vaccination decisions: Recent evidence and tentative guidelines for online vaccine communication. Vaccine 2012, 30, 3723–3726.
- Connolly, T.; Reb, J. Toward interactive, Internet-based decision aid for vaccination decisions: Better information alone is not enough. Vaccine 2012, 30, 3813–3818.
- Dubé, È.; Ward, J.K.; Verger, P.; MacDonald, N.E. Vaccine Hesitancy, Acceptance, and Anti-Vaccination: Trends and Future Prospects for Public Health. Annu. Rev. Public Health 2021, 42, 175–191.
- Kata, A. A postmodern Pandora’s box: Anti-vaccination misinformation on the Internet. Vaccine 2010, 28, 1709–1716.
- Ruiz, J.B.; Bell, R.A. Understanding vaccination resistance: Vaccine search term selection bias and the valence of retrieved information. Vaccine 2014, 32, 5776–5780.
- Burki, T. Vaccine misinformation and social media. Lancet Digit. Health 2019, 1, e258–e259.
- Jamison, A.; Broniatowski, D.A.; Smith, M.C.; Parikh, K.S.; Malik, A.; Dredze, M.; Quinn, S.C. Adapting and Extending a Typology to Identify Vaccine Misinformation on Twitter. Am. J. Public Health 2020, 110, S331–S339.
- Loomba, S.; de Figueiredo, A.; Piatek, S.J.; de Graaf, K.; Larson, H.J. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat. Hum. Behav. 2021, 5, 337–348.
- Megget, K. Even COVID-19 can’t kill the anti-vaccination movement. BMJ 2020, 369, m2184.
- Pennycook, G.; McPhetres, J.; Zhang, Y.; Lu, J.G.; Rand, D.G. Fighting COVID-19 Misinformation on Social Media: Experimental Evidence for a Scalable Accuracy-Nudge Intervention. Psychol. Sci. 2020, 31, 770–780.
- Fine, P.; Eames, K.; Heymann, D.L. “Herd immunity”: A rough guide. Clin. Infect. Dis. 2011, 52, 911–916.
- Walkinshaw, E. Mandatory vaccinations: The international landscape. Can. Med. Assoc. J. 2011, 183, E1167–E1168.
- Gualano, M.R.; Olivero, E.; Voglino, G.; Corezzi, M.; Rossello, P.; Vicentini, C.; Bert, F.; Siliquini, R. Knowledge, attitudes and beliefs towards compulsory vaccination: A systematic review. Hum. Vaccines Immunother. 2019, 15, 918–931.
- Kennedy, A.M.; Brown, C.J.; Gust, D.A. Vaccine beliefs of parents who oppose compulsory vaccination. Public Health Rep. 2005, 120, 252–258.
- McCoy, C.A. The social characteristics of Americans opposed to vaccination: Beliefs about vaccine safety versus views of U.S. vaccination policy. Crit. Public Health 2020, 30, 4–15.
More
Information
Subjects:
Infectious Diseases; Others
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.1K
Revisions:
3 times
(View History)
Update Date:
20 Oct 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




