Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Luca Bertolaccini | -- | 3020 | 2022-08-01 21:44:41 | | | |
| 2 | Peter Tang | Meta information modification | 3020 | 2022-08-02 04:20:35 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Bertolaccini, L.; Mohamed, S.; Bardoni, C.; Iacono, G.L.; Mazzella, A.; Guarize, J.; Spaggiari, L. Interdisciplinary Management of Lung Cancer in European Community. Encyclopedia. Available online: https://encyclopedia.pub/entry/25745 (accessed on 07 February 2026).
Bertolaccini L, Mohamed S, Bardoni C, Iacono GL, Mazzella A, Guarize J, et al. Interdisciplinary Management of Lung Cancer in European Community. Encyclopedia. Available at: https://encyclopedia.pub/entry/25745. Accessed February 07, 2026.
Bertolaccini, Luca, Shehab Mohamed, Claudia Bardoni, Giorgio Lo Iacono, Antonio Mazzella, Juliana Guarize, Lorenzo Spaggiari. "Interdisciplinary Management of Lung Cancer in European Community" Encyclopedia, https://encyclopedia.pub/entry/25745 (accessed February 07, 2026).
Bertolaccini, L., Mohamed, S., Bardoni, C., Iacono, G.L., Mazzella, A., Guarize, J., & Spaggiari, L. (2022, August 01). Interdisciplinary Management of Lung Cancer in European Community. In Encyclopedia. https://encyclopedia.pub/entry/25745
Bertolaccini, Luca, et al. "Interdisciplinary Management of Lung Cancer in European Community." Encyclopedia. Web. 01 August, 2022.
Copy Citation
Lung cancer continues to be the largest cause of cancer-related mortality among men and women globally, accounting for around 27% of all cancer-related deaths. Recent advances in lung cancer medicines, particularly for non-small-cell lung cancer (NSCLC), have increased the need for multidisciplinary disease care, thereby enhancing patient outcomes and quality of life. Different studies in the European community have evaluated the impact of multidisciplinary care on outcomes for lung cancer patients, including its impact on survival, adherence to guideline treatment, utilization of all treatment modalities, timeliness of treatment, patient satisfaction, quality of life, and referral to palliative care.
multidisciplinary management
tailored therapy
lung cancer
1. Introduction
Lung cancer remains the leading cause of cancer-related mortality among men and women worldwide, accounting for approximately 27% of all cancer-related deaths. The recent advancements in therapies for lung cancer, especially for non-small-cell lung cancer (NSCLC), have created a greater demand for multidisciplinary management of this disease, improving outcomes and quality of life. Different treatment options have been described, including surgery, radiation therapy, systemic therapy (chemotherapy, targeted therapies, or immunotherapy), or a combination of two or three modalities may be used. When needed, a palliative approach to treatment may be appropriate for patients with advanced disease, significant comorbidities, or poor performance status. Due to these multiple treatment options available, different specialists need efficient collaboration to develop a more specific patient-centred management plan. One of the ten goals regarding multidisciplinary cancer management outlined in the Quality Cancer Care Statement by the American Society of Clinical Oncology (ASCO)—the European Society for Medical Oncology (ESMO) states that the “Optimal treatment of cancer should be provided by a team that includes, where appropriate, multidisciplinary medical expertise composed of medical oncologists, surgical oncologists, radiation oncologists, palliative care experts, as well as oncology nurses and social workers. Patients should also have access to counselling for their psychological, nutritional, and other needs.” [1].
In July 2007, at the Lisbon roundtable held during the Europe meeting, under the Portuguese Presidency, one of the conclusions stated was that a multidisciplinary team approach to lung cancer care is required for European lung cancer centres [2].
Another similar statement was recommended by the American Thoracic Society (ATS) and the European Respiratory Society (ERS), which says that all centres offering thoracic oncology services should have multidisciplinary clinics and a thoracic oncology multidisciplinary meeting [3].
2. Interdisciplinary Service
An active multidisciplinary lung cancer service is an essential aspect of multidisciplinary lung cancer care, with particular attention to patient-focused care and an attempt to improve the patient journey through collaboration, communication, and streamlining of diagnostics and treatment [4]. In order to have an efficient multidisciplinary lung cancer service, interested physicians should be achieved amongst members of the hospital or community healthcare team with relevant expertise. The interdisciplinary tumour board members must attend meetings frequently to identify lung cancer patients that could benefit from multidisciplinary evaluation and management [5]. Inappropriate work scheduling and time management can compromise physicians’ attendance at multidisciplinary meetings. They can impact the quality of multidisciplinary discussions, and this can happen, for example, through daily clinical ward duties.
For this reason, all members should have dedicated time for multidisciplinary meetings. All other activities should be planned appropriately, including additional time to cover administrative duties that may arise from tumour boards [6][7]. To ensure tumour board efficiency, a competent multidisciplinary meeting lead physician who is an established clinician in the hospital from any speciality among those in the team must be defined. The team leader must obtain opinions from different specialists to assess the meeting’s overall quality and to provide documentation of adequate management plans [8][9][10]. The leader and the members should work closely to optimise patient management and avoid service disruption. Limits to an efficient multidisciplinary meeting can be poor leadership, insufficient teamwork, and time pressure [11][12]. In order to solve this issue, thoracic oncology training in Europe to ensure competent candidates was introduced by the European Respiratory Society as HERMES (Harmonising Education in Respiratory Medicine for European Specialists) European Curriculum recommendations. This program shall train efficient thoracic oncology leads enrolled in any speciality [13][14]. Generally, communication has a crucial role in the smooth running of the entire work, either for the relationship between tumour board members and between clinicians and the patient, the family, and the caregivers, and specific communications skills training is required to explain clearly the different steps of the treatment journey [15]. Consultation and a final agreement with all tumour board members are advised before a treatment plan, considering the complex and increasing rate of multimodality therapy. The quality of the discussion in the multidisciplinary team may be influenced by several factors, such as poor leadership and lack of time and information technology (IT) support, which may be essential, especially in many cases. In the last two years, due to the recent coronavirus disease 2019 (COVID-19) pandemic, multidisciplinary meetings have become gradually virtual to avoid direct contact between multiple clinicians to contain the spread of contagion. For this reason, virtual multidisciplinary team meetings became the standard of care to review patient cases at a safe distance. In this view, a lack of resources about information technology may slow the tumour board meeting due to an incorrect projection of the exams and pathology results on the screen [16].
For this latter, ESMO has published new guidelines and recommendations on managing and treating lung cancer patients in the era of COVID-19 [17].
3. Multidisciplinary Meeting Roles and Responsibilities
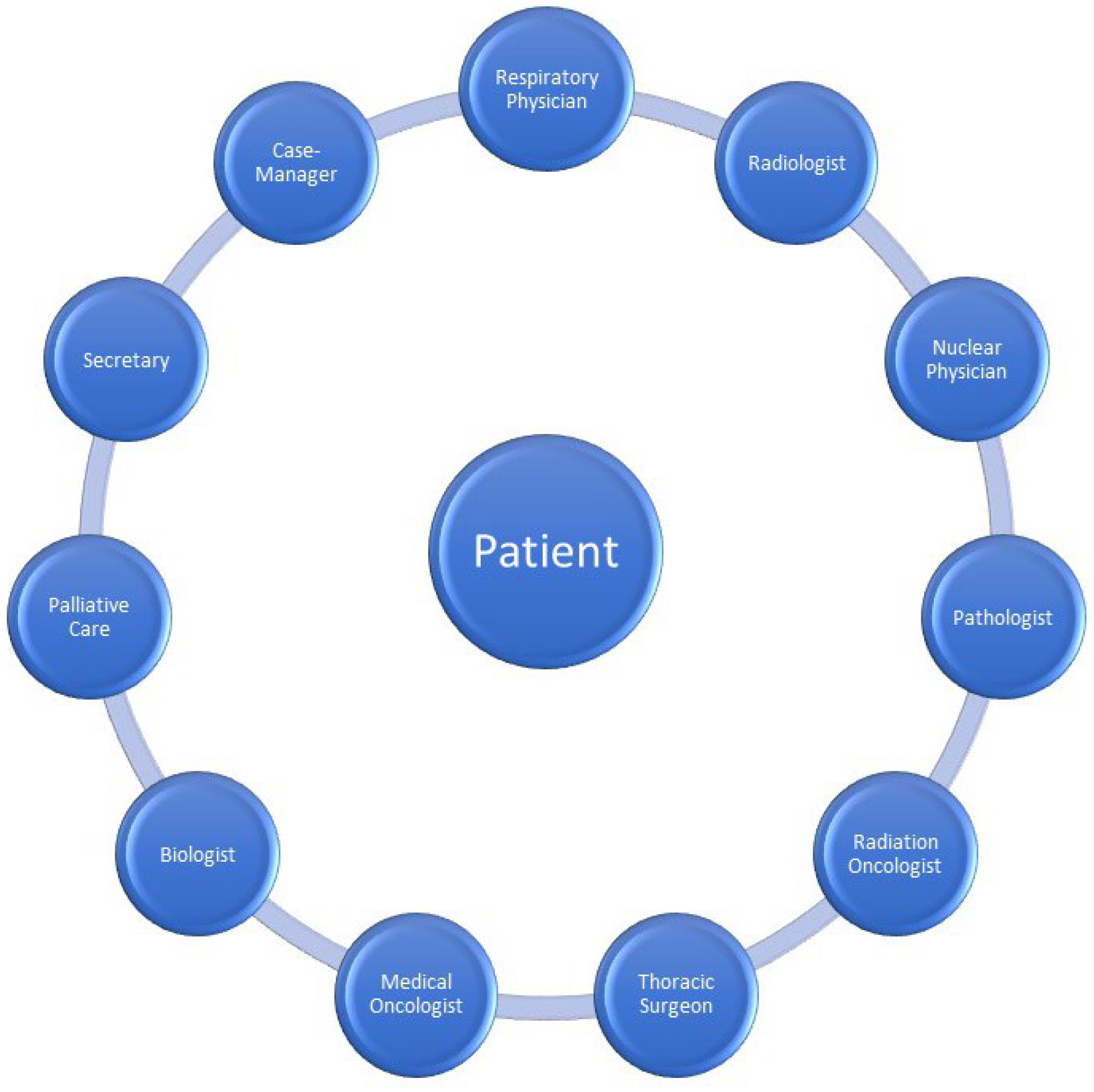
Multidisciplinary meetings include clinicians and other health professionals. Clinicians involved in lung cancer multidisciplinary meetings should include a thoracic surgeon, radiation oncologist, medical oncologist, respiratory physician, pathologist, nuclear medicine physician, radiologist, and palliative care physician [8][18][19][20]. Other tumour board members could include interventional pulmonologists, clinical nurse specialists, MDM coordinators, psychologists, clinical trials coordinators, nutritionists, physical and occupational therapists, trainees and medical students. Every meeting member should attend on schedule most of the meetings. At least one team member should know the patient case and be present for the discussion and decision-making process.
Moreover, to ensure diversity of opinions and optimal decisions, at least a minimum of one attending member from each speciality is necessary. In case of attendance is not possible, arrangements should be made to ensure that all decisions are made considering all required specialities. Additionally, late multidisciplinary meeting case additions should be avoided unless clinically urgent. This can provide insufficient time to prepare these cases [19][20]. The frequency of multidisciplinary meetings varies between institutions. At least one multidisciplinary meeting takes place weekly in high-volume centres, unlike small institutions where MDM may not be hosted regularly due to a small number of specialists, especially for rare tumours such as mesothelioma or sarcomas. An irregular frequency of multidisciplinary meetings is associated with more comprehensive time management for definitive treatment. The frequency of tumour boards is essential, especially for rapidly progressive neoplasms such as small-cell lung cancer. There should be a rapid referral to the oncologists for immediate treatment and management without waiting for a multidisciplinary meeting. In this group of patients, the specialists must make a quick decision in the best interest because the risk of missing the right time to be treated is higher than waiting for a potential multidisciplinary meeting [19][20]. Administrative support by the MDM coordinator plays an essential role in a functional and efficient multidisciplinary meeting. (Figure 1).
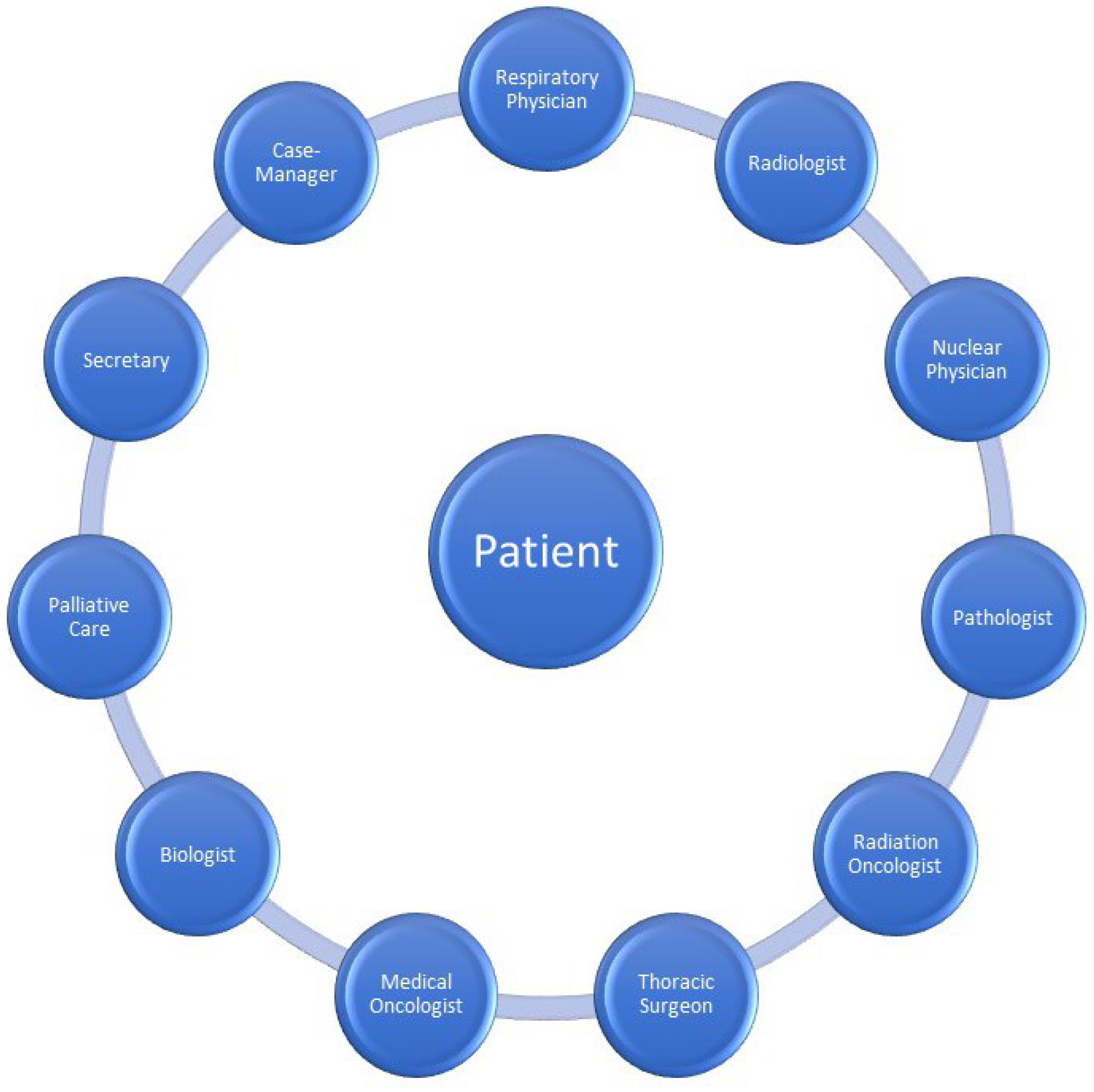
Figure 1. All the specialists contribute to the interdisciplinary management of lung cancer.
4. Impact on Survival
In the European community, the influence of multidisciplinary care on lung cancer survival has been recorded in very few single-centre retrospective studies. Price et al. (2002) and Forrest et al. (2005) [21][22] were the first groups from Scotland and the United Kingdom to publish studies nearly twenty years ago. Price et al. published a retrospective analysis of 542 NSCLC patients aged 70 and older. A total of 262 were treated without a multidisciplinary meeting, while 280 were addressed prior to a specific treatment at a multidisciplinary meeting (MDM). The MDMs included three specialized respiratory oncologists three times every week. In this study, they demonstrated a statistically significant improvement in 1-year survival from 18.3 percent to 23.5 percent (p = 0.049) of elderly NSCLC patients over the age of 70 referred for radiotherapy following the establishment of an MDM, as well as an increase in the rate of curative radiotherapy and a decrease in the rate of palliative thoracic radiotherapy [23].
In contrast, Forrest et al. conducted a retrospective research at a single institution with 243 inoperable NSCLC (stage III/IV) patients, of which 156 were addressed before to a specific treatment in an MDM and 167 were treated without an MDM. At a single tertiary hospital, the MDMs have included two respiratory physicians, two surgeons, a medical oncologist, a clinical oncologist, a palliative care physician, a radiologist, and a lung cancer nurse. In this study, this group found a statistically significant improvement in the median survival of MDM patients who received increasing rates of active treatment and chemotherapy, but not radiotherapy with curative or palliative purpose [21]. In a more recent retrospective cohort analysis from an Italian group, Tamburini et al. reported a comparable outcome based on 477 NSCLC patients treated with surgery between January 2008 and December 2015, of whom 231 were MDM patients and 246 were seen prior to the establishment of the MDM. A surgeon, medical oncologist, radiation oncologist, nuclear medicine physician, pathologist, radiologist, and lung cancer coordinator attended the MDM’s weekly lung cancer meeting [22]. Tamburini et al. observed a statistically significant improvement in survival after one year for patients with early-stage NSCLC who underwent lung resection, 92 percent in the MDM group against 82 percent in the pre-MDM group [22].
In contrast, Murray et al. (United Kingdom) published in 2003 a randomized controlled trial in which there was no difference in survival between patients assigned to the two arms, either overall or among those getting curative treatment [24]. From October 1998 to January 2001, 88 patients with probable lung cancer were evaluated in this study, 45 in the central MDM arm and 43 in the traditional arm. A thoracic surgeon, respiratory physicians, medical oncologists, clinical oncologists, palliative care physicians, and a study coordinator were present at MDMs. In addition, there was a trend toward more curative treatment in the MDM arm. The non-cancer diagnosis of about 30% of patients in this trial and the small sample size are crucial limitations that must be acknowledged [24]. According to the stage of cancer, Forrest et al. and Tamburini et al. have studied the impact of multidisciplinary care.
In addition, the same studies have assessed the impact of a given stage on a cohort of patients at all phases. The majority of MDM patients arrived with stage III disease, whereas the majority of non-MDM patients presented with stage IV disease. Forrest et al. showed a statistically significant improvement in the median survival of patients with inoperable stage III/IV NSCLC following the formation of an MDM at a single centre, 6.6 months versus 3.2 months [21][22]. The distribution of these two groups of patients with inoperable stage III and IV disease was comparable, but again, the relatively small number of patients represents a limitation of this study. Neither patient performance status nor co-morbidities were accounted for in this investigation. Considering these few studies, there is little evidence that multidisciplinary meetings have a major impact on lung cancer survival. According to numerous studies, interdisciplinary care significantly improves patients’ survival. However, these investigations are restricted by their retrospective methodology, small sample size, and inability to account for confounding variables that influence the survival of this patient population. Statistical analysis of potential imbalances in prognostic factors between the main two-arm groups has revealed that the group receiving multidisciplinary care has a greater chance of survival.
5. Treatment Utilisation
The most crucial purpose of multidisciplinary meetings, the cooperation between different specialised professionals, is to develop an appropriate management plan and determine the most specific treatment for every patient. Murray et al., in their randomised trial, have reported that patients discussed in a multidisciplinary setting are more likely to receive curative treatment, including all treatment modalities. Patients discussed in a multidisciplinary setting recorded twice as likely to have chemotherapy, especially with palliative intent. In this small-size study, there was no significant difference in the use of curative treatment [24]. On the other hand, Forrest et al. stated that a statistically significant number of patients not managed in a multidisciplinary setting were more likely to receive the best supportive care only [21]. This difference may reflect that the non-discussed patients generally have poor performance status with multiple comorbidities, are older, and have more advanced diseases.
5.1. Surgery
Study to study, the effect of multidisciplinary meetings on surgical utilization differs. Davison et al. performed a modest retrospective single-institution analysis on 62 patients selected between November 2000 and November 2001, 50 of whom had undergone thoracotomy three years prior to the MDM. In this instance, biweekly interdisciplinary discussions were held by teleconference between a regional centre and a metropolitan tertiary hospital. A thoracic surgeon, respiratory physicians, medical oncologists, clinical oncologists, radiologists, and a lung cancer nurse coordinator were present at MDMs [25]. Patients initially seen in a centre with a department of thoracic surgery experienced a 30% increase in surgery rates after the establishment of a teleconferencing multidisciplinary meeting (MDM) between a regional and tertiary referral centre, presumably because this provided a more direct referral pathway for patients and physicians [26]. In their retrospective observational analysis, Tamburini et al. observed an increase in the frequency of MDM patients receiving mediastinal staging prior to surgery [22]. Overall, individuals having access to thoracic surgery or an established referral channel for thoracic surgeon evaluation who are discussed in a multidisciplinary context have a higher surgical use rate, particularly for stage I and II NSCLC.
5.2. Radiation Therapy
In their two retrospective analyses [21][23], Price et al. and Forrest evaluated two categories of radiation-treated patients: curative and palliative. The findings of these trials following multidisciplinary care varied. Forrest et al. [21] examined inoperable NSCLC patients and found comparable rates of curative or palliative radiation therapy before and after establishing an MDM. The sample size of patients, particularly those receiving curative radiation therapy, was however modest. Price et al. discovered a significant increase in curative thoracic radiation therapy and a decrease in palliative thoracic radiation therapy in older patients in a multidisciplinary environment [23] three years earlier. Recent advances in radiation therapy and improved accuracy of radiation delivery have contributed to observed improvements in patient survival over the past decade, making radiation therapy a cornerstone of contemporary lung cancer treatment alongside surgery, chemotherapy, immunotherapy, and targeted therapies. These developments have led to the evolution of radiation therapy into a treatment recommended by guidelines for early-stage and locally progressed lung cancer, but not for small-cell lung cancer. Examples of this enhanced survival include the lowering rates of non-treatment in early-stage lung cancer in population studies and the survival benefits observed in trials including immunotherapy after chemotherapy and radiation therapy in locally advanced NSCLC.
In addition, although radiation therapy has traditionally been utilized for the palliation of advanced lung cancer, it is increasingly being used as a locally ablative treatment for patients with oligometastatic illness. As a result, therapeutic options are getting increasingly complex, and multidisciplinary tumor meetings are assuming an increasingly vital role in the selection of effective methods. With the development of new treatment options, multidisciplinary tumour boards have become essential for selecting and customizing treatment methods, as well as addressing toxicity and survivability concerns.
5.3. Targeted Therapies or Immunotherapy
All the reported studies were published before targeted therapies or immunotherapy, so the role of these therapies inside a multidisciplinary meeting was not assessed.
5.4. Guideline Treatment
Decisions regarding treating and managing lung cancer patients can be made with the help of different evidence-based clinical practice guidelines, including ESMO and AIOM [17][25]. The few European studies reported in this chapter showed that despite their limitations, such as single institution, retrospective study design, small sample size, and potential referral bias, involving patient case discussion in a multidisciplinary setting is associated with increased utilisation of evidence-based treatment guidelines and greater adherence to guideline-based treatment.
5.5. Timeliness of Care
In their two retrospective studies [21][23], Price et al. and Forrest evaluated two categories of radiation therapy patients: curative and palliative. Different outcomes were observed in these trials following multidisciplinary care. Forrest et al. [21] examined inoperable NSCLC patients and found comparable rates of curative or palliative radiation therapy prior to and after the establishment of an MDM. The sample size of patients, particularly those receiving curative radiation therapy, was limited. Three years earlier, Price et al. [23] found a significant increase in the incidence of curative thoracic radiation therapy and a decrease in the rate of palliative thoracic radiation therapy among older patients. In the past decade, the recent advances in radiation therapy and the improved accuracy of radiation delivery have contributed to the observed improvements in patient survival, making radiation therapy, along with surgery, chemotherapy, immunotherapy, and targeted therapies, a cornerstone of modern lung cancer treatment. These advancements have contributed to the evolution of radiation therapy into a treatment recommended by guidelines for early-stage and locally progressed lung cancer, but not for small-cell lung cancer. Examples of this enhanced survival are the declining rates of non-treatment in early-stage lung cancer in population studies and the survival benefits observed in trials including immunotherapy after chemotherapy and radiation therapy in locally advanced NSCLC [27].
In addition, although radiation therapy has long been utilized for the palliation of advanced lung cancer, it increasingly has a function as a locally ablative therapy for patients with oligometastatic illness. As a result, treatment options are becoming increasingly complex, and multidisciplinary tumor conferences are playing an increasingly crucial role in determining the most effective techniques. With the availability of novel treatment options, multidisciplinary tumor boards have become essential for selecting and customizing treatment strategies, as well as controlling toxicity and survivability difficulties [28][29].
5.6. Palliative Care, Quality of Life, Patient Satisfaction
Smith et al. reported a qualitative assessment of 497 NSCLC patients visited in the palliative care clinic between January 2009 and January 2011. In a weekly MDM, respiratory physicians, thoracic oncologists, palliative care physicians, lung cancer nurses, and clinical trials discussed their patients’ cases. Patients in this study recognized various benefits of having palliative care services as part of multidisciplinary care, including increased service provision, quicker time for referrals and access to cancer trials, lower transport expenses, and a seamless transition between services [30]. They also observed that collaborative teamwork improves the palliative patient’s experience and is connected with possible cost savings for the organization.
References
- American Society of Clinical Oncology; European Society for Medical Oncology. ASCO-ESMO consensus statement on quality cancer care. Ann. Oncol. 2006, 17, 1063–1064.
- Gouveia, J.; Coleman, M.; Haward, R.; Zanetti, R.; Hakama, M.; Borras, J.M.; Primic-Žakelj, M.; de Koning, H.J.; Travado, L. Improving cancer control in the European Union: Conclusions from the Lisbon roundtable under the Portuguese EU presidency, 2007. Eur. J. Cancer 2008, 44, 1457–1462.
- Gaga, M.; Powell, C.A.; Schraufnagel, D.E.; Schönfeld, N.; Rabe, K.; Hill, N.S.; Sculier, J.-P. An official American Thoracic Society/European Respiratory Society statement: The role of the pulmonologist in diagnosing and managing lung cancer. Am. J. Respir. Crit. Care Med. 2013, 188, 503–507.
- Hardavella, G.; Frille, A.; Theochari, C.; Keramida, E.; Bellou, E.; Fotineas, A.; Bracka, I.; Pappa, L.; Zagana, V.; Palamiotou, M.; et al. Multidisciplinary care models for patients with lung cancer. Breathe 2020, 16, 200076.
- Haas, M.; Mortensen, M. The secrets of great teamwork. Harv. Bus. Rev. 2016, 94, 70–76.
- World Health Organization. Framework for Action on Interprofessional Education and Collaborative Practice; World Health Organization: Geneva, Switzerland, 2010. Available online: www.who.int/hrh/resources/framework_action/en/index.html (accessed on 26 April 2020).
- Royal College of Physicians. Respiratory Medicine: Workforce and Job Planning. Available online: www.rcpmedicalcare.org.uk/developingphysicians/specialties/respiratory-medicine/workforce (accessed on 20 April 2020).
- Denton, E.; Conron, M. Improving outcomes in lung cancer: The value of the multidisciplinary health care team. J. Multidiscip. Healthc. 2016, 9, 137–144.
- Ruhstaller, T.; Roe, H.; Thürlimann, B.; Nicoll, J.J. The multidisciplinary meeting: An indispensable aid to communication between different specialties. Eur. J. Cancer 2006, 42, 2459–2462.
- Mathioudakis, A.; Rousalova, I.; Gagnat, A.A.; Saad, N.; Hardavella, G. How to keep good clinical records. Breathe 2016, 12, 369–373.
- Jalil, R.; Lamb, B.; Russ, S.; Sevdalis, N.; Green, J.S.A. The cancer multidisciplinary team from the coordinators’ perspective: Results from a national survey in the UK. BMC Health Serv. Res. 2012, 12, 457.
- Nancarrow, S.; Booth, A.; Ariss, S.; Smith, T.; Enderby, P.; Roots, A. Ten principles of good interdisciplinary teamwork. Hum. Resour. Health 2013, 11, 19.
- Gamarra, F.; Noël, J.L.; Brunelli, A.; Dingemans, A.-M.C.; Felip, E.; Gaga, M.; Grigoriu, B.D.; Hardavella, G.; Huber, R.M.; Janes, S.; et al. Thoracic oncology HERMES: European curriculum recommendations for training in thoracic oncology. Breathe 2016, 12, 249–255.
- Hardavella, G.; Gaga, M. Harmonising Education in Thoracic Oncology in Europe; European Recommendations for integrated training. Pneumon 2016, 29, 203–205.
- Shaw, D.J.; Davidson, J.E.; Smilde, R.I.; Sondoozi, T.; Agan, D. Multidisciplinary team training to enhance family communication in the ICU. Crit. Care Med. 2014, 42, 265–271.
- Cancer Australia. All about Multidisciplinary Care. Available online: www.canceraustralia.gov.au/clinical-best-practice/multidisciplinary-care/all-about-multidisciplinary-care (accessed on 20 April 2020).
- European Society for Medical Oncology. ESMO Management and Treatment Adapted Recommendations in the COVID-19 Era: Lung Cancer. Available online: www.esmo.org/guidelines/cancer-patientmanagement-during-the-covid-19-pandemic/lung-cancerin-the-covid-19-era (accessed on 28 August 2020).
- Osarogiagbon, R.U.; Freeman, R.K.; Krasna, M.J. Implementing effective and sustainable multidisciplinary clinical thoracic oncology programs. Transl. Lung Cancer Res. 2015, 4, 448–455.
- National Lung Cancer Working Group. Lung Cancer Multidisciplinary Meeting Toolkit; Ministry of Health: Wellington, New Zealand, 2014.
- Patkar, V.; Acosta, D.; Davidson, T.; Jones, A.; Fox, J.; Keshtgar, M. Cancer multidisciplinary team meetings: Evidence, challenges, and the role of clinical decision support technology. Int. J. Breast Cancer 2011, 2011, 831605.
- Forrest, L.M.; McMillan, D.C.; McArdle, C.S.; Dunlop, D.J. An evaluation of the impact of a multidisciplinary team, in a single centre, on treatment and survival in patients with inoperable non-small-cell lung cancer. Br. J. Cancer 2005, 93, 977–978.
- Tamburini, N.; Maniscalco, P.; Mazzara, S.; Maietti, E.; Santini, A.; Calia, N.; Stefanelli, A.; Frassoldati, A.; Santi, I.; Rinaldi, R.; et al. Multidisciplinary management improves survival at 1 year after surgical treatment for non-small-cell lung cancer: A propensity score-matched study. Eur. J. Cardiothorac. Surg. 2018, 53, 1199–1204.
- Price, A.; Kerr, G.; Gregor, A. 237 Oral The impact of multidisciplinary teams and site specialisation on the use of radiotherapy in elderly people with non-small cell lung cancer (NSCLC). Radiother. Oncol. 2002, 64, S80.
- Murray, P.V.; O’Brien, M.E.; Sayer, R.; Cooke, N.; Knowles, G.; Miller, A.C.; Varney, V.; Rowell, N.P.; Padhani, A.R.; MacVicar, D.; et al. The pathway study: Results of a pilot feasibility study in patients suspected of having lung carcinoma investigated in a conventional chest clinic setting compared to a centralised two-stop pathway. Lung Cancer 2003, 42, 283–290.
- Passiglia, F.; Bertolaccini, L.; Del Re, M.; Facchinetti, F.; Ferrara, R.; Franchina, T.; Malapelle, U.; Menis, J.; Passaro, A.; Pilotto, S.; et al. Diagnosis and treatment of early and locally advanced non-small-cell lung cancer: The 2019 AIOM (Italian Association of Medical Oncology) clinical practice guidelines. Crit. Rev. Oncol. Hematol. 2020, 148, 102862.
- Davison, A.G.; Eraut, C.D.; Haque, A.S. Telemedicine for multidisciplinary lung cancer meetings. J. Telemed. Telecare 2004, 10, 140–143.
- Lin, P.; Koh, E.S.; Lin, M.; Vinod, S.K.; Ho-Shon, I.; Yap, J.; Som, S. Diagnostic and staging impact of radiotherapy planning FDG-PET-CT in non-small-cell lung cancer. Radiother. Oncol. 2011, 101, 284–290.
- Mohammed, N.; Kestin, L.L.; Grills, I.S.; Battu, M.; Fitch, D.L.; Wong, C.-Y.O.; Margolis, J.H.; Chmielewski, G.W.; Welsh, R.J. Rapid disease progression with delay in treatment of non-small-cell lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2011, 79, 466–472.
- Osarogiagbon, R.U. Making the evidentiary case for universal multidisciplinary thoracic oncologic care. Clin. Lung Cancer 2018, 19, 294–300.
- Smith, J.; Williamson, I.; Ionescu, A.; Brewster, A.E.; Howison, H.; Williams, S.; Smith, C.; Noble, S.I.R. 97 Improving outcomes for palliative lung cancer patients: Experience of a multiprofessional parallel clinic model in a district general hospital. Lung Cancer 2012, 75, S32.
More
Information
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.4K
Revisions:
2 times
(View History)
Update Date:
02 Aug 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




