
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Brandon Lucke-Wold | -- | 2373 | 2022-09-29 18:06:10 | | | |
| 2 | Amina Yu | -2 word(s) | 2371 | 2022-09-30 11:06:59 | | |
Video Upload Options
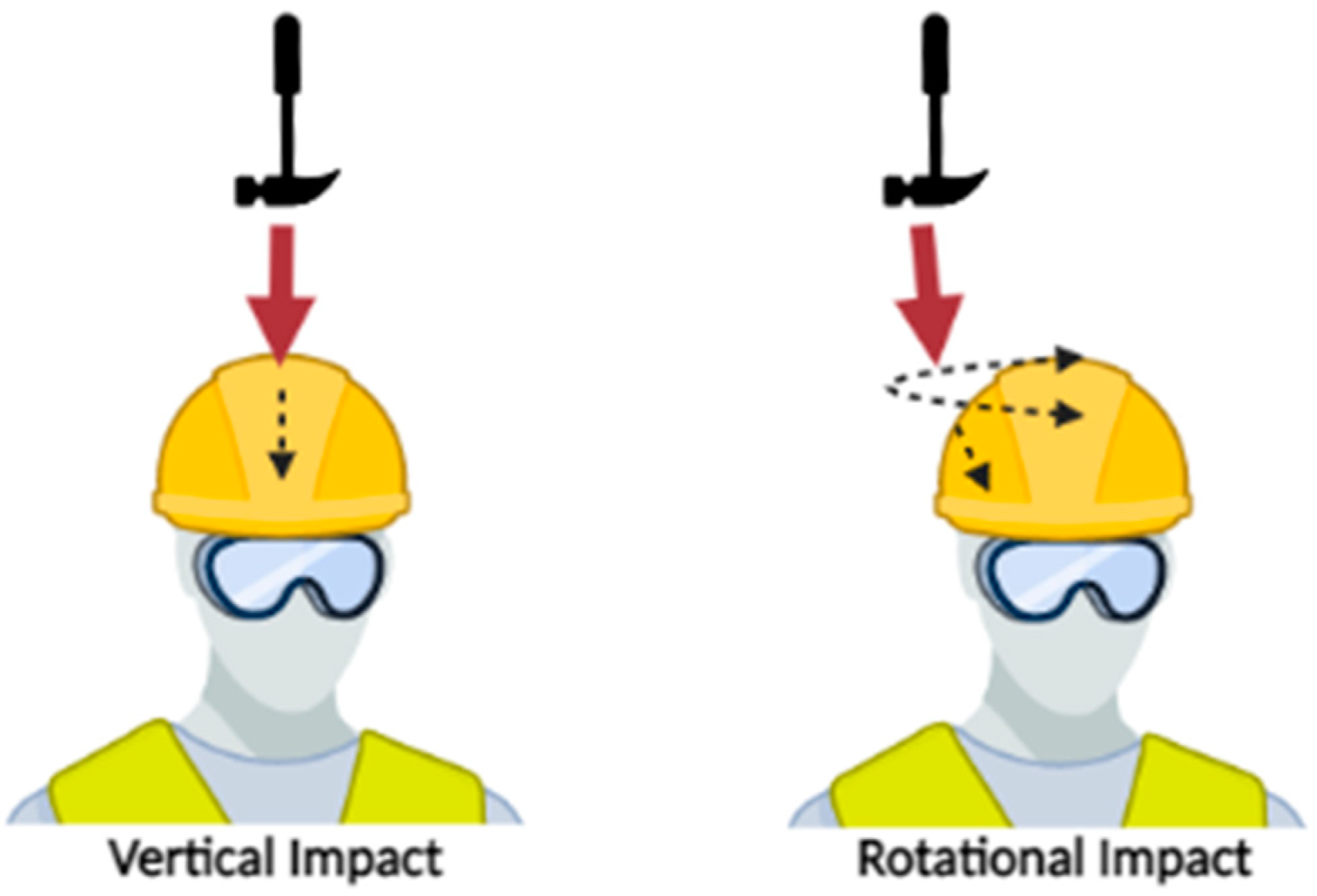
Neurotrauma is an important, often preventable cause of morbidity and mortality. Between 180 and 250 traumatic brain injuries (TBIs) occur per 100,000 population per year in the U.S.. Helmets have been employed by humans for thousands of years and have served as a crucial instrument by which we protect ourselves from and minimize the effects of traumatic brain injury. Substantial evidence from systematic reviews and meta-analyses points toward the protective effectiveness (often >60%) of helmets in preventing TBIs in athletes, cyclists and motorcyclists. However, when stratifying TBI by severity, helmets may be less effective or even ineffective in preventing milder forms of TBI such as concussion. Helmet design has been predicated on linear acceleration as a metric corresponding to head injury. This has served well in preventing catastrophic injuries. However, rotational acceleration is more likely implicated in the pathophysiology of milder brain injuries, including concussion.
1. Current Sports Helmet Design
2. Current Military Helmet Design
3. Current Construction Helmet Design
4. Secondary Injury Prevention
References
- Cantu, R.C. Neurologic Athletic Head and Spine Injuries; W.B. Saunders: Philadelphia, PA, USA, 2000.
- Post, A.; Hoshizaki, T.B. Mechanisms of brain impact injuries and their prediction: A review. Trauma 2012, 14, 327–349.
- Bain, A.C.; Meaney, D.F. Tissue-level thresholds for axonal damage in an experimental model of central nervous system white matter injury. J. Biomech. Eng. 2000, 122, 615–622.
- Rueda, M.A.F.; Cui, L.; Gilchrist, M.D. Finite element modelling of equestrian helmet impacts exposes the need to address rotational kinematics in future helmet designs. Comput. Methods Biomech. Biomed. Eng. 2011, 14, 1021–1031.
- Hoshizaki, T.; Brien, S. The Science and Design of Head Protection in Sport. Neurosurgery 2004, 55, 956–966.
- McIntosh, A.S.; Andersen, T.E.; Bahr, R.; Greenwald, R.; Kleiven, S.; Turner, M.; Varese, M.; McCrory, P. Sports helmets now and in the future. Br. J. Sports Med. 2011, 45, 1258–1265.
- Post, A.; Hoshizaki, T.B.; Brien, S. Head Injuries, Measurement Criteria and Helmet Design. In Routledge Handbook of Ergonomics in Sport and Exercise; Hong, Y., Ed.; Routledge Publishers: London, UK, 2012.
- Hoshizaki, T.B.; Post, A.; Oeur, R.A.; Brien, S.E. Current and Future Concepts in Helmet and Sports Injury Prevention. Neurosurgery 2014, 75, S136–S148.
- Bustamante, M.C.; Bruneau, D.; Barker, J.B.; Gierczycka, D.; Coralles, M.A.; Cronin, D.S. Component-Level Finite Element Model and Validation for a Modern American Football Helmet. J. Dyn. Behav. Mater. 2019, 5, 117–131.
- Tuna, E.B.; Ozel, E. Factors Affecting Sports-Related Orofacial Injuries and the Importance of Mouthguards. Sports Med. 2014, 44, 777–783.
- Ranalli, D.N.; Demas, P.N. Orofacial Injuries from Sport. Sports Med. 2002, 32, 409–418.
- Underwood, L.; Jermy, M.; Eloi, P.; Cornillon, G. Helmet position, ventilation holes and drag in cycling. Sports Eng. 2015, 18, 241–248.
- Gibson, T.J.; Thai, K. Helmet Protection against Basilar Skull Fracture; Australian Transport Safety Bureau: Canberra, Australian, 2007.
- Scharine, A.A.; Binseel, M.S.; Mermagen, T.; Letowski, T.R. Sound localisation ability of soldiers wearing infantry ACH and PASGT helmets. Ergonomics 2014, 57, 1222–1243.
- York, S.; Edwards, E.D.; Jesunathadas, M.; Landry, T.; Piland, S.G.; Plaisted, T.A.; Kleinberger, M.; Gould, T.E. Influence of Friction at the Head-Helmet Interface on Advanced Combat Helmet (ACH) Blunt Impact Kinematic Performance. Mil. Med. 2022, usab547.
- Bradfield, C.; Vavalle, N.; DeVincentis, B.; Wong, E.; Luong, Q.; Voo, L.; Carneal, C. Combat Helmet Suspension System Stiffness Influences Linear Head Acceleration and White Matter Tissue Strains: Implications for Future Helmet Design. Mil. Med. 2018, 183, 276–286.
- Terpsma, R.; Carlsen, R.W.; Szalkowski, R.; Malave, S.; Fawzi, A.L.; Franck, C.; Hovey, C. Head Impact Modeling to Support a Rotational Combat Helmet Drop Test. Mil. Med. 2021, usab374.
- Begonia, M.; Humm, J.; Shah, A.; Pintar, F.A.; Yoganandan, N. Influence of ATD versus PMHS reference sensor inputs on computational brain response in frontal impacts to advanced combat helmet (ACH). Traffic Inj. Prev. 2018, 19, S159–S161.
- Sone, J.Y.; Kondziolka, D.; Huang, J.H.; Samadani, U. Helmet efficacy against concussion and traumatic brain injury: A review. J. Neurosurg. 2017, 126, 768–781.
- Grujicic, M.; Bell, W.C.; Pandurangan, B.; Glomski, P.S. Fluid/Structure Interaction Computational Investigation of Blast-Wave Mitigation Efficacy of the Advanced Combat Helmet. J. Mater. Eng. Perform. 2011, 20, 877–893.
- Zhang, L.; Makwana, R.; Sharma, S. Brain response to primary blast wave using validated finite element models of human head and advanced combat helmet. Front. Neurol. 2013, 4, 88.
- Nyein, M.K.; Jason, A.M.; Yu, L.; Pita, C.M.; Joannopoulos, J.D.; Moore, D.F.; Radovitzky, R.A. In silico investigation of intracranial blast mitigation with relevance to military traumatic brain injury. Proc. Natl. Acad. Sci. USA 2010, 107, 20703–20708.
- Ivins, B.J.; Crowley, J.S.; Johnson, J.; Warden, D.L.; Schwab, K.A. Traumatic brain injury risk while parachuting: Comparison of the personnel armor system for ground troops helmet and the advanced combat helmet. Mil. Med. 2008, 173, 1168–1172.
- Waehrer, G.M.; Dong, X.S.; Millera, T.; Haile, E.; Men, Y. Costs of occupational injuries in construction in the United States. Accid. Anal. Prev. 2007, 39, 1258–1266.
- U.S. Bureau of Labor Statistics. Available online: https://www.bls.gov/ (accessed on 24 July 2022).
- 1926.100—Head Protection. Occupational Safety and Health Administration. Available online: https://www.osha.gov/laws-regs/regulations/standardnumber/1926/1926.100 (accessed on 24 July 2022).
- Long, J.; Yang, J.; Lei, Z.; Liang, D. Simulation-based assessment for construction helmets. Comput. Methods Biomech. Biomed. Eng. 2015, 18, 24–37.
- Hume, A.; Mills, N.J.; Gilchrist, A. Industrial Head Injuries and the Performance of the Helmets. 1995. Available online: https://www.semanticscholar.org/paper/Industrial-head-injuries-and-the-performance-of-Hulme-Mills/03bf8f6afc4729f9529ce630daed14473b11ecb8 (accessed on 24 July 2022).
- Magnuson, S.; Autenrieth, D.A.A.; Stack, T.; Risser, S.; Gilkey, D. Are hard hats a risk factor for WRMSD in the cervical-thoracic region? Work Read. Mass. 2020, 66, 437–443.
- Wu, J.Z.; Pan, C.S.; Wimer, B.M.; Rosen, C.L. Finite element simulations of the head-brain responses to the top impacts of a construction helmet: Effects of the neck and body mass. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2017, 231, 58–68.
- Naresh, P.; Krishnudu, D.M.; Babu, A.H.; Hussain, P. Design And Analysis of Industrial Helmet. Int. J. Mech. Eng. Res. 2015, 5, 81–95.
- Wu, J.Z.; Pan, C.S.; Wimer, B.M. Evaluation of the shock absorption performance of construction helmets under repeated top impacts | Elsevier Enhanced Reader. Eng. Fail. Anal. 2019, 96, 330–339.
- Wei, L.; Cheng, M.; Feng, M.; Lijuan, Z. Research on Recognition of Safety Helmet Wearing of Electric Power Construction Personnel Based on Artificial Intelligence Technology. IOP Sci. 2020, 1684, 012013.
- Kim, S.C.; Ro, Y.S.; Shin, S.D.; Kim, J.Y. Preventive Effects of Safety Helmets on Traumatic Brain Injury after Work-Related Falls. Int. J. Environ. Res. Public Health 2016, 13, 1063.
- Tierney, G. Concussion biomechanics, head acceleration exposure and brain injury criteria in sport: A review. Sports Biomech. 2021, 1–29.
- Kleiven, S. Why Most Traumatic Brain Injuries are Not Caused by Linear Acceleration but Skull Fractures are. Front. Bioeng. Biotechnol. 2013, 1, 15.
- Rowson, S.; Bland, M.L.; Campolettano, E.T.; Press, J.N.; Rowson, B.; Smith, J.A.; Sproule, D.W.; Tyson, A.M.; Duma, S.M. Biomechanical Perspectives on Concussion in Sport. Sports Med. Arthrosc. Rev. 2016, 24, 100–107.
- Trotta, A.; Annaidh, A.N.; Burek, R.O.; Pelgrims, B.; Ivens, J. Evaluation of the head-helmet sliding properties in an impact test. J. Biomech. 2018, 75, 28–34.
- Neice, R.; Plaisted, T. Evaluation of a Combat Helmet Under Combined Translational and Rotational Impact Loading. 2020. Available online: https://apps.dtic.mil/sti/citations/AD1120852 (accessed on 24 July 2022).
- McKeithan, L.; Hibshman, N.; Yengo-Kahn, A.M.; Solomon, G.S.; Zuckerman, S.L. Sport-Related Concussion: Evaluation, Treatment, and Future Directions. Med. Sci. 2019, 7, 44.
- Jamjoom, A.A.B.; Rhodes, J.; Andrews, P.J.D.; Grant, S.G.N. The synapse in traumatic brain injury. Brain 2020, 144, 18–31.
- Pavlovic, D.; Pekic, S.; Stojanovic, M.; Popovic, V. Traumatic brain injury: Neuropathological, neurocognitive and neurobehavioral sequelae. Pituitary 2019, 22, 270–282.
- Romeu-Mejia, R.; Giza, C.C.; Goldman, J.T. Concussion Pathophysiology and Injury Biomechanics. Curr. Rev. Musculoskelet. Med. 2019, 12, 105–116.
- Keating, C.E.; Cullen, D.K. Mechanosensation in traumatic brain injury. Neurobiol. Dis. 2021, 148, 105210.
- Wofford, K.L.; Grovola, M.R.; Adewole, D.O.; Browne, K.D.; Putt, M.E.; O’Donnell, J.C.; Cullen, D.K. Relationships between injury kinematics, neurological recovery, and pathology following concussion. Brain Commun. 2021, 3, fcab268.
- Tehse, J.; Taghibiglou, C. The overlooked aspect of excitotoxicity: Glutamate-independent excitotoxicity in traumatic brain injuries. Eur. J. Neurosci. 2019, 49, 1157–1170.
- Guerriero, R.M.; Giza, C.C.; Rotenberg, A. Glutamate and GABA Imbalance Following Traumatic Brain Injury. Curr. Neurol. Neurosci. Rep. 2015, 15, 27.
- Wofford, K.L.; Loane, D.J.; Cullen, D.K. Acute drivers of neuroinflammation in traumatic brain injury. Neural Regen. Res. 2019, 14, 1481–1489.
- Hubbard, W.B.; Joseph, B.; Spry, M.; Vekaria, H.J.; Saatman, K.E.; Sullivan, P.G. Acute Mitochondrial Impairment Underlies Prolonged Cellular Dysfunction after Repeated Mild Traumatic Brain Injuries. J. Neurotrauma 2019, 36, 1252–1263.
- Cheng, G.; Kong, R.-H.; Zhang, L.-M.; Zhang, J.-N. Mitochondria in traumatic brain injury and mitochondrial-targeted multipotential therapeutic strategies. Br. J. Pharmacol. 2012, 167, 699–719.
- Verweij, B.H.; Muizelaar, J.P.; Vinas, F.C.; Peterson, P.L.; Xiong, Y.; Lee, C.P. Impaired cerebral mitochondrial function after traumatic brain injury in humans. J. Neurosurg. 2000, 93, 815–820.
- Ismail, H.; Shakkour, Z.; Tabet, M.; Abdelhady, S.; Kobaisi, A.; Abedi, R.; Nasrallah, L.; Pintus, G.; Al-Dhaheri, Y.; Mondello, S.; et al. Traumatic Brain Injury: Oxidative Stress and Novel Anti-Oxidants Such as Mitoquinone and Edaravone. Antioxidants 2020, 9, 943.
- Sahel, D.K.; Kaira, M.; Raj, K.; Sharma, S.; Singh, S. Mitochondrial dysfunctioning and neuroinflammation: Recent highlights on the possible mechanisms involved in Traumatic Brain Injury. Neurosci. Lett. 2019, 710, 134347.
- Brady, R.D.; Bird, S.; Sun, M.; Yamakawa, G.R.; Major, B.P.; Mychasiuk, R.; O’Brien, T.J.; McDonald, S.J.; Shultz, S.R. Activation of the Protein Kinase R–Like Endoplasmic Reticulum Kinase (PERK) Pathway of the Unfolded Protein Response after Experimental Traumatic Brain Injury and Treatment with a PERK Inhibitor. Neurotrauma Rep. 2021, 2, 330–342.
- Scheper, W.; Hoozemans, J.J.M. The unfolded protein response in neurodegenerative diseases: A neuropathological perspective. Acta Neuropathol. 2015, 130, 315–331.
- Krishnamurthy, K.; Laskowitz, D.T. Cellular and Molecular Mechanisms of Secondary Neuronal Injury. In Translational Research in Traumatic Brain Injury; Laskowitz, D., Grant, G., Eds.; CRC Press, Taylor and Francis Group: Boca Raton, FL, USA, 2016.
- Hetz, C.; Axten, J.M.; Patterson, J.B. Pharmacological targeting of the unfolded protein response for disease intervention. Nat. Chem. Biol. 2019, 15, 764–775.
- Kim, I.; Xu, W.; Reed, J.C. Cell death and endoplasmic reticulum stress: Disease relevance and therapeutic opportunities. Nat. Rev. Drug Discov. 2008, 7, 1013–1030.




