Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Athanasia Pataka | -- | 2271 | 2022-09-13 20:05:03 | | | |
| 2 | Beatrix Zheng | -42 word(s) | 2229 | 2022-09-14 08:05:18 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Pataka, A.; Kotoulas, S.; Kalamaras, G.; Tzinas, A.; Grigoriou, I.; Kasnaki, N.; Argyropoulou, P. Association between Smoking and Obstructive Sleep Apnea. Encyclopedia. Available online: https://encyclopedia.pub/entry/27144 (accessed on 07 February 2026).
Pataka A, Kotoulas S, Kalamaras G, Tzinas A, Grigoriou I, Kasnaki N, et al. Association between Smoking and Obstructive Sleep Apnea. Encyclopedia. Available at: https://encyclopedia.pub/entry/27144. Accessed February 07, 2026.
Pataka, Athanasia, Seraphim Kotoulas, George Kalamaras, Asterios Tzinas, Ioanna Grigoriou, Nectaria Kasnaki, Paraskevi Argyropoulou. "Association between Smoking and Obstructive Sleep Apnea" Encyclopedia, https://encyclopedia.pub/entry/27144 (accessed February 07, 2026).
Pataka, A., Kotoulas, S., Kalamaras, G., Tzinas, A., Grigoriou, I., Kasnaki, N., & Argyropoulou, P. (2022, September 13). Association between Smoking and Obstructive Sleep Apnea. In Encyclopedia. https://encyclopedia.pub/entry/27144
Pataka, Athanasia, et al. "Association between Smoking and Obstructive Sleep Apnea." Encyclopedia. Web. 13 September, 2022.
Copy Citation
The connection between smoking and Obstructive sleep apnea (OSA) is not yet clear. There are studies that have confirmed the effect of smoking on sleep disordered breathing, whereas others did not. Nicotine affects sleep, as smokers have prolonged total sleep and REM latency, reduced sleep efficiency, total sleep time, and slow wave sleep. Smoking cessation has been related with impaired sleep.
obstructive sleep apnea
smoking
smoking cessation
1. Introduction
Obstructive sleep apnea (OSA) is the most common sleep breathing disorder characterized by recurrent episodes of complete or partial obstruction of the upper airway, resulting in intermittent hypoxia and sleep fragmentation [1]. The main predisposing risk factors of OSA are male gender, older age, genetic and anatomical factors, central obesity, alcohol consumption, and also a narrowed upper airway. OSA is an independent risk factor for cardiovascular and cerebrovascular disease leading to increased morbidity and all-cause mortality [2].
Sleep fragmentation from frequent arousals result to daytime sleepiness, memory loss, and impaired cognitive function contributing to accidents [3]. OSA causes catecholamine surges, low-grade inflammation, and oxidative stress, having as a result cardio-metabolic consequences [4] such as hypertension, stroke, cardiac arrhythmias, and death when left untreated. The gold standard for the diagnosis of OSA is in laboratory polysomnography (PSG). As PSG is not widely available and rather expensive, other alternative diagnostic approaches have been tested as questionnaires, clinical prediction scores, and portable sleep monitors. Several questionnaires have been developed as screening tools for the detection of patients with a high probability of OSA, but none of these instruments achieved the reliability of PSG. Home sleep studies provide benefits in terms of cost and time, but with a lower diagnostic reliability compared with in-laboratory testing. However, in patients with a high probability of OSA and without co-morbidities, home sleep apnea testing is not inferior to in-laboratory PSG. Imagine modalities as lateral cephalometry, endoscopy, computed tomography (CT), or magnetic resonance imaging (MRI) may be useful for identifying the site of upper airway obstruction [4]. Continuous positive airway pressure (CPAP) is often considered the gold standard of OSA treatment; however, adherence to this treatment is often poor [5]. Additional OSA treatments include upper airway surgery, mandibular device therapy, modulation of hypoglossal nerve, pharmacotherapy, and combination therapy [6].
OSA is a heterogeneous disease with different clinical phenotypes and also different underlying pathogenetic mechanisms (endotypes). Several factors may be involved in the pathogenesis of OSA as (a) anatomical compromise resulting in a small, collapsible upper airway, (b) impaired pharyngeal dilator muscle function, (c) unstable oversensitive ventilatory control (elevated loop gain), and (d) low arousal threshold (individuals predisposed to wake up easily with respiratory disturbances). Additionally, the redistribution of body fluid may also be important [7][8][9][10]. Causes of narrowed upper airway anatomy that predispose to the development of OSA include nasal congestion, increased tonsil or adenoid or tongue size, fat deposition around the upper airway due to central obesity, and upper airway edema due to several factors including smoking [11][12][13][14][15][16][17]. The data on the relationship between OSA and smoking still remain controversial, failing to establish a safe conclusion about the association between these two entities [10].
Cigarette smoking is still the leading cause of preventable mortality and is the major contributor of cardiovascular disease. Both smoking and OSA increase the risk of cardiovascular disease as they both induce oxidative stress, endothelial dysfunction, and increase inflammatory response. For that they are associated with significant morbidity and mortality [16]. Further, there is evidence that each of these two conditions adversely affects the other and may lead to increased co-morbidity [15]. The health consequences of cigarette smoking are well documented; however, the effect of smoking cessation on sleep apnea has not been extensively studied.
Targeting anatomy with medical therapy is challenging. Smoking cessation could improve OSA, as it may alleviate upper airways oedema, but studies to support this are limited [15][18]. Additionally, there is some evidence that links untreated OSA with increased smoking addiction [19], implying that the treatment of OSA could help towards a more successful smoking cessation attempt.
2. Mechanisms by Which Smoking Can Result in OSA
Smoking induces chronic inflammation of the upper airway contributing to OSA symptoms [18][20]. Apart from active, passive and former smoking has been related with snoring [12]. There are studies that have confirmed the effect of smoking on sleep disordered breathing [11][12][13][14][15][16][17]. They have found that the prevalence of respiratory events, as sleep apnea or snoring, is higher in smokers, even in passive smokers [11][12][13][14][15][16][17]. Smoking has an impact on OSA through several mechanisms that include enhanced upper airway inflammation, changes of sleep architecture, instability of arousal mechanisms, and alterations of upper airway neuromuscular function [15] (Figure 1).
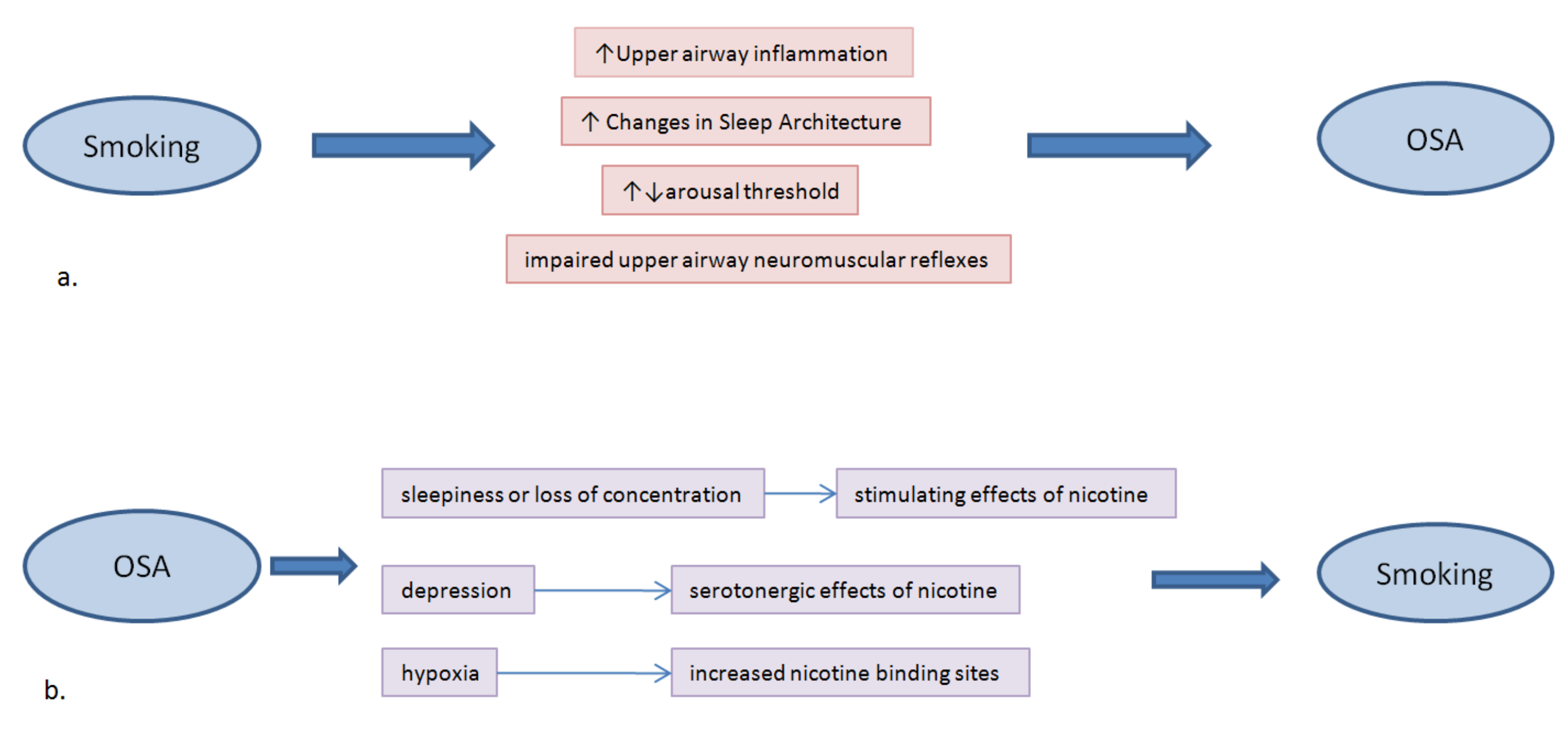
Figure 1. A summary of the bidirectional relationship between Obstructive Sleep Apnea (OSA) and cigarette smoking; (a) Mechanisms by which smoking can result in OSA; (b) Associations between OSA and smoking.
2.1. Upper Airway Inflammation due to Inhalation of Cigarette Smoke
Exposure to cigarette smoke may contribute to the inflammation of upper airways resulting in further narrowing and predisposing to the development of hypopneas and apneas. OSA alone has been found to be associated with inflammation of the upper airway [18]. In the study of Kim et al. [18], all the patients with moderate to severe OSA presented increased thickness and edema of the uvular mucosa in upper airway mucosal biopsy. Additionally, increased calcitonin gene-related peptide (CGRP) was found in the biopsies of smokers with OSA. This may have possibly further contributed to the inflammation of the upper airways of these patients. However further studies are needed to clarify the relationship of the inflammation caused by smoking and OSA pathogenesis.
Cigarette smoke has been found to reversibly activate hypoxia-inducible factor 1 (HIF-1α) [21] and this factor has been also found unregulated in OSA patients. As HIF-1α has been involved in the regulation of metabolic processes and in the development of insulin resistance and diabetes, it may further contribute to the development and aggravation of the metabolic co-morbidities of OSA [22].
2.2. Changes in Sleep Architecture and Smoking
Another mechanism by which smoking may have an impact on OSA pathogenesis is by its effect on sleep architecture [23][24][25]. There is evidence for an association between smoking and a worse sleep quality. Current smokers reported daytime sleepiness, difficulty falling and staying asleep, and increased insomnia symptoms [26] more frequently than non-smokers, with male smokers more likely to report nightmares [24]. Data from the Sleep Heart Health Study [27] demonstrated that current smokers, as compared with nonsmokers or former smokers, had longer sleep latency and a higher proportion of lighter sleep. However, no differences in sleep architecture were found between never and former smokers [27]. Analysis using EEG spectral analysis, demonstrated that the differences in sleep quality between smokers and nonsmokers were more evident during the early part of the night and decreased during the end [28]. The predominance of disturbances during the earlier part of the night may be attributed to the immediate effects of nicotine and/or to the nicotine withdrawal effects. Shorter sleep time, longer sleep latency, and higher rapid eye movement (REM) sleep density were found in smokers compared to non-smokers when matched by sex and age, in a study that used in-laboratory polysomnography [29]. Further, a larger analysis from 1492 adults that also used data from in-laboratory sleep studies, reported that current smokers had a higher arousal index and more sleep time with saturation of oxygen (SaO2) less than 90% compared with nonsmokers [30]. However, there is still a need for further objective data in order to support the hypothesis that current smoking is associated with poor sleep quality leading to OSA.
2.3. Smoking May Affect Arousal Threshold
Arousals have been implicated in the pathogenesis of OSA [7][8][31]. There is a hypothesis that smoking results in a higher arousal threshold mostly from pediatric clinical studies, but there is still conflicting evidence. Due to nicotine’s short half-life, its effects on the arousal threshold may be different during the early period of the night compared with the end. In the study of Conway et al. [30], smokers presented a higher arousal index, with longer respiratory events and greater desaturations. On the other hand, infants that were exposed to maternal smoking demonstrated reduced arousability from sleep and passive smoking is a recognized risk factor for the development of sudden infant death syndrome [32][33]. Further data are needed as the higher arousal threshold may result in less instability of sleep and decrease the collapsibility of upper airways [23].
2.4. Smoking May Impair Upper Airway Neuromuscular Reflexes
The impairment of the protective upper airway neuromuscular reflexes by nicotine is considered to be another potential mechanism by which smoking may affect sleep apnea. Data from animal models have shown that exposure to passive smoking in lambs resulted in enhanced respiratory inhibition and in more apneas with laryngeal stimulation [34]. Studies in animal models support the hypothesis that nicotine exposure may enhance the constriction of the upper airways; however, data in humans to support this are scarce.
3. Association between Smoking and OSA
The association between smoking and OSA is not currently well-established (Figure 1). Active but not former smoking was associated with a higher possibility of developing moderate or severe OSA in the Wisconsin Sleep Cohort Study, even after adjusting for confounding factors, and especially in heavy smokers [14]. Other smaller studies showed that OSA and smoking were independently associated, and that the prevalence of current smoking was higher in OSA patients compared with those that did not suffer from OSA [35][36]. Similarly, it was found that smoking related with earlier age of OSA diagnosis and that heavy smokers suffered from more severe disease [37]. Likewise, in a large single-center study that included 3613 OSA patients, it was reported that smokers suffering from OSA presented higher AHI and lower mean oxygenation during sleep [38]. A more recent study had also demonstrated the significant effect of increased smoking status, expressed by Pack/Years (P/Ys), with OSA severity, expressed by Apnea Hypopnea Index (AHI) and oxygen desaturation index (ODI) [39]. The group had recently performed a study evaluating the effects of smoking on OSA and even if the researchers did not find an independent effect of smoking on OSA, the severity of smoking status (measured by number of cigarettes/days, P/Ys), and nicotine dependence were found higher in patients with more severe OSA. Smoking was not significantly associated with OSA after adjusting for gender, age, BMI, and alcohol [40]. Similarly, another study reported that smoking was not associated with AHI but only with ODI and arousals, with these events been more pronounced in current smokers [30]. Those that smoked more than 15 P/Ys presented higher arousal index and longer time spend with SaO2 < 90%. Former smokers with a history of more than 15 P/Ys presented higher arousal index and AHI compared with those with less P/Ys [30].
On the other hand, there are other studies that did not find a causal relationship between cigarette smoking and OSA. Older studies have demonstrated that smokers present a significant decrease in nocturnal oxygen saturation, but when compared with non-smokers, no significant differences in either AHI or ODI were found [41]. However, evidence from the Sleep Heart Health Study showed that the former, but not current smoking was associated with more severe disease. An inverse association between current smoking and AHI was observed, with lower AHI values in current smokers [42]. Additionally, a large population study had also found that current smoking was strongly but inversely related with self-reported OSA both in men and women [43]. A large cross-sectional study reported that, after adjusting for age, BMI, and gender, smoking was not an independent risk factor for OSA. However, the same study found that patients with more severe disease (AHI > 50) were heavier smokers and also that compared with non-smokers, heavy smokers presented higher AHI [44]. Similarly, another study also concluded that although there was no significant association between smoking and OSA, smokers presented higher AHI [45]. In a retrospective analysis, when current/former smokers were compared with non-smokers, no significant differences in the AHI were reported but a lower nocturnal mean oxygen saturation was found in current/former smokers [46]. These three studies [44][45][46] reported that smokers presented worse daytime sleepiness that was attributed to nicotine’s effects on the upper airway, on sleep architecture, and also to nocturnal hypoxia. In a more recent meta-analysis, there was evidence to confirm that OSA was related with alcohol use, but not with tobacco or caffeine. However, the level of evidence in that analysis was low and the results should be interpreted with caution [47].
The differences between the results of the aforementioned studies could be explained by the different populations that were examined, as some of the studies evaluated populations from the community setting and others population referred to a sleep clinic. Additionally, according to CDC (https://www.cdc.gov/nchs/nhis/tobacco/tobacco_glossary.htm, accessed 2 August 2022) a current smoker is defined as an adult who has smoked 100 cigarettes in his or her lifetime and who currently smokes cigarettes, and a former smoker as an adult who has smoked at least 100 cigarettes in his or her lifetime but who had quit smoking at the time of the research. Passive smoking or second-hand smoke is the inhalation of environmental tobacco smoke. A heavy smoker is the smoker who consumes 20 or more cigarettes per day. (https://www.canada.ca/en/health-canada/services/health-concerns/tobacco/research/tobacco-use-statistics/terminology.html, accessed 2 August 2022) [37]. However, it is worth mentioning that in some studies the aforementioned criteria may differ, i.e., a heavy smoker defined as someone who smokes more than 40 cigarettes per day [39], or a current smoker someone who smokes more than 10 pack/years [41] and this may also explain the differences in the results.
References
- Dempsey, J.A.; Veasey, S.C.; Morgan, B.J.; O’Donnell, C.P. Pathophysiology of Sleep Apnea. Physiol. Rev. 2010, 90, 47–112.
- Marshall, N.S.; Wong, K.K.H.; Liu, P.Y.; Cullen, S.R.J.; Knuiman, M.W.; Grunstein, R.R. Sleep Apnea as an Independent Risk Factor for All-Cause Mortality: The Busselton Health Study. Sleep 2008, 31, 1079–1085.
- George, C.; Nickerson, P.; Hanly, P.; Millar, T.; Kryger, M. Sleep apnoea patients have more automobile accidents. Lancet 1987, 330, 447.
- Jordan, A.S.; McSharry, D.G.; Malhotra, A. Adult obstructive sleep apnoea. Lancet 2013, 383, 736–747.
- Weaver, T.E.; Grunstein, R.R. Adherence to Continuous Positive Airway Pressure Therapy: The Challenge to Effective Treatment. Proc. Am. Thorac. Soc. 2008, 5, 173–178.
- Randerath, W.; Verbraecken, J.; de Raaff, C.; Hedner, J.; Herkenrath, S.; Hohenhorst, W.; Jakob, T.; Marrone, O.; Marklund, M.; McNicholas, W.T.; et al. European Respiratory Society guideline on non-CPAP therapies for obstructive sleep apnoea. Eur. Respir. Rev. 2021, 30, 210200.
- Eckert, D.J.; White, D.P.; Jordan, A.S.; Malhotra, A.; Wellman, A. Defining Phenotypic Causes of Obstructive Sleep Apnea. Identification of Novel Therapeutic Targets. Am. J. Respir. Crit. Care Med. 2013, 188, 996–1004.
- Edwards, B.A.; Eckert, D.J.; McSharry, D.G.; Sands, S.A.; Desai, A.; Kehlmann, G.; Bakker, J.P.; Genta, P.R.; Owens, R.L.; White, D.P.; et al. Clinical Predictors of the Respiratory Arousal Threshold in Patients with Obstructive Sleep Apnea. Am. J. Respir. Crit. Care Med. 2014, 190, 1293–1300.
- Younes, M.; Ostrowski, M.; Thompson, W.; Leslie, C.; Shewchuk, W. Chemical Control Stability in Patients with Obstructive Sleep Apnea. Am. J. Respir. Crit. Care Med. 2001, 163, 1181–1190.
- Deleanu, O.C.; Pocora, D.; Mihalcu¸ta, S.; Ulmeanu, R.; Zaharie, A.M.; Mihal¸tan, F.D. Influence of smoking on sleep and obstructive sleep apnea syndrome. Pneumologia 2016, 65, 28–35.
- Bearpark, H.; Elliott, L.; Grunstein, R.; Cullen, S.; Schneider, H.; Althaus, W.; Sullivan, C. Snoring and sleep apnea. A population study in Australian men. Am. J. Respir. Crit. Care Med. 1995, 151, 1459–1465.
- Franklin, K.A.; Gíslason, T.; Omenaas, E.; Jõgi, R.; Jensen, E.J.; Lindberg, E.; Gunnbjörnsdóttir, M.; Nyström, L.; Laerum, B.N.; Björnsson, E.; et al. The Influence of Active and Passive Smoking on Habitual Snoring. Am. J. Respir. Crit. Care Med. 2004, 170, 799–803.
- Lindberg, E.; Taube, A.; Janson, C.; Gislason, T.; Svärdsudd, K.; Boman, G. A 10-Year Follow-up of Snoring in Men. Chest 1998, 114, 1048–1055.
- Wetter, D.W.; Young, T.B.; Bidwell, T.R.; Badr, M.S.; Palta, M. Smoking as a risk factor for sleep-disordered breathing. Arch. Intern. Med. 1994, 154, 2219–2224.
- Krishnan, V.; Dixon-Williams, S.; Thornton, J.D. Where there is smoke there is sleep apnea: Exploring the relationship between smoking and sleep apnea. Chest 2014, 146, 1673–1680.
- Lui, M.M.S.; Mak, J.C.W.; Lai, A.Y.K.; Hui, C.K.M.; Lam, J.C.M.; Lam, D.C.L.; Ip, M.S.M. The Impact of Obstructive Sleep Apnea and Tobacco Smoking on Endothelial Function. Respiration 2016, 91, 124–131.
- Chang, C.-W.; Chang, C.-H.; Chuang, H.-Y.; Cheng, H.-Y.; Lin, C.-I.; Chen, H.-T.; Yang, C.-C. What is the association between secondhand smoke (SHS) and possible obstructive sleep apnea: A meta-analysis. Environ. Health 2022, 21, 58.
- Kim, K.S.; Kim, J.H.; Park, S.Y.; Won, H.-R.; Lee, H.-J.; Yang, H.S.; Kim, H.J. Smoking Induces Oropharyngeal Narrowing and Increases the Severity of Obstructive Sleep Apnea Syndrome. J. Clin. Sleep Med. 2012, 8, 367–374.
- Schrand, J.R. Is sleep apnea a predisposing factor for tobacco use? Med. Hypotheses 1996, 47, 443–448.
- Lin, Y.-N.; Li, Q.-Y.; Zhang, X.-J. Interaction between smoking and obstructive sleep apnea: Not just participants. Chin. Med. J. 2012, 125, 3150–3156.
- Daijo, H.; Hoshino, Y.; Kai, S.; Suzuki, K.; Nishi, K.; Matsuo, Y.; Harada, H.; Hirota, K. Cigarette smoke reversibly activates hypoxia-inducible factor 1 in a reactive oxygen species-dependent manner. Sci. Rep. 2016, 6, srep34424.
- Gabryelska, A.; Karuga, F.F.; Szmyd, B.; Białasiewicz, P. HIF-1α as a Mediator of Insulin Resistance, T2DM, and Its Complications: Potential Links With Obstructive Sleep Apnea. Front. Physiol. 2020, 11, 1035.
- Series, F.; Roy, N.; Marc, I. Effects of sleep deprivation and sleep fragmentation on upper airway collapsibility in normal subjects. Am. J. Respir. Crit. Care Med. 1994, 150, 481–485.
- Wetter, D.; Young, T. The Relation Between Cigarette Smoking and Sleep Disturbance. Prev. Med. 1994, 23, 328–334.
- Phillips, B.A.; Danner, F.J. Cigarette smoking and sleep disturbance. Arch. Intern. Med. 1995, 155, 734–737.
- McNamara, J.P.; Wang, J.; Holiday, D.B.; Warren, J.Y.; Paradoa, M.; Balkhi, A.M.; Fernandez-Baca, J.; McCrae, C. Sleep disturbances associated with cigarette smoking. Psychol. Health Med. 2013, 19, 410–419.
- Zhang, L.; Samet, J.; Caffo, B.; Punjabi, N.M. Cigarette Smoking and Nocturnal Sleep Architecture. Am. J. Epidemiol. 2006, 164, 529–537.
- Zhang, L.; Samet, J.; Caffo, B.; Bankman, I.; Punjabi, N.M. Power Spectral Analysis of EEG Activity During Sleep in Cigarette Smokers. Chest 2008, 133, 427–432.
- Jaehne, A.; Unbehaun, T.; Feige, B.; Lutz, U.C.; Batra, A.; Riemann, D. How smoking affects sleep: A polysomnographical analysis. Sleep Med. 2012, 13, 1286–1292.
- Conway, S.; Roizenblatt, S.; Palombini, L.; Castro, L.; Bittencourt, L.; Silva, R.; Tufik, S. Effect of smoking habits on sleep. Braz. J. Med Biol. Res. 2008, 41, 722–727.
- Eckert, D.J.; Younes, M.K. Arousal from sleep: Implications for obstructive sleep apnea pathogenesis and treatment. J. Appl. Physiol. 2014, 116, 302–313.
- DiFranza, J.R.; Aligne, C.A.; Weitzman, M. Prenatal and Postnatal Environmental Tobacco Smoke Exposure and Children’s Health. Pediatrics 2004, 113, 1007–1015.
- Horne, R.S.; Parslow, P.M.; Ferens, D.; Bandopadhayay, P.; Osborne, A.; Watts, A.-M.; Cranage, S.M.; Adamson, T. Arousal responses and risk factors for sudden infant death syndrome. Sleep Med. 2002, 3, S61–S65.
- St-Hilaire, M.; Duvareille, C.; Avoine, O.; Carreau, A.M.; Samson, N.; Micheau, P.; Doueik, A.; Praud, J.P. Effects of postnatal smoke exposure on laryngeal chemorefl exes in newborn lambs. J. Appl. Physiol. 2010, 109, 1820–1826.
- Kashyap, R.; Hock, L.M.; Bowman, T.J. Higher prevalence of smoking in patients diagnosed as having obstructive sleep apnea. Sleep Breath. 2001, 5, 167–172.
- Boussoffara, L.; Boudawara, N.; Sakka, M.; Knani, J. Smoking habits and severity of obstructive sleep apnea hypopnea syndrome. Rev. Mal. Respir. 2013, 30, 38–43.
- Varol, Y.; Anar, C.; Tuzel, O.E.; Guclu, S.Z.; Ucar, Z.Z. The impact of active and former smoking on the severity of obstructive sleep apnea. Sleep Breath. 2015, 19, 1279–1284.
- Bielicki, P.; Trojnar, A.; Sobieraj, P.; Wąsik, M. Smoking Status in Relation to Obstructive Sleep Apnea Severity (OSA) And Cardiovascular Comorbidity in Patients with Newly Diagnosed OSA. Adv. Respir. Med. 2019, 87, 103–109.
- Yosunkaya, S.; Kutlu, R.; Vatansev, H. Effects of smokıng on patıents wıth obstructıve sleep apnea syndrome. Clin. Respir. J. 2021, 15, 147–153.
- Ioannidou, D.; Kalamaras, G.; Kotoulas, S.-C.; Pataka, A. Smoking and Obstructive Sleep Apnea: Is There An Association between These Cardiometabolic Risk Factors?—Gender Analysis. Medicina 2021, 57, 1137.
- Casasola, G.G.; Alvarez-Sala, J.L.; Marques, J.A.; Sánchez-Alarcos, J.M.F.; Tashkin, D.P.; Espinós, D. Cigarette smoking behavior and respiratory alterations during sleep in a healthy population. Sleep Breath. 2002, 6, 19–24.
- Nieto, F.J.; Young, T.B.; Lind, B.K.; Shahar, E.; Samet, J.M.; Redline, S.; D’Agostino, R.B.; Newman, A.B.; Lebowitz, M.D.; Pickering, T.G.; et al. Association of Sleep-Disordered Breathing, Sleep Apnea, and Hypertension in a Large Community-Based Study. JAMA 2000, 283, 1829–1836.
- Huang, T.; Lin, B.M.; Markt, S.; Stampfer, M.J.; Laden, F.; Hu, F.B.; Tworoger, S.S.; Redline, S. Sex differences in the associations of obstructive sleep apnoea with epidemiological factors. Eur. Respir. J. 2018, 51, 1702421.
- Hoflstein, V. Relationship between smoking and sleep apnea in clinic population. Sleep 2002, 25, 519–524.
- Hsu, W.-Y.; Chiu, N.-Y.; Chang, C.-C.; Chang, T.-G.; Lane, H.-Y. The association between cigarette smoking and obstructive sleep apnea. Tob. Induc. Dis. 2019, 17, 27.
- Shao, C.; Qi, H.; Fang, Q.; Tu, J.; Li, Q.; Wang, L. Smoking history and its relationship with comorbidities in patients with obstructive sleep apnea. Tob. Induc. Dis. 2020, 18, 56.
- Taveira, K.V.M.; Kuntze, M.M.; Berretta, F.; De Souza, B.D.M.; Godolfim, L.R.; Demathe, T.; Canto, G.D.L.; Porporatti, A.L. Association between obstructive sleep apnea and alcohol, caffeine and tobacco: A meta-analysis. J. Oral Rehabil. 2018, 45, 890–902.
More
Information
Subjects:
Primary Health Care; Health Policy & Services
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.4K
Revisions:
2 times
(View History)
Update Date:
14 Sep 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




