
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Luisa Chocarro | -- | 3462 | 2022-08-08 12:00:23 | | | |
| 2 | Beatrix Zheng | -89 word(s) | 3373 | 2022-08-10 03:23:09 | | | | |
| 3 | Beatrix Zheng | Meta information modification | 3373 | 2022-08-10 03:29:43 | | | | |
| 4 | Beatrix Zheng | Meta information modification | 3373 | 2022-08-10 03:32:10 | | |
Video Upload Options
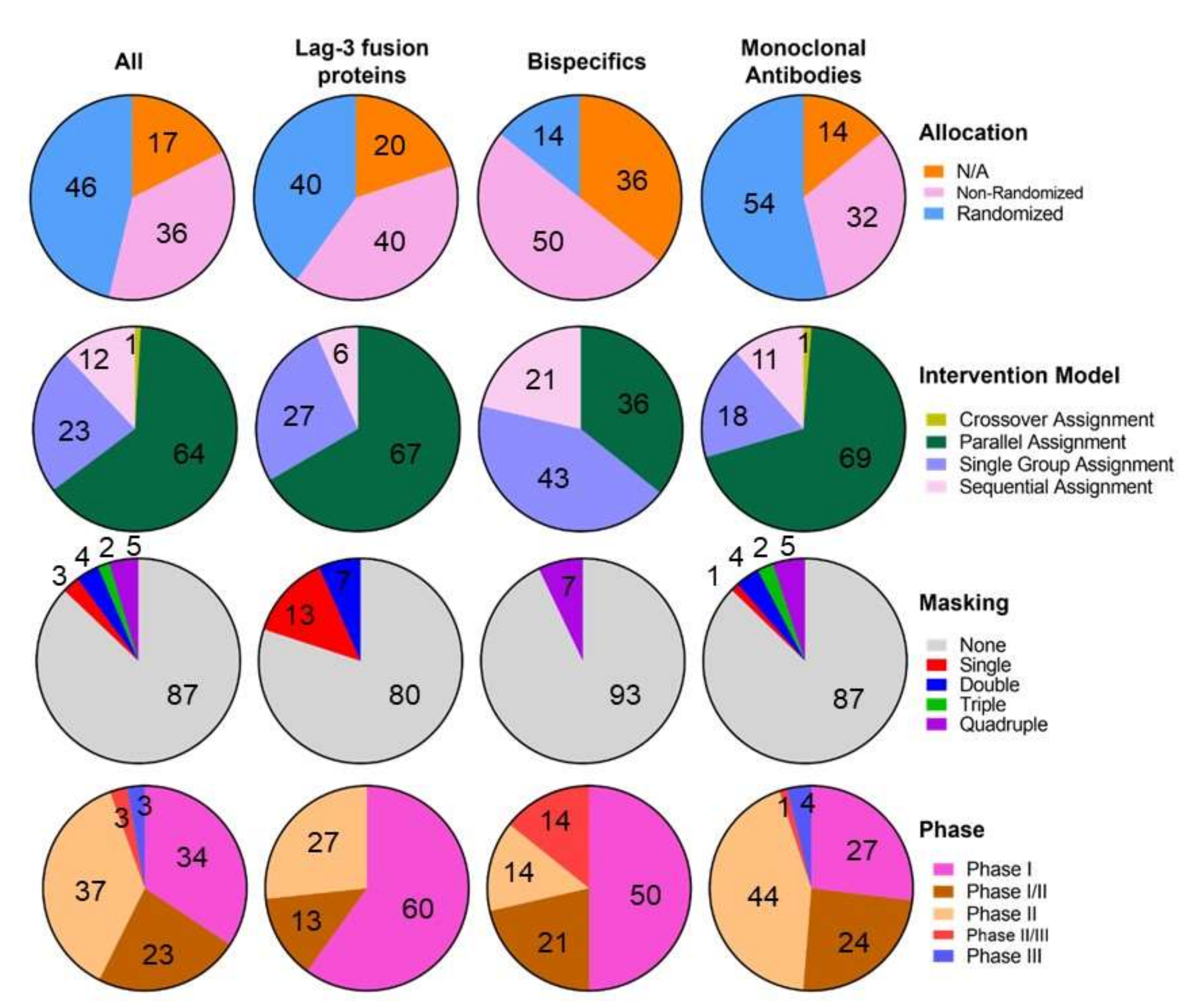
Immune checkpoint inhibitors (ICIs) have revolutionized medical practice in oncology since the FDA approval of the first ICI 11 years ago. In light of this, Lymphocyte-Activation Gene 3 (LAG-3) is one of the most important next-generation immune checkpoint molecules, playing a similar role as Programmed cell Death protein 1 (PD-1) and Cytotoxic T-Lymphocyte Antigen 4 (CTLA-4). 19 LAG-3 targeting molecules are being evaluated at 108 clinical trials which are demonstrating positive results, including promising bispecific molecules targeting LAG-3 simultaneously with other ICIs. Recently, a new dual anti-PD-1 (Nivolumab) and anti-LAG-3 (Relatimab) treatment developed by Bristol Myers Squibb (Opdualag), was approved by the Food and Drug Administration (FDA) as the first LAG-3 blocking antibody combination for unresectable or metastatic melanoma. This novel immunotherapy combination more than doubled median progression-free survival (PFS) when compared to nivolumab monotherapy (10.1 months versus 4.6 months).
1. LAG-3 Molecular Function
2. LAG-3 Clinical Research
2.1. Anti-LAG-3 Monoclonal Antibodies
-
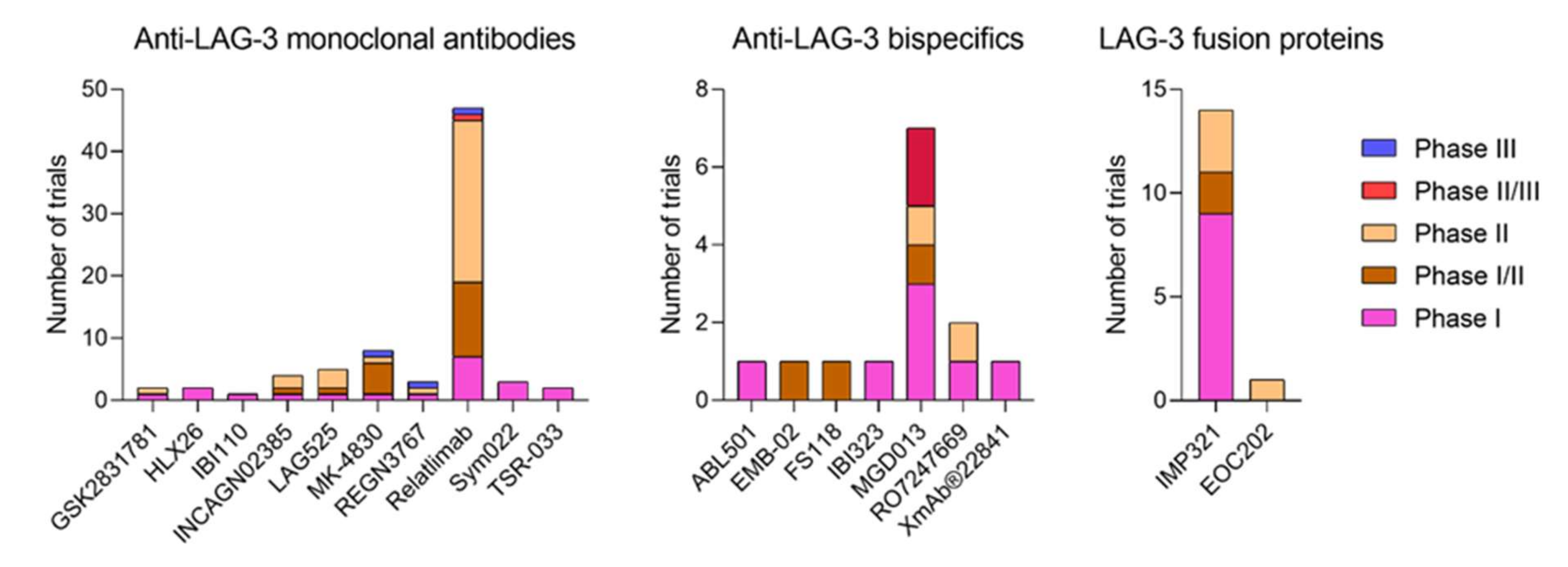
BMS-986016 or relatlimab, developed by Bristol-Myers Squibb in 47 clinical trials, was the first anti-LAG-3 monoclonal antibody to be clinically developed and the first one to receive the FDA approval for its clinical use. It has 4 subunits, with 16 disulfide links and 2 N-glycosylation sites, with an average molecular weight of 145.3 kDa [78]. Phase I (7 trials), I/II (12 trials), II (26 trials), II/III (1 trial) and III (1 trial) preliminary results showed good tolerability, efficacy, toxicity and antitumour profiles alone or in combination with anti-PD-1/PD-L1 blockade immunotherapies, as a good alternative to overcome immunotherapy resistance [79][80][81]. For example, it restores T cell mediated responses and TNF-a, IFN-y and IL-2 cytokine release [82]. The phase III clinical trial that led to the LAG-3/PD-1 combination approval for melanoma treatment is further discussed in the next section.
-
GSK2831781, derived from IMP731 Immunetep’s antibody, developed in monotherapy by GlaxoSmithKline in 3 clinical trials (2 phase I and 1 phase II) for psoriasis and ulcerative colitis. The ulcerative colitis phase II trial was terminated after an interim analysis [83], but phase I results show good tolerability, safety and inflammation regulation profiles [84].
-
HLX26, developed by Fosun Pharma in 2 phase I clinical trials (NCT05078593 and NCT05400265), where its safety, tolerability, pharmacokinetic characteristics and preliminary efficacy are being evaluated alone and in combination with anti-PD-1 treatments in patients with solid tumors or lymphoma.
-
IBI110, developed by Innovent Biologics in a phase I clinical trial alone and in combination with anti-PD-1 in patients with relapsed or refractory diffuse large B cell lymphoma (r/r DLBCL) (NCT05039658).
-
INCAGN02385, is being developed by Incyte in 4 clinical trials (1 phase I, 1 phase I/II and 2 phase II) alone (NCT03538028) or in combination (NCT04370704, NCT05287113, NCT04586244) with anti-PD-1 and anti-TIM-3 immune checkpoint therapies. Preliminary data shows good tolerability profiles [85].
-
LAG525 or IMP701 developed by Novartis in 5 clinical trials (1 phase I, 1 phase I/II and 3 phase II), alone or in combination with anti-PD-1 blockers. The structure of this antibody consists of 4 subunits, 16 disulfide bridges and 2 N-glycosylation sites, with an estimated molecular weight of 147 kDa [86]. Preliminary data demonstrate promising pharmacokinetics, antitumour activity and safety alone and in combination [87][88][89].
-
MK-4830 or favezelimab, developed by Merck in 8 clinical trials (1 phase I, 5 phase I/II, 1 phase II and 1 phase III), alone or in combination with anti-PD-1, oxaliplatin, Leucovorin (Calcium Folinate), Fluorouracil [5-FU] and lenvatinib, showing manageable safety and tolerability alone and in combination. In fact, anti-LAG-3/anti-PD-1 combination showed a 6.3% objective response rate, better than the monotherapy treatment, with similar treatment-related adverse effects [90][91]. The structure of this antibody consists of 4 subunits, 16 disulfide bridges and 2 glycosylation sites, with an estimated molecular weight of 146 kDa [92].
-
REGN3767 or fianlimab, developed by Regeneron Pharmaceuticals and Sanofi in 3 clinical trials (1 phase I, 1 phase II and 1 phase III), promotes T cell activation and T cell mediated cytotoxicity with good pharmacokinetics and toxicology profiles in vitro and in vivo [93]. The structure of the antibody is composed of 4 subunits, 16 sulfide bridges and 2 N-glycosilation sites [94]. Early efficacy and antitumor activity were also suggested in the preliminary clinical trials results. Its combination with cemiplimab also showed a good safety profile [95][96][97]. The combination with anti-PD-1, and cemiplimab is being evaluated in phase I (NCT03005782), II (NCT01042379) and III (NCT05352672) trials while it is being studied alone in the NCT03005782 phase I trial. Interestingly, anti-LAG-3 PET tracers (89Zr-DFO-REGN3767) are being clinically developed to establish the tracer biodistribution and dosimetry, monitoring the response to REGN3767 treatment (NCT05346276, NCT04706715, NCT04566978). However, these clinical trials are not being considered in this research as LAG-3 targeting clinical trials, because their main purpose is establishing PET scanning as a diagnostic method.
-
Sym022, developed by Symphogen in 3 phase I clinical trials, is being evaluated for dose-escalation and dose-expansion alone (NCT03489369) or in combination (NCT03311412, NCT04641871) with anti-PD-1 and anti-TIM-3 immunotherapies. The treatment combination showed synergic antitumor activity in preclinical models [98][99].
-
TSR-033, is being developed by Tesaro in 2 phase I clinical trials, alone and in combination with anti-PD-1 and anti-TIM-3 treatments (NCT03250832, NCT02817633). The combination with PD-1 blockers increases CD4 T cell activation and IL-2 production and cell proliferation [100]. Phase I preliminary data indicates good safety and tolerability.
2.2. Anti-LAG-3 Bispecific Antibodies
-
ABL501 is being developed by ABL Bio in a phase I trial for the treatment of any progressive, locally advanced (unresectable) or metastatic solid tumor (NCT05101109). This bispecific antibody blocks PD-L1 and LAG-3 as a single agent. Dose-escalation analysis is being conducted. The dosing interval to be used in the dose-expansion part will be re-evaluated based on the emerging safety and pharmacokinetics data from the dose-escalation part of the research. It promotes enhanced human T cell activation in vitro and potentiates antitumor responses of T cells through DC activation [101][102].
-
IBI323, a LAG-3/PD-L1 bispecific antibody, is being developed by Innovent Biologics in a phase I clinical trial alone and in combination with chemotherapy in patients with advanced malignancies. The purpose of this resesarch is to evaluate IBI323 safety, tolerability and efficacy. It enhances tumor-specific immunity in vitro [103].
-
MGD013 or Tebotelimab, a LAG-3/PD-1 bispecific DART® antibody, is being developed by MacroGenetics in 7 clinical trials (3 phase I, 1 phase I/II, 1 phase II and 2 phase II/III) in patients with unresectable or metastatic neoplasms (NCT03219268), patients with advanced or metastatic solid tumors who failed prior treatment (NCT04178460), melanoma (NCT04653038), liver cancer (NCT04212221), Head and Neck Cancer (NCT04634825, NCT04082364) and HER2+ Gastric/GEJ Cancer (NCT04082364), to evaluate its safety and efficacy, alone or in combination with margetuximab (anti-HER2), niraparib (a selective PARP1/2 inhibitor), Brivanib Alaninate (Multitargeted tyrosine kinase inhibitor) and enoblituzumab (Anti-B7-H3 antibody). Preliminary results showed good tolerability, safety and antitumour activity profiles [104].
-
RO7247669, a LAG-3/PD-1 bispecific antibody, is being developed by Hoffmann-La Roche in 1 phase I and 1 phase II clinical trials in patients with advanced and/or metastatic solid tumors (NCT04140500) and advanced or metastatic squamous cell carcinoma of the oesophagus (NCT04785820), alone or in combination with a PD-1/TIM-3 bispecific antibody or an anti-PD-1 single agent.
-
XmAb®22841 or pavunalimab, a LAG-3/CTLA-4 bispecific antibody, is being developed by Xencor in a phase I clinical trial (NCT03849469), alone and in combination with anti-PD-1 as a single agent in selected advanced solid tumors. It enhances antitumor activity, T cell activation, cytokine secretion and cell proliferation [105].
-
EMB-02, a LAG-3/PD-1 bispecific antibody, is being developed as a single treatment agent by EpimAb Biotherapeutics in a phase I/II clinical trial (NCT04618393) in advanced solid tumors. Dose escalation followed by cohort expansion will be performed. In vivo preclinical data showed antitumor activity in anti-PD-1 resistant models.
-
FS118, a LAG-3/PD-L1 bispecific antibody, is being developed as a single agent treatment by F-star Therapeutics in a phase I/II clinical trial (NCT03440437) in patients with advanced malignancies, to determine dosing and toxicity. It enhanced T cell activation and antitumor activity in vitro and in vivo [105][106][107]. Preliminary clinical trial data showed good pharmacodynamics and tolerability profiles. [108][109].
-
CB213 Humabody®, a PD-1xLAG-3 antagonist developed by Crescendo Biologics Ltd., have recently entered a partnership with Cancer Research UK for its clinical development into a future phase I clinical trial ([110]). This bispecific molecule binds and blocks with high affinity PD1 and LAG-3 on PD-1+LAG-3+ T cells, induces ex vivo T cell proliferation of dysfunctional T cells from NSCLC patients, with superior activity than anti-PD-1 alone and suppress tumor growth in vivo [111].
2.3. LAG-3 Fusion Proteins
-
IMP321, Eftilagimod Alpha or Efti, a LAG-3 soluble fusion protein, is being developed by Immutep in 14 clinical trials (9 phase I, 2 phase I/II and 3 phase II) for the treatment of advanced solid tumors, hepatitis B and flu. IMP321 is being developed as an adjuvant and immune modulator for cancer and vaccines against infectious diseases, as well as an anticancer treatment agent. It is being tested alone and in combination with chemotherapy (gemcitabine), anti-PD-L1, anti-PD-1, paclitaxel, hepatitis B antigen (without alum), a reference flu antigen, Melan-A VLP vaccine and melanoma tumor-specific peptides. Data shows that IMP321 enhances T cell activation and proliferation, humoral, effector and adaptive immunity, cytokine release, immunogenicity and antitumor activity, with good tolerability, efficacy and safety profiles [112][113][114][115][116][117][118][119][120].
-
EOC202, a recombinant human LAG-3 fusion protein, is being developed by Taizhou EOC Pharma in a phase II clinical trial (NCT05322720) in HR+, HER2- advanced breast cancer with progression after endocrine therapy to evaluate the PFS for EOC202 combined with albumin-bound paclitaxel versus albumin-bound paclitaxel alone.
2.4. Anti-LAG-3 CAR-T Cells
3. Opdualag and Its Pathway towards the Clinic
References
- De Erauso, L.C.; Zuazo, M.; Arasanz, H.; Bocanegra, A.; Hernandez, C.; Fernandez, G.; Garcia-Granda, M.J.; Blanco, E.; Vera, R.; Kochan, G.; et al. Resistance to PD-L1/PD-1 Blockade Immunotherapy. A Tumor-Intrinsic or Tumor-Extrinsic Phenomenon? Front. Pharmacol. 2020, 11, 441.
- Chocarro, L.; Blanco, E.; Arasanz, H.; Fernández-Rubio, L.; Bocanegra, A.; Echaide, M.; Garnica, M.; Ramos, P.; Fernández-Hinojal, G.; Vera, R.; et al. Clinical landscape of LAG-3-targeted therapy. Immunol.-Oncol. Technol. 2022, 14, 100079.
- Chocarro, L.; Blanco, E.; Zuazo, M.; Arasanz, H.; Bocanegra, A.; Fernández-Rubio, L.; Morente, P.; Fernández-Hinojal, G.; Echaide, M.; Garnica, M.; et al. Understanding LAG-3 Signaling. Int. J. Mol. Sci. 2021, 22, 5282.
- Triebel, F.; Jitsukawa, S.; Baixeras, E.; Roman-Roman, S.; Genevee, C.; Viegas-Pequignot, E.; Hercend, T. LAG-3, a novel lymphocyte activation gene closely related to CD4. J. Exp. Med. 1990, 171, 1393–1405.
- Huard, B.; Prigent, P.; Pagès, F.; Bruniquel, D.; Triebel, F. T cell major histocompatibility complex class II molecules down-regulate CD4+ T cell clone responses following LAG-3 binding. Eur. J. Immunol. 1996, 26, 1180–1186.
- Huard, B.; Tournier, M.; Hercend, T.; Triebel, F.; Faure, F. Lymphocyte-activation gene 3/major histocompatibility complex class II interaction modulates the antigenic response of CD4+ T lymphocytes. Eur. J. Immunol. 1994, 24, 3216–3221.
- Andrews, L.P.; Marciscano, A.E.; Drake, C.G.; Vignali, D.A.A. LAG3 (CD223) as a cancer immunotherapy target. Immunol. Rev. 2017, 276, 80–96.
- Workman, C.J.; Cauley, L.S.; Kim, I.-J.; Blackman, M.A.; Woodland, D.L.; Vignali, D.A.A. Lymphocyte Activation Gene-3 (CD223) Regulates the Size of the Expanding T Cell Population Following Antigen Activation In Vivo. J. Immunol. 2004, 172, 5450–5455.
- Workman, C.J.; Dugger, K.J.; Vignali, D.A.A. Cutting Edge: Molecular Analysis of the Negative Regulatory Function of Lymphocyte Activation Gene-3. J. Immunol. 2002, 169, 5392–5395.
- Williams, J.B.; Horton, B.L.; Zheng, Y.; Duan, Y.; Powell, J.D.; Gajewski, T.F. The EGR2 targets LAG-3 and 4-1BB describe and regulate dysfunctional antigen-specific CD8+ T cells in the tumor microenvironment. J. Exp. Med. 2017, 214, 381–400.
- Huang, R.-Y.; Eppolito, C.; Lele, S.; Shrikant, P.; Matsuzaki, J.; Odunsi, K. LAG3 and PD1 co-inhibitory molecules collaborate to limit CD8+ T cell signaling and dampen antitumor immunity in a murine ovarian cancer model. Oncotarget 2015, 6, 27359–27377.
- Grosso, J.F.; Goldberg, M.V.; Getnet, D.; Bruno, T.C.; Yen, H.-R.; Pyle, K.J.; Hipkiss, E.; Vignali, D.A.A.; Pardoll, D.M.; Drake, C.G. Functionally Distinct LAG-3 and PD-1 Subsets on Activated and Chronically Stimulated CD8 T Cells. J. Immunol. 2009, 182, 6659–6669.
- Grosso, J.F.; Kelleher, C.C.; Harris, T.J.; Maris, C.H.; Hipkiss, E.L.; De Marzo, A.; Anders, R.; Netto, G.; Getnet, D.; Bruno, T.C.; et al. LAG-3 regulates CD8+ T cell accumulation and effector function in murine self- and tumor-tolerance systems. J. Clin. Investig. 2007, 117, 3383–3392.
- Chihara, N.; Madi, A.; Kondo, T.; Zhang, H.; Acharya, N.; Singer, M.; Nyman, J.; Marjanovic, N.D.; Kowalczyk, M.S.; Wang, C.; et al. Induction and transcriptional regulation of the co-inhibitory gene module in T cells. Nature 2018, 558, 454–459.
- Blackburn, S.D.; Shin, H.; Haining, W.N.; Zou, T.; Workman, C.J.; Polley, A.; Betts, M.R.; Freeman, G.J.; A A Vignali, D.; Wherry, E.J. Coregulation of CD8+ T cell exhaustion by multiple inhibitory receptors during chronic viral infection. Nat. Immunol. 2008, 10, 29–37.
- Camisaschi, C.; Casati, C.; Rini, F.; Perego, M.; De Filippo, A.; Triebel, F.; Parmiani, G.; Belli, F.; Rivoltini, L.; Castelli, C. LAG-3 Expression Defines a Subset of CD4+CD25highFoxp3+ Regulatory T Cells That Are Expanded at Tumor Sites. J. Immunol. 2010, 184, 6545–6551.
- Workman, C.J.; Vignali, D.A.A. Negative Regulation of T Cell Homeostasis by Lymphocyte Activation Gene-3 (CD223). J. Immunol. 2005, 174, 688–695.
- White, A.M.; Wraith, D.C. Tr1-Like T Cells—An Enigmatic Regulatory T Cell Lineage. Front. Immunol. 2016, 7, 355.
- Huard, B.; Tournier, M.; Triebel, F. LAG-3 does not define a specific mode of natural killing in human. Immunol. Lett. 1998, 61, 109–112.
- Baixeras, E.; Huard, B.; Miossec, C.; Jitsukawa, S.; Martin, M.; Hercend, T.; Auffray, C.; Triebel, F.; Piatier-Tonneau, D. Characterization of the lymphocyte activation gene 3-encoded protein. A new ligand for human leukocyte antigen class II antigens. J. Exp. Med. 1992, 176, 327–337.
- Huang, C.-T.; Workman, C.J.; Flies, D.; Pan, X.; Marson, A.L.; Zhou, G.; Hipkiss, E.L.; Ravi, S.; Kowalski, J.; Levitsky, H.I.; et al. Role of LAG-3 in Regulatory T Cells. Immunity 2004, 21, 503–513.
- Zuazo, M.; Arasanz, H.; Fernández-Hinojal, G.; García-Granda, M.J.; Gato, M.; Bocanegra, A.; Martínez, M.; Hernández, B.; Teijeira, L.; Morilla, I.; et al. Functional systemic CD 4 immunity is required for clinical responses to PD -L1/PD -1 blockade therapy. EMBO Mol. Med. 2019, 11, e10293.
- Matsuzaki, J.; Gnjatic, S.; Mhawech-Fauceglia, P.; Beck, A.; Miller, A.; Tsuji, T.; Eppolito, C.; Qian, F.; Lele, S.; Shrikant, P.; et al. Tumor-infiltrating NY-ESO-1–specific CD8 + T cells are negatively regulated by LAG-3 and PD-1 in human ovarian cancer. Proc. Natl. Acad. Sci. USA 2010, 107, 7875–7880.
- Bruniquel, D.; Borie, N.; Hannier, S.; Triebel, F. Regulation of expression of the human lymphocyte activation gene-3 (LAG-3) molecule, a ligand for MHC class II. Immunogenetics 1998, 48, 116–124.
- Annunziato, F.; Manetti, R.; Cosmi, L.; Galli, G.; Heusser, C.H.; Romagnani, S.; Maggi, E. Opposite role for interleukin-4 and interferon-γ on CD30 and lymphocyte activation gene-3 (LAG-3) expression by activated naive T cells. Eur. J. Immunol. 1997, 27, 2239–2244.
- Annunziato, F.; Manetti, R.; Tomasévic, I.; Giudizi, M.; Biagiotti, R.; Giannò, V.; Germano, P.; Mavilia, C.; Maggi, E.; Romagnani, S. Expression and release of LAG-3-encoded protein by human CD4 + T cells are associated with IFN-γ production. FASEB J. 1996, 10, 769–776.
- Bae, J.; Lee, S.J.; Park, C.-G.; Lee, Y.S.; Chun, T. Trafficking of LAG-3 to the Surface on Activated T Cells via Its Cytoplasmic Domain and Protein Kinase C Signaling. J. Immunol. 2014, 193, 3101–3112.
- Mao, X.; Ou, M.T.; Karuppagounder, S.S.; Kam, T.-I.; Yin, X.; Xiong, Y.; Ge, P.; Umanah, G.E.; Brahmachari, S.; Shin, J.-H.; et al. Pathological α-synuclein transmission initiated by binding lymphocyte-activation gene 3. Science 2016, 353.
- Angelopoulou, E.; Paudel, Y.N.; Villa, C.; Shaikh, M.F.; Piperi, C. Lymphocyte-Activation Gene 3 (LAG3) Protein as a Possible Therapeutic Target for Parkinson’s Disease: Molecular Mechanisms Connecting Neuroinflammation to α-Synuclein Spreading Pathology. Biology 2020, 9, 86.
- Guo, W.; Zhou, M.; Qiu, J.; Lin, Y.; Chen, X.; Huang, S.; Mo, M.; Liu, H.; Peng, G.; Zhu, X.; et al. Association of LAG3 genetic variation with an increased risk of PD in Chinese female population. J. NeuroInflamm. 2019, 16, 270.
- Lino, A.C.; Dang, V.D.; Lampropoulou, V.; Welle, A.; Joedicke, J.; Pohar, J.; Simon, Q.; Thalmensi, J.; Baures, A.; Flühler, V.; et al. LAG-3 Inhibitory Receptor Expression Identifies Immunosuppressive Natural Regulatory Plasma Cells. Immunity 2018, 49, 120–133.e9.
- Kisielow, M.; Kisielow, J.; Capoferri-Sollami, G.; Karjalainen, K. Expression of lymphocyte activation gene 3 (LAG-3) on B cells is induced by T cells. Eur. J. Immunol. 2005, 35, 2081–2088.
- Donia, M.; Andersen, R.; Kjeldsen, J.W.; Fagone, P.; Munir, S.; Nicoletti, F.; Andersen, M.H.; Straten, P.T.; Svane, I.M. Aberrant Expression of MHC Class II in Melanoma Attracts Inflammatory Tumor-Specific CD4+ T- Cells, Which Dampen CD8+ T-cell Antitumor Reactivity. Cancer Res. 2015, 75, 3747–3759.
- Hemon, P.; Jean-Louis, F.; Ramgolam, K.; Brignone, C.; Viguier, M.; Bachelez, H.; Triebel, F.; Charron, D.; Aoudjit, F.; Al-Daccak, R.; et al. MHC Class II Engagement by Its Ligand LAG-3 (CD223) Contributes to Melanoma Resistance to Apoptosis. J. Immunol. 2011, 186, 5173–5183.
- Huard, B.; Prigent, P.; Tournier, M.; Bruniquel, D.; Triebel, F. CD4/major histocompatibility complex class II interaction analyzed with CD4- and lymphocyte activation gene-3 (LAG-3)-Ig fusion proteins. Eur. J. Immunol. 1995, 25, 2718–2721.
- Long, L.; Zhang, X.; Chen, F.; Pan, Q.; Phiphatwatchara, P.; Zeng, Y.; Chen, H. The promising immune checkpoint LAG-3: From tumor microenvironment to cancer immunotherapy. Genes Cancer 2018, 9, 176–189.
- Kouo, T.; Huang, L.; Pucsek, A.B.; Cao, M.; Solt, S.; Armstrong, T.; Jaffee, E. Galectin-3 Shapes Antitumor Immune Responses by Suppressing CD8+ T Cells via LAG-3 and Inhibiting Expansion of Plasmacytoid Dendritic Cells. Cancer Immunol. Res. 2015, 3, 412–423.
- Li, M.; Feng, Y.; Fang, S. Overexpression of ezrin and galectin-3 as predictors of poor prognosis of cervical cancer. Braz. J. Med. Biol. Res. 2017, 50, e5356.
- Lu, W.; Wang, J.; Yang, G.; Yu, N.; Huang, Z.; Xu, H.; Li, J.; Qiu, J.; Zeng, X.; Chen, S.; et al. Posttranscriptional regulation of Galectin-3 by miR-128 contributes to colorectal cancer progression. Oncotarget 2017, 8, 15242–15251.
- Chung, L.-Y.; Tang, S.-J.; Wu, Y.-C.; Sun, G.-H.; Liu, H.-Y.; Sun, K.-H. Galectin-3 augments tumor initiating property and tumorigenicity of lung cancer through interaction with β-catenin. Oncotarget 2014, 6, 4936–4952.
- Ming, Q.; Celias, D.P.; Wu, C.; Cole, A.R.; Singh, S.; Mason, C.; Dong, S.; Tran, T.H.; Amarasinghe, G.K.; Ruffell, B.; et al. LAG3 ectodomain structure reveals functional interfaces for ligand and antibody recognition. Nat. Immunol. 2022, 23, 1031–1041.
- Huard, B.; Mastrangeli, R.; Prigent, P.; Bruniquel, D.; Donini, S.; El-Tayar, N.; Maigret, B.; Dréano, M.; Triebel, F. Characterization of the major histocompatibility complex class II binding site on LAG-3 protein. Proc. Natl. Acad. Sci. USA 1997, 94, 5744–5749.
- Wang, J.; Sanmamed, M.F.; Datar, I.; Su, T.T.; Ji, L.; Sun, J.; Chen, L.; Chen, Y.; Zhu, G.; Yin, W.; et al. Fibrinogen-like Protein 1 Is a Major Immune Inhibitory Ligand of LAG-3. Cell 2019, 176, 334–347.e12.
- Xu, F.; Liu, J.; Liu, D.; Liu, B.; Wang, M.; Hu, Z.; Du, X.; Tang, L.; He, F. LSECtin Expressed on Melanoma Cells Promotes Tumor Progression by Inhibiting Antitumor T-cell Responses. Cancer Res. 2014, 74, 3418–3428.
- Zuazo, M.; Arasanz, H.; Bocanegra, A.; Chocarro, L.; Vera, R.; Escors, D.; Kagamu, H.; Kochan, G. Systemic CD4 immunity: A powerful clinical biomarker for PD-L1/PD-1 immunotherapy. EMBO Mol. Med. 2020, 12, e12706.
- Hernandez, C.; Arasanz, H.; Chocarro, L.; Bocanegra, A.; Zuazo, M.; Fernandez-Hinojal, G.; Blanco, E.; Vera, R.; Escors, D.; Kochan, G. Systemic Blood Immune Cell Populations as Biomarkers for the Outcome of Immune Checkpoint Inhibitor Therapies. Int. J. Mol. Sci. 2020, 21, 2411.
- Zuazo, M.; Arasanz, H.; Bocanegra, A.; Fernandez, G.; Chocarro, L.; Vera, R.; Kochan, G.; Escors, D. Systemic CD4 Immunity as a Key Contributor to PD-L1/PD-1 Blockade Immunotherapy Efficacy. Front. Immunol. 2020, 11, 586907.
- Zhang, X.; Zhao, H.; Shi, X.; Jia, X.; Yang, Y. Identification and validation of an immune-related gene signature predictive of overall survival in colon cancer. Aging 2020, 12, 26095–26120.
- Saka, D.; Gökalp, M.; Piyade, B.; Cevik, N.C.; Arik Sever, E.; Unutmaz, D.; Ceyhan, G.O.; Demir, I.E.; Asimgil, H. Mechanisms of T-Cell Exhaustion in Pancreatic Cancer. Cancers 2020, 12, 2274.
- Deng, W.-W.; Mao, L.; Yu, G.-T.; Bu, L.-L.; Ma, S.-R.; Liu, B.; Gutkind, J.S.; Kulkarni, A.B.; Zhang, W.-F.; Sun, Z.-J. LAG-3 confers poor prognosis and its blockade reshapes antitumor response in head and neck squamous cell carcinoma. OncoImmunology 2016, 5, e1239005.
- Datar, I.; Sanmamed, M.F.; Wang, J.; Henick, B.S.; Choi, J.; Badri, T.; Dong, W.; Mani, N.; Toki, M.; Mejías, L.D.; et al. Expression Analysis and Significance of PD-1, LAG-3, and TIM-3 in Human Non–Small Cell Lung Cancer Using Spatially Resolved and Multiparametric Single-Cell Analysis. Clin. Cancer Res. 2019, 25, 4663–4673.
- Wang, Y.; Dong, T.; Xuan, Q.; Zhao, H.; Qin, L.; Zhang, Q. Lymphocyte-Activation Gene-3 Expression and Prognostic Value in Neoadjuvant-Treated Triple-Negative Breast Cancer. J. Breast Cancer 2018, 21, 124–133.
- Zhu, Z.; Ye, J.; Ma, Y.; Hua, P.; Huang, Y.; Fu, X.; Li, D.; Yuan, M.; Xia, Z. Function of T regulatory type 1 cells is down-regulated and is associated with the clinical presentation of coronary artery disease. Hum. Immunol. 2018, 79, 564–570.
- Haudebourg, T.; Dugast, A.-S.; Coulon, F.; Usal, C.; Triebel, F.; Vanhove, B. Depletion of LAG-3 Positive Cells in Cardiac Allograft Reveals Their Role in Rejection and Tolerance. Transplantation 2007, 84, 1500–1506.
- Rodriguez, A. High HDL-Cholesterol Paradox: SCARB1-LAG3-HDL Axis. Curr. Atheroscler. Rep. 2021, 23, 5.
- Golden, D.; Kolmakova, A.; Sura, S.; Vella, A.T.; Manichaikul, A.; Wang, X.-Q.; Bielinski, S.J.; Taylor, K.D.; Chen, Y.-D.I.; Rich, S.S.; et al. Lymphocyte activation gene 3 and coronary artery disease. JCI Insight 2016, 1, e88628.
- Slevin, S.M.; Garner, L.C.; Lahiff, C.; Tan, M.; Wang, L.M.; Ferry, H.; Greenaway, B.; Lynch, K.; Geremia, A.; Hughes, S.; et al. Lymphocyte Activation Gene (LAG)-3 Is Associated With Mucosal Inflammation and Disease Activity in Ulcerative Colitis. J. Crohn’s Colitis 2020, 14, 1446–1461.
- Do, J.-S.; Visperas, A.; Sanogo, Y.O.; Bechtel, J.J.; Dvorina, N.; Kim, S.; Jang, E.; Stohlman, S.A.; Shen, B.; Fairchild, R.L.; et al. An IL-27/Lag3 axis enhances Foxp3+ regulatory T cell–suppressive function and therapeutic efficacy. Mucosal Immunol. 2015, 9, 137–145.
- Zhang, Z.; Duvefelt, K.; Svensson, F.; Masterman, T.; Jonasdottir, G.; Salter, H.; Emahazion, T.; Hellgren, D.; Falk, G.; Olsson, T.; et al. Two genes encoding immune-regulatory molecules (LAG3 and IL7R) confer susceptibility to multiple sclerosis. Genes Immun. 2005, 6, 145–152.
- Delmastro, M.M.; Styche, A.J.; Trucco, M.M.; Workman, C.J.; Vignali, D.A.; Piganelli, J.D. Modulation of Redox Balance Leaves Murine Diabetogenic TH1 T Cells “LAG-3-ing” Behind. Diabetes 2012, 61, 1760–1768.
- Bettini, M.; Szymczak-Workman, A.L.; Forbes, K.; Castellaw, A.H.; Selby, M.; Pan, X.; Drake, C.G.; Korman, A.J.; Vignali, D.A.A. Cutting Edge: Accelerated Autoimmune Diabetes in the Absence of LAG-3. J. Immunol. 2011, 187, 3493–3498.
- Doe, H.T.; Kimura, D.; Miyakoda, M.; Kimura, K.; Akbari, M.; Yui, K. Expression of PD-1/LAG-3 and cytokine production by CD4+T cells during infection withPlasmodiumparasites. Microbiol Immunol. 2016, 60, 121–131.
- Phillips, B.L.; Mehra, S.; Ahsan, M.H.; Selman, M.; Khader, S.; Kaushal, D. LAG3 Expression in Active Mycobacterium tuberculosis Infections. Am. J. Pathol. 2014, 185, 820–833.
- Graydon, C.G.; Balasko, A.L.; Fowke, K.R. Roles, function and relevance of LAG3 in HIV infection. PLOS Pathog. 2019, 15, e1007429.
- Jochems, S.P.; Jacquelin, B.; Tchitchek, N.; Busato, F.; Pichon, F.; Huot, N.; Liu, Y.; Ploquin, M.J.; Roché, E.; Cheynier, R.; et al. DNA methylation changes in metabolic and immune-regulatory pathways in blood and lymph node CD4 + T cells in response to SIV infections. Clin. Epigenetics 2020, 12, 188.
- Wuerdemann, N.; Pütz, K.; Eckel, H.; Jain, R.; Wittekindt, C.; Huebbers, C.U.; Sharma, S.J.; Langer, C.; Gattenlöhner, S.; Büttner, R.; et al. LAG-3, TIM-3 and VISTA Expression on Tumor-Infiltrating Lymphocytes in Oropharyngeal Squamous Cell Carcinoma—Potential Biomarkers for Targeted Therapy Concepts. Int. J. Mol. Sci. 2020, 22, 379.
- Li, F.-J.; Zhang, Y.; Jin, G.-X.; Yao, L.; Wu, D.-Q. Expression of LAG-3 is coincident with the impaired effector function of HBV-specific CD8+ T cell in HCC patients. Immunol. Lett. 2012, 150, 116–122.
- Roy, S.; Coulon, P.-G.; Srivastava, R.; Vahed, H.; Kim, G.J.; Walia, S.S.; Yamada, T.; Fouladi, M.A.; Ly, V.T.; Benmohamed, L. Blockade of LAG-3 Immune Checkpoint Combined With Therapeutic Vaccination Restore the Function of Tissue-Resident Anti-viral CD8+ T Cells and Protect Against Recurrent Ocular Herpes Simplex Infection and Disease. Front. Immunol. 2018, 9, 2922.
- Roy, S.; Coulon, P.-G.; Prakash, S.; Srivastava, R.; Geertsema, R.; Dhanushkodi, N.; Lam, C.; Nguyen, V.; Gorospe, E.; Nguyen, A.M.; et al. Blockade of PD-1 and LAG-3 Immune Checkpoints Combined with Vaccination Restores the Function of Antiviral Tissue-Resident CD8 + T RM Cells and Reduces Ocular Herpes Simplex Infection and Disease in HLA Transgenic Rabbits. J. Virol. 2019, 93, e00827-19.
- Richter, K.; Agnellini, P.; Oxenius, A. On the role of the inhibitory receptor LAG-3 in acute and chronic LCMV infection. Int. Immunol. 2009, 22, 13–23.
- Anderson, A.C.; Joller, N.; Kuchroo, V.K. Lag-3, Tim-3, and TIGIT: Co-inhibitory Receptors with Specialized Functions in Immune Regulation. Immunity 2016, 44, 989–1004.
- McLane, L.M.; Abdel-Hakeem, M.S.; Wherry, E.J. CD8 T Cell Exhaustion during Chronic Viral Infection and Cancer. Annu. Rev. Immunol. 2019, 37, 457–495.
- Chocarro, L.; Blanco, E.; Arasanz, H.; Fernandez-Rubio, L.; Echaide, M.; Garnica, M.; Ramos, P.; Piñeiro, S.; Kochan, G.; Escors, D. LAG-3 Role in Infection. In Proceedings of the 1st International Electronic Conference on Molecular Sciences: Druggable Targets of Emerging Infectious Disease, 31 August 2021; Volume 2021.
- Chocarro, L.; Blanco, E.; Arasanz, H.; Fernandez-Rubio, L.; Echaide, M.; Garnica, M.; Ramos, P.; Piñeiro, S.; Kochan, G.; Escors, D. LAG-3 Role in Cardiovascular Diseases. In Proceedings of the MOL2NET’22, Conference on Molecular, Biomedical & Computational Sciences and Engineering, Basel, Switzerland, 23 March 2022.
- Chocarro, L.; Blanco, E.; Arasanz, H.; Fernandez-Rubio, L.; Echaide, M.; Garnica, M.; Ramos, P.; Piñeiro, S.; Kochan, G.; Escors, D. LAG-3 Role in Inflammatory Diseases. In Proceedings of the MOL2NET’22, Conference on Molecular, Biomedical & Computational Sciences and Engineering, Basel, Switzerland, 23 March 2022.
- Chocarro, L.; Blanco, E.; Arasanz, H.; Fernandez-Rubio, L.; Echaide, M.; Garnica, M.; Ramos, P.; Piñeiro, S.; Kochan, G.; Escors, D. LAG-3 Role in Neurological Diseases. In Proceedings of the MOL2NET’22, Conference on Molecular, Biomedical & Computational Sciences and Engineering, Basel, Switzerland, 23 March 2022.
- Chocarro, L.; Blanco, E.; Arasanz, H.; Fernandez-Rubio, L.; Bocanegra, A.; Echaide, M.; Garnica, M.; Ramos, P.; Piñeiro, S.; Kochan, G.; et al. Role of the next-generation immune checkpoint LAG-3 in response and resistance to cancer immunotherapy. In Proceedings of the MOL2NET’22, Conference on Molecular, Biomedical & Computational Sciences and Engineering, Basel, Switzerland, 23 March 2022.
- RELATLIMAB. Available online: https://drugs.ncats.io/substance/AF75XOF6W3 (accessed on 1 July 2022).
- Ascierto, P.A.; Melero, I.; Bhatia, S.; Bono, P.; Sanborn, R.E.; Lipson, E.J.; Callahan, M.K.; Gajewski, T.; Gomez-Roca, C.A.; Hodi, F.S.; et al. Initial efficacy of anti-lymphocyte activation gene-3 (anti–LAG-3; BMS-986016) in combination with nivolumab (nivo) in pts with melanoma (MEL) previously treated with anti–PD-1/PD-L1 therapy. J. Clin. Oncol. 2017, 35, 9520.
- Lipson, E.; Long, G.; Tawbi, H.; Schadendorf, D.; Atkinson, V.; Maurer, M.; Simonsen, K.; Harbison, C.; Hodi, F. CA224-047: A randomized, double-blind, phase II/III study of relatlimab (anti–LAG-3) in combination with nivolumab (anti–PD-1) versus nivolumab alone in previously untreated metastatic or unresectable melanoma. Ann. Oncol. 2018, 29, viii464–viii465.
- Ascierto, P.A.; Bono, P.; Bhatia, S.; Melero, I.; Nyakas, M.S.; Svane, I.-M.; Larkin, J.; Gomez-Roca, C.; Schadendorf, D.; Dummer, R.; et al. Efficacy of BMS-986016, a monoclonal antibody that targets lymphocyte activation gene-3 (LAG-3), in combination with nivolumab in pts with melanoma who progressed during prior anti–PD-1/PD-L1 therapy (mel prior IO) in all-comer and biomarker-enriched populations. Ann. Oncol. 2017, 28, v611–v612.
- Sordo-Bahamonde, C.; Lorenzo-Herrero, S.; González-Rodríguez, A.P.; Payer, Á.R.; González-García, E.; López-Soto, A.; Gonzalez, S. LAG-3 Blockade with Relatlimab (BMS-986016) Restores Anti-Leukemic Responses in Chronic Lymphocytic Leukemia. Cancers 2021, 13, 2112.
- Clinical Trials Register—Search for 2018-003278-28. Available online: https://www.clinicaltrialsregister.eu/ctr-search/search?query=2018-003278-28 (accessed on 1 July 2022).
- Ellis, J.; Marks, D.J.; Srinivasan, N.; Barrett, C.; Hopkins, T.G.; Richards, A.; Fuhr, R.; Albayaty, M.; Coenen, M.; Liefaard, L.; et al. Depletion of LAG-3 + T Cells Translated to Pharmacology and Improvement in Psoriasis Disease Activity: A Phase I Randomized Study of mAb GSK2831781. Clin. Pharmacol. Ther. 2020, 109, 1293–1303.
- Savitsky, D.; Ward, R.; Riordan, C.; Mundt, C.; Jennings, S.; Connolly, J.; Findeis, M.; Sanicola, M.; Underwood, D.; Nastri, H.; et al. Abstract 3819: INCAGN02385 is an antagonist antibody targeting the co-inhibitory receptor LAG-3 for the treatment of human malignancies. Cancer Res. 2018, 78, 3819.
- IERAMILIMAB. Available online: https://drugs.ncats.io/substance/OI8P0SFD4R (accessed on 1 July 2022).
- Lin, C.-C.; Garralda, E.; Schöffski, P.; Hong, D.; Siu, L.; Martin, M.; Maur, M.; Hui, R.; Soo, R.; Chiu, J.; et al. 387 A Phase II, multicenter study of the safety and efficacy of LAG525 in combination with spartalizumab in patients with advanced malignancies. J. Immunother. Cancer 2020, 8, A412.
- Uboha, N.V.; Milhem, M.M.; Kovacs, C.; Amin, A.; Magley, A.; Das Purkayastha, D.; Piha-Paul, S.A. Phase II study of spartalizumab (PDR001) and LAG525 in advanced solid tumors and hematologic malignancies. J. Clin. Oncol. 2019, 37, 2553.
- Hong, D.S.; Schoffski, P.; Calvo, A.; Sarantopoulos, J.; De Olza, M.O.; Carvajal, R.D.; Prawira, A.; Kyi, C.; Esaki, T.; Akerley, W.L.; et al. Phase I/II study of LAG525 ± spartalizumab (PDR001) in patients (pts) with advanced malignancies. J. Clin. Oncol. 2018, 36, 3012.
- Garralda, E.; Sukari, A.; Lakhani, N.J.; Patnaik, A.; Lou, Y.; Im, S.-A.; Golan, T.; Geva, R.; Wermke, M.; De Miguel, M.; et al. A phase 1 first-in-human study of the anti-LAG-3 antibody MK4280 (favezelimab) plus pembrolizumab in previously treated, advanced microsatellite stable colorectal cancer. J. Clin. Oncol. 2021, 39, 3584.
- Gregory, G.P.; Zinzani, P.L.; Palcza, J.; Healy, J.A.; Orlowski, R.J.; Nahar, A.; Armand, P. Abstract CT106: Anti-LAG-3 antibody MK-4280 in combination with pembrolizumab for the treatment of hematologic malignancies: A Phase I/II study. Cancer Res. 2019, 79, CT106.
- FAVEZELIMAB. Available online: https://drugs.ncats.io/substance/H1396W7D1H (accessed on 1 July 2022).
- Burova, E.; Hermann, A.; Dai, J.; Ullman, E.; Halasz, G.; Potocky, T.; Hong, S.; Liu, M.; Allbritton, O.; Woodruff, A.; et al. Preclinical Development of the Anti-LAG-3 Antibody REGN3767: Characterization and Activity in Combination with the Anti-PD-1 Antibody Cemiplimab in Human PD-1xLAG-3–Knockin Mice. Mol. Cancer Ther. 2019, 18, 2051–2062.
- FIANLIMAB. Available online: https://drugs.ncats.io/substance/OX5LRQ5H6K (accessed on 1 July 2022).
- Hamid, O.; Wang, D.; Kim, T.M.; Kim, S.-W.; Lakhani, N.J.; Johnson, M.L.; Groisberg, R.; Papadopoulos, K.P.; Kaczmar, J.M.; Middleton, M.R.; et al. Clinical activity of fianlimab (REGN3767), a human anti-LAG-3 monoclonal antibody, combined with cemiplimab (anti-PD-1) in patients (pts) with advanced melanoma. J. Clin. Oncol. 2021, 39, 9515.
- Nanda, R.; Liu, M.C.; Yau, C.; Shatsky, R.; Pusztai, L.; Wallace, A.; Chien, A.J.; Forero-Torres, A.; Ellis, E.; Han, H.; et al. Effect of Pembrolizumab Plus Neoadjuvant Chemotherapy on Pathologic Complete Response in Women With Early-Stage Breast Cancer: An Analysis of the Ongoing Phase 2 Adaptively Randomized I-SPY2 Trial. JAMA Oncol. 2020, 6, 676–684.
- Papadopoulos, K.P.; Lakhani, N.J.; Johnson, M.L.; Park, H.; Wang, D.; Yap, T.; Dowlati, A.; Maki, R.G.; Lynce, F.; Ulahannan, S.V.; et al. First-in-human study of REGN3767 (R3767), a human LAG-3 monoclonal antibody (mAb), ± cemiplimab in patients (pts) with advanced malignancies. J. Clin. Oncol. 2019, 37, 2508.
- Spreafico, A.; Janku, F.; Rodon, J.A.; Tolcher, A.W.; Chandana, S.R.; Oliva, M.; Musalli, S.; Knauss, L.; Kragh, L.; Alifrangis, L.; et al. A phase I study of Sym021, an anti-PD-1 antibody (Ab), alone and in combination with Sym022 (anti-LAG-3) or Sym023 (anti-TIM-3). Ann. Oncol. 2019, 30.
- Lakhani, N.; Spreafico, A.; Tolcher, A.; Rodon, J.; Janku, F.; Chandana, S.; Oliva, M.; Sharma, M.; Abdul-Karim, R.; Hansen, U.; et al. 1019O Phase I studies of Sym021, an anti-PD-1 antibody, alone and in combination with Sym022 (anti-LAG-3) or Sym023 (anti-TIM-3). Ann. Oncol. 2020, 31, S704.
- Ghosh, S.; Sharma, G.; Travers, J.; Kumar, S.; Choi, J.; Jun, H.T.; Kehry, M.; Ramaswamy, S.; Jenkins, D. TSR-033, a novel therapeutic antibody targeting LAG-3, enhances T-cell function and the activity of PD-1 blockade in vitro and in vivo. Mol. Cancer Ther. 2019, 18, 632–641.
- Park, E.; Kim, H.; Sung, E.; Jung, U.; Hong, Y.; Lee, H.; Ko, M.; Park, Y.; Park, C.K.; Kim, S.J.; et al. Abstract 1633: ABL501, PD-L1 x LAG-3, a bispecific antibody promotes enhanced human T cell activation through targeting simultaneously two immune checkpoint inhibitors, LAG-3 and PD-L1. Cancer Res. 2021, 81, 1633.
- Sung, E.; Ko, M.; Won, J.-Y.; Jo, Y.; Park, E.; Kim, H.; Choi, E.; Jung, U.-J.; Jeon, J.; Kim, Y.; et al. LAG-3xPD-L1 bispecific antibody potentiates antitumor responses of T cells through dendritic cell activation. Mol. Ther. 2022, 30, S1525.
- Jiang, H.; Ni, H.; Zhang, P.; Guo, X.; Wu, M.; Shen, H.; Wang, J.; Wu, W.; Wu, Z.; Ding, J.; et al. PD-L1/LAG-3 bispecific antibody enhances tumor-specific immunity. OncoImmunology 2021, 10, 1943180.
- Powderly, J.D.; Hurwitz, H.; Ryan, D.P.; Laheru, D.A.; Pandya, N.B.; Lohr, J.; Moore, P.A.; Bonvini, E.; Wigginton, J.M.; Crocenzi, T.S. A phase 1, first-in-human, open label, dose escalation study of MGD007, a humanized gpA33 × CD3 DART molecule, in patients with relapsed/refractory metastatic colorectal carcinoma. J. Clin. Oncol. 2016, 34, TPS3628.
- Hedvat, M.; Bonzon, C.; Bernett, M.J.; Moore, G.L.; Avery, K.; Rashid, R.; Nisthal, A.; Schubert, S.; Varma, R.; Lee, S.-H.; et al. Abstract 2784: Simultaneous checkpoint-checkpoint or checkpoint-costimulatory receptor targeting with bispecific antibodies promotes enhanced human T cell activation. Cancer Res. 2018, 78, 2784.
- Everett, K.L.; Kraman, M.; Wollerton, F.P.; Zimarino, C.; Kmiecik, K.; Gaspar, M.; Pechouckova, S.; Allen, N.L.; Doody, J.F.; Tuna, M. Generation of Fcabs targeting human and murine LAG-3 as building blocks for novel bispecific antibody therapeutics. Methods 2018, 154, 60–69.
- Kraman, M.; Faroudi, M.; Allen, N.L.; Kmiecik, K.; Gliddon, D.; Seal, C.; Koers, A.; Wydro, M.M.; Batey, S.; Winnewisser, J.; et al. FS118, a Bispecific Antibody Targeting LAG-3 and PD-L1, Enhances T-Cell Activation Resulting in Potent Antitumor Activity. Clin. Cancer Res. 2020, 26, 3333–3344.
- Yap, T.; Wong, D.; Hu-Lieskovan, S.; Papadopoulos, K.; Morrow, M.; Grabowska, U.; Gliddon, D.; Holz, J.-B.; LoRusso, P. 395 A first-in-human study of FS118, a tetravalent bispecific antibody targeting LAG-3 and PD-L1, in patients with advanced cancer and resistance to PD-(L)1 therapy. J. ImmunoTherapy Cancer 2020, 8, A420.
- Yap, T.; Papadopoulos, K.P.; Lorusso, P.; Wong, D.J.; Hu-Lieskovan, S.; Holz, J.-B. A first-in-human phase I study of FS118, an anti-LAG-3/PD-L1 bispecific antibody in patients with solid tumors that have progressed on prior PD-1/PD-L1 therapy. J. Clin. Oncol. 2019, 37, TPS2652.
- Crescendo Biologics and Cancer Research UK Sign Clinical Development Partnership to Develop CB213, a Novel Bispecific Humabody® Therapeutic | Business Wire. Available online: https://www.businesswire.com/news/home/20200505005080/en/Crescendo-Biologics-and-Cancer-Research-UK-sign-Clinical-Development-Partnership-to-develop-CB213-a-novel-bispecific-Humabody%C2%AE-therapeutic (accessed on 1 July 2022).
- Edwards, C.J.; Sette, A.; Cox, C.; Di Fiore, B.; Wyre, C.; Sydoruk, D.; Yadin, D.; Hayes, P.; Stelter, S.; Bartlett, P.D.; et al. The multi-specific VH-based Humabody CB213 co-targets PD1 and LAG3 on T cells to promote anti-tumour activity. Br. J. Cancer 2021, 126, 1168–1177.
- Haftcheshmeh, S.M.; Zamani, P.; Mashreghi, M.; Nikpoor, A.R.; Tavakkol-Afshari, J.; Jaafari, M.R. Immunoliposomes bearing lymphocyte activation gene 3 fusion protein and P5 peptide: A novel vaccine for breast cancer. Biotechnol. Prog. 2020, 37, e3095.
- Cappello, P.; Triebel, F.; Iezzi, M.; Caorsi, C.; Quaglino, E.; Lollini, P.L.; Amici, A.; Di Carlo, E.; Musiani, P.; Giovarelli, M.; et al. LAG-3 Enables DNA Vaccination to Persistently Prevent Mammary Carcinogenesis in HER-2/neu Transgenic BALB/c. Cancer Res. 2003, 63, 2518–2525.
- Fougeray, S.; Brignone, C.; Triebel, F. A soluble LAG-3 protein as an immunopotentiator for therapeutic vaccines: Preclinical evaluation of IMP321. Vaccine 2006, 24, 5426–5433.
- Andreae, S.; Piras, F.; Burdin, N.; Triebel, F. Maturation and Activation of Dendritic Cells Induced by Lymphocyte Activation Gene-3 (CD223). J. Immunol. 2002, 168, 3874–3880.
- Brignone, C.; Grygar, C.; Marcu, M.; Schäkel, K.; Triebel, F. A soluble form of lymphocyte activation gene-3 (IMP321) induces activation of a large range of human effector cytotoxic cells. J. Immunol. 2007, 179, 4202–4211.
- El Mir, S.; Triebel, F. A Soluble Lymphocyte Activation Gene-3 Molecule Used as a Vaccine Adjuvant Elicits Greater Humoral and Cellular Immune Responses to Both Particulate and Soluble Antigens. J. Immunol. 2000, 164, 5583–5589.
- Brignone, C.; Grygar, C.; Marcu, M.; Perrin, G.; Triebel, F. IMP321 (sLAG-3), an immunopotentiator for T cell responses against a HBsAg antigen in healthy adults: A single blind randomised controlled phase I study. J. Immune Based Ther. Vaccines 2007, 5, 5.
- Brignone, C.; Grygar, C.; Marcu, M.; Perrin, G.; Triebel, F. IMP321 (sLAG-3) safety and T cell response potentiation using an influenza vaccine as a model antigen: A single-blind phase I study. Vaccine 2007, 25, 4641–4650.
- Casati, C.; Camisaschi, C.; Rini, F.; Arienti, F.; Rivoltini, L.; Triebel, F.; Parmiani, G.; Castelli, C. Soluble Human LAG-3 Molecule Amplifies the In vitro Generation of Type 1 Tumor-Specific Immunity. Cancer Res. 2006, 66, 4450–4460.
- Advanced Melanoma | OpdualagTM (Nivolumab and Relatlimab-Rmbw). Available online: https://www.opdualag.com/ (accessed on 1 July 2022).
- FDA Approves Opdualag for Unresectable or Metastatic Melanoma. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-opdualag-unresectable-or-metastatic-melanoma (accessed on 1 July 2022).




