Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Elena González-Burgos | -- | 4288 | 2022-07-27 09:00:10 | | | |
| 2 | Peter Tang | Meta information modification | 4288 | 2022-07-27 09:52:16 | | | | |
| 3 | Peter Tang | -8 word(s) | 4280 | 2022-07-27 09:55:53 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Sánchez, M.; González-Burgos, E.; Iglesias, I.; Gómez-Serranillos, M.P. Pharmacological Update Properties of Aloe Vera Active Constituents. Encyclopedia. Available online: https://encyclopedia.pub/entry/25567 (accessed on 07 March 2026).
Sánchez M, González-Burgos E, Iglesias I, Gómez-Serranillos MP. Pharmacological Update Properties of Aloe Vera Active Constituents. Encyclopedia. Available at: https://encyclopedia.pub/entry/25567. Accessed March 07, 2026.
Sánchez, Marta, Elena González-Burgos, Irene Iglesias, M. Pilar Gómez-Serranillos. "Pharmacological Update Properties of Aloe Vera Active Constituents" Encyclopedia, https://encyclopedia.pub/entry/25567 (accessed March 07, 2026).
Sánchez, M., González-Burgos, E., Iglesias, I., & Gómez-Serranillos, M.P. (2022, July 27). Pharmacological Update Properties of Aloe Vera Active Constituents. In Encyclopedia. https://encyclopedia.pub/entry/25567
Sánchez, Marta, et al. "Pharmacological Update Properties of Aloe Vera Active Constituents." Encyclopedia. Web. 27 July, 2022.
Copy Citation
Aloe vera (Aloe barbadensis Miller, family Xanthorrhoeaceae) is a perennial green herb with bright yellow tubular flowers that is extensively distributed in hot and dry areas of North Africa, the Middle East of Asia, the Southern Mediterranean, and the Canary Islands. Aloe vera has been traditionally used to treat skin injuries (burns, cuts, insect bites, and eczemas) and digestive problems because its anti-inflammatory, antimicrobial, and wound healing properties.
Aloe vera
pharmacology
extracts
isolated compounds
1. Introduction
Aloe vera (Aloe barbadensis Miller, family Xanthorrhoeaceae) is a perennial green herb with bright yellow tubular flowers that is extensively distributed in hot and dry areas of North Africa, the Middle East of Asia, the Southern Mediterranean, and the Canary Islands. Aloe vera derives from “Allaeh” (Arabic word that means “shining bitter substances”) and “Vera” (Latin word that means “true”). The colorless mucilaginous gel from Aloe vera leaves has been extensively used with pharmacological and cosmetic applications. Traditionally, this medicinal plant has been employed to treat skin problems (burns, wounds, and anti-inflammatory processes). Moreover, Aloe vera has shown other therapeutic properties including anticancer, antioxidant, antidiabetic, and antihyperlipidemic. Aloe vera contains more than 75 different compounds, including vitamins (vitamin A, C, E, and B12), enzymes (i.e., amylase, catalase, and peroxidase), minerals (i.e., zinc, copper, selenium, and calcium), sugars (monosaccharides such as mannose-6-phosphate and polysaccharides such as glucomannans), anthraquinones (aloin and emodin), fatty acids (i.e., lupeol and campesterol), hormones (auxins and gibberellins), and others (i.e., salicylic acid, lignin, and saponins) [1][2][3] (Figure 1, Figure 2).
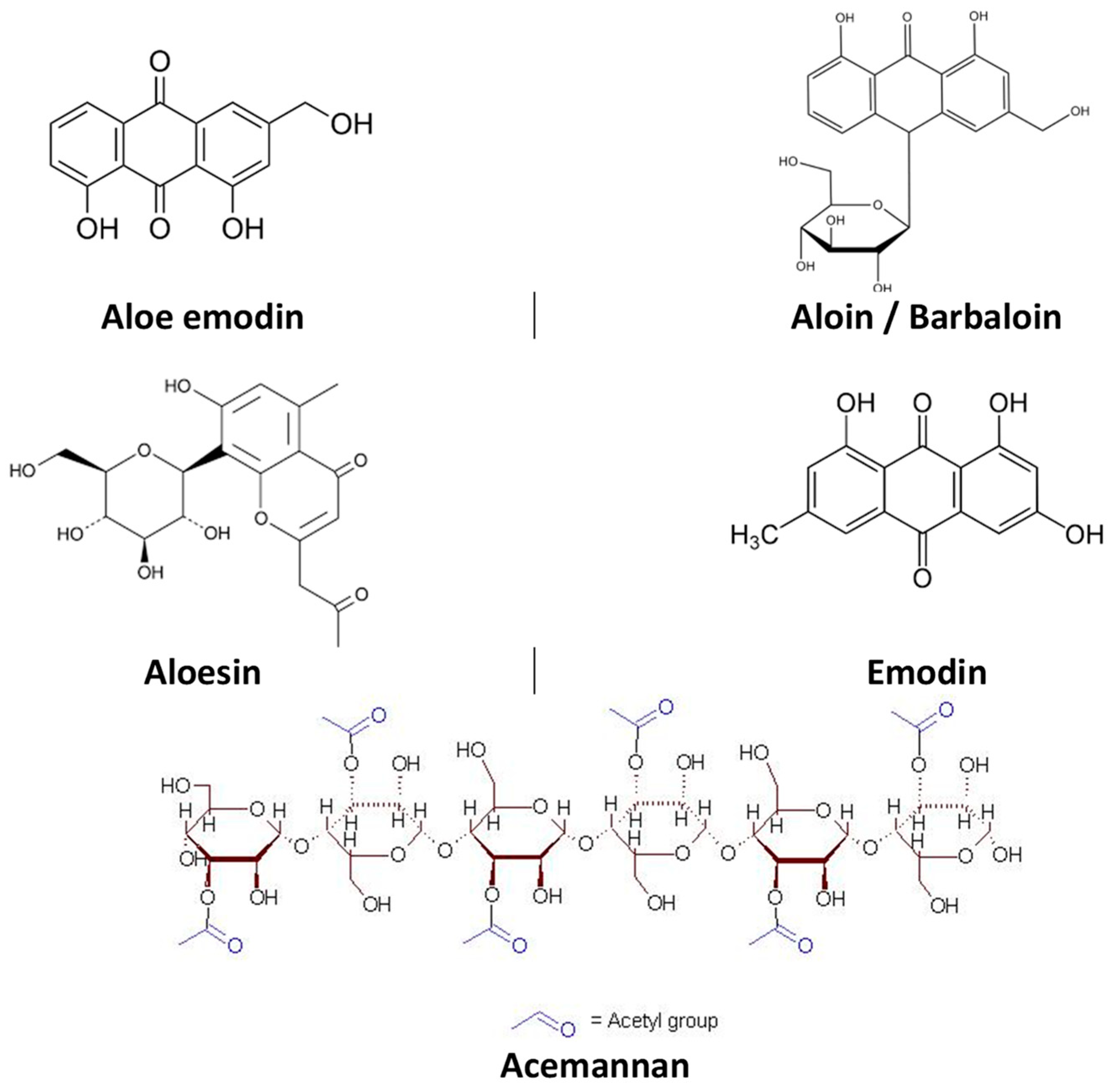
Figure 1. Chemical structure of compounds isolated from Aloe vera with pharmacological activity.
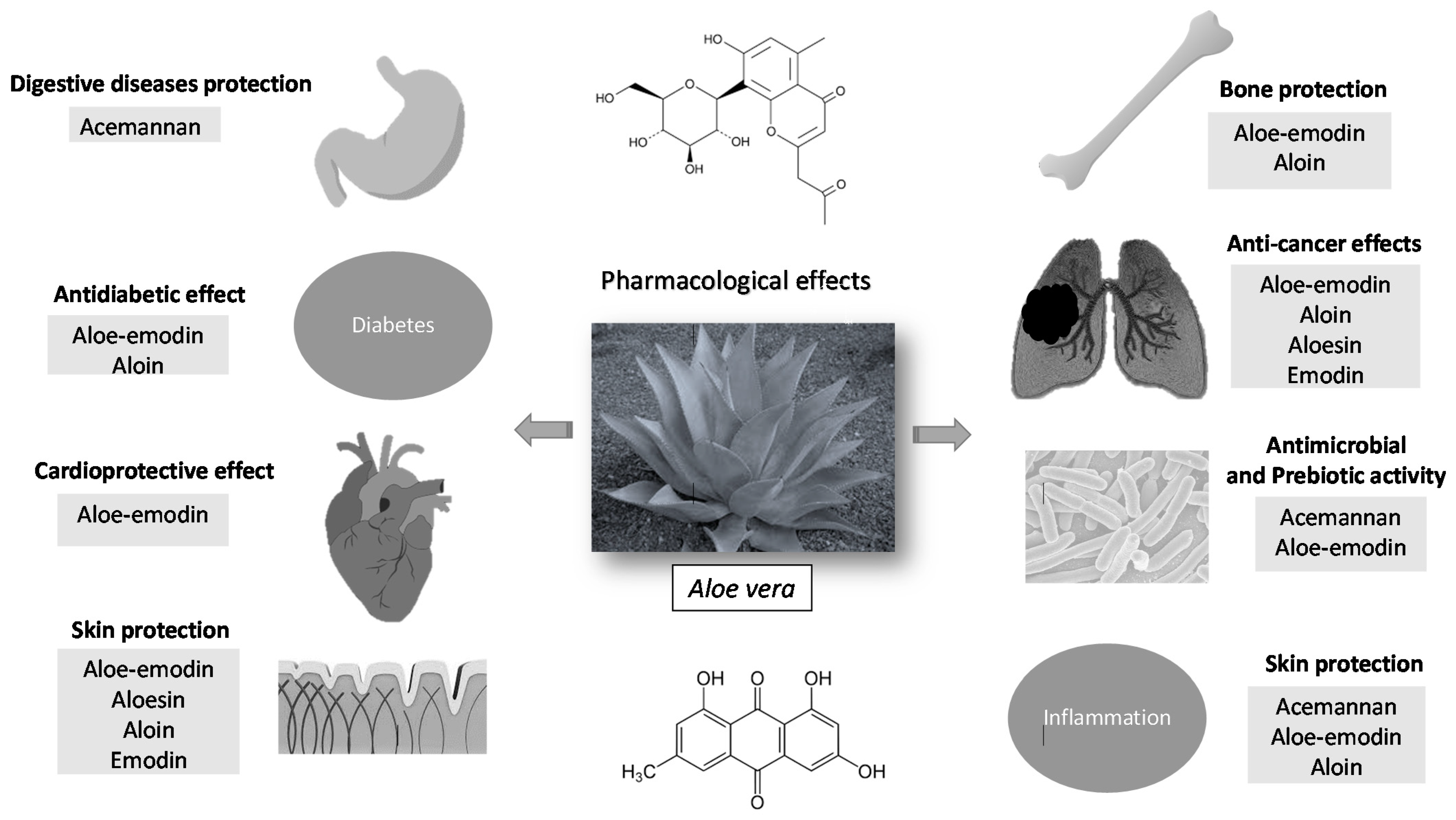
Figure 2. Pharmacological effects of the main constituents of Aloe vera.
2. Digestive Diseases Protection
Aloe vera extract (50%) increased cell viability of dental pulp stem cells being useful for avulsed broken teeth [4]. This effect is attributed to polysaccharides, mainly acemannan, by inducing osteogenic-specific gene expressions, DNA synthesis, growth factor, and JAK-STAT pathway [5][6]. Moreover, Aloe vera (225 mg/kg) exerted a radioprotective effect against salivary gland dysfunction in a rat model as evidenced in an increase of salivary flow rate [7].
Periodontitis is a serious and common dental affliction in which gums are infected and become inflamed, causing tissue and bone destruction. Gingivitis is the initial phase of periodontitis and is caused by dental plaque. Significant clinical evidence has demonstrated that Aloe vera mouthwash and gel are effective in the prevention and treatment of gingivitis and periodontitis by reducing gingival index, plaque index, and probing depth and by increasing bone fill and regeneration [8][9][10][11][12][13][14]. Aloe vera has proven to be as effective as other usual treatments such as chlorhexidine, alendronate, and chlorine dioxide [8][10][11][13].
In a randomized placebo double-blind study with 20 healthy adults, Fallahi et al. [15] investigated the effect of Aloe vera mouthwash on postoperative complications after impacted third molar surgery. Aloe vera gel significantly reduced swelling and postoperative pain. In another work, Kalra et al. [16] evaluated the efficacy of Aloe vera gel and mineral trioxide aggregate as pulpotomy agents in primary molar teeth. The overall success rates at 3, 6, 9, and 12 months was high for patients treated with mineral trioxide aggregate. Moreover, a cross-sectional randomized interventional study revealed that Aloe vera gel promoted wound healing and reduced pain in patients that required atraumatic tooth extractions, and its effectiveness was higher than that of traditional analgesics [17]. Furthermore, Aloe vera resulted to be a promising cavity disinfecting agent in minimally invasive dentistry in a randomized clinical trial with 10 patients [18].
Oral mucositis/stomatitis is an inflammatory and/or ulcerative condition that occurs as a debilitating complication of chemotherapy and radiotherapy treatments and affects quality of life of oncological patients. Aloe vera mouthwash alleviated radiation-induced mucositis severity in patients with head and neck cancers similarly to the reference benzydamine mouthwash [19]. Moreover, Aloe vera mouthwash has also demonstrated to be efficient in the treatment of stomatitis (mean intensity and pain) associated with radiotherapy in patients with acute myeloid leukemia and acute lymphocytic leukemia [20].
Oral submucous fibrosis is a precancerous condition of the oral cavity characterized by abnormal collagen deposition. This malignant disorder is mainly caused by chewing areca nut and it is most frequent in India and Southeast Asia. Anuradha et al. [21] evaluated the efficacy of Aloe vera (systemic as juice and topical as gel) in the treatment of oral submucous fibrosis. Clinical evidence demonstrated that Aloe vera reduced burning sensation and increased cheek flexibility, mouth opening, and tongue protrusion similar to the reference treatment hydrocortisone, hyaluronidase, and antioxidant supplements. In another study on oral submucous fibrosis, the combination of Aloe vera gel with physiotherapy was more efficient in decreasing burning sensation and increasing tongue protrusion, mouth opening, and cheek flexibility than the combination of antioxidant capsules with physiotherapy [22].
Gastroesophageal reflux disease is a common chronic digestive disease in which gastric acids move up into the esophagus. Aloe vera syrup (10 mL/day) for 4 weeks reduced the frequency of symptoms of gastroesophageal reflux diseases including heartburn, food regurgitation, dysphagia, flatulence, belching, nausea, and acid regurgitation without causing adverse effects (only one case of vertigo and another of stomach ache were reported) [23].
Gastritis is an inflammation of mucous membrane layer of the stomach. Aloe vera gel protected in a Balb/c mouse model of alcohol-induced acute gastritis by increasing matrix metalloproteinase-9 inhibitory activity [24].
The topical administration of Aloe vera 3% ointment alleviated the symptoms of diarrhea and fecal urgency in patients with acute radiation proctitis induced by radiotherapy of the pelvic area [25]. Moreover, Aloe barbadensis extract (AVH200®) reduced, but not significantly, the severity of gastrointestinal symptoms in patients with irritable bowel syndrome compared to a control group [26]. Lin et al. [5] revealed that Aloe polysaccharide (15 mg/kg) protected rats from 2,4,6-three nitrobenzene sulfonic acid colitis induced by increasing JAK2, p-JAK2, STAT-3, and p-STAT3 protein expression. Furthermore, Aloe vera cream applied three times daily for 6 weeks reduced chronic anal fissure pain and hemorrhaging after defection and promoted wound healing in a prospective double blind clinical trial [27].
3. Skin Protection
Most in vitro studies on skin protection study the ability of Aloe vera and active compounds in wound healing. The immortalized human keratinocyte HaCaT cell line, the primary normal human epidermal keratinocytes HEKa cell line, and fibroblasts cell lines are the most used. These studies have revealed that Aloe vera and its major compounds (aloesin, aloin, and emodin) exert their protective action mainly through antioxidant and anti-inflammatory mechanisms. Hence, Aloe vera up-regulated TFGβ1, bFGF, and Vegf-A expression in fibroblasts and increased keratinocyte proliferation and differentiation by lysosomal membrane stability [28][29][30][31][32]. Moreover, Aloe vera solution could accelerate corneal wound closure at low concentrations (≤175 μg/mL) by increasing type IV collagen-degrading activity in a cellular model of primary cultures of corneal epithelial cells [33]. Furthermore, aloin exerted skin protection by reducing IL-8 production, DNA damage, lipid peroxidation, and ROS generation and by increasing GSH content and SOD activity [34]. The compound aloesin resulted in promoting wound healing by increasing cell migration via phosphorylation of Cdc42 and Rak1, cytokines, and growth factors [35]. In addition to this healing activity, it has been seen that Aloe polysaccharide (20, 40, and 80 µg/mL for 24 h) could be a beneficial agent in psoriasis as evidenced in the inhibition of TNF-α levels and IL-8 and IL-12 protein expression in human keratinocyte HaCaT cell line.
As for in vivo studies, the most common models are genetically modified animals (BALB/c mice, HR-1 hairless mice and SKH-1 hairless mice) and UV and X-ray skin damage in animals. Most of these in vivo studies have been done with Aloe vera extracts and gel. Application of topical Aloe vera favored wound healing in animal models with dermal incisions by reducing inflammatory cell infiltration, increasing CD4+/CD8+ ratio lymphocytes, and improving epidermal thickness and collagen deposition [36][37][38][39]. In another study conducted in Indonesia with several medicinal plants, the effect of Nigella sativa oil gel and Aloe vera gel to treat diabetic ulcers was investigated. Aloe vera resulted to be more efficient in improving wound healing on alloxan-induced diabetes in Wistar rats with wounds on dorsum as evidenced by a decrease of necrotic tissue and inflammation and an improvement of re-epithelialization [40]. Furthermore, a UV-induced mice model revealed that Aloe vera gel powder increased epidermal growth factor and hyaluronan synthase and reduced matrix metalloproteinases expression (types 2, 9, and 13) [41][42]. Aloe sterols are involved in this UV protection [43]. Likewise, it has been observed that Aloe vera protected against X-radiation through antioxidant mechanisms (increased antioxidant enzyme activity and GSH content and reduced ROS production and lipid peroxidation) [44][45]. Among isolated compounds, investigations with the compounds aloe-emodin and aloesin have shown that their healing activity is due to angiogenic properties [46][47].
In the last 6 years, several clinical trials have also been carried out. Some of these have been aimed at evaluating the effectiveness of Aloe vera on ulcers. Hence, the administration of Aloe vera gel twice daily for 3 months improved and accelerated wound healing as well as reduced hospitalization time [48][49]. Moreover, in a randomized, triple-blind clinical trial with 80 patients hospitalized in the orthopedic ward, Hekmatpou et al. [50] demonstrated that Aloe vera gel twice daily for 10 days prevented the development of pressure ulcers on the areas of hip, sacrum, and heel. Moreover, clinical trials have demonstrated that Aloe vera facilitated rapid tissue epithelialization and granulation in burns [51], promoted healing of cesarean wound [52], and accelerated wound healing of split-thickness skin graft donor sites [53]. Furthermore, Aloe vera has been investigated in randomized, double-blind, placebo-controlled studies for its benefits to maintain healthy skin. Therefore, the daily oral intake of 40 µg of Aloe sterol (cycloartenol and lophenol) for at least 12 weeks improved skin elasticity in men under 46 years exposed to the sunlight but do not use sunscreen to protect themselves [54], reduced facial wrinkles in Japanese women over 40 years old by stimulating hyaluronic acid and collagen production [55], and increased gross elasticity, net elasticity, and biological elasticity in women aged 30–59 [56]. However, despite clinical evidence on the protective role of Aloe vera in the skin, there are clinical trials that have not yet found effectiveness of this medicinal plant, particularly in decreasing radiation-induced skin injury. Two clinical trials have been published between 2014 and 2019 in relation to this effect. Both studies found that topical administration of Aloe vera as gel or cream did not reduce the prevalence and severity of radiotherapy-induced dermatitis and skin toxicity in breast cancer patients compared to control group [57][58].
4. Anti-Inflammatory Activity
Most recent studies on anti-inflammatory activity of Aloe vera are focused on the action mechanism of isolated compounds in murine macrophage RAW264.7 cells and mice stimulated with LPS. Hence, the potential anti-inflammatory effect of aloin is related to its ability to inhibit cytokines, ROS production, and JAK1-STAT1/3 signaling pathway [59][60]. Moreover, aloe-emodin sulfates/glucuronides (0.5 μM), rhein sulfates/glucuronides (1.0 μM), aloe-emodin (0.1 μM), and rhein (0.3 μM) inhibited pro-inflammatory cytokines and nitric oxide production, iNOS expression, and MAPKs phosphorylation [61].
In another study, Thunyakitpisal et al. [62] demonstrated that acemannan increased IL-6 and IL-8 expression and NF-κB/DNA binding in human gingival fibroblast via a toll-like receptor signaling pathway. Since there is a relation between high IL-1β levels and periodontal diseases, Na et al. [63] investigated the anti-inflammatory properties of aloin in human oral KB epithelial cells stimulated with saliva from healthy volunteers. This study revealed that those saliva samples with high content in IL-1β stimulated IL-8 production in KB cells, and pretreatments with aloin inhibited IL-8 production by decreasing p38 and extracellular signal-regulated kinases pathway.
In addition to isolated compounds, Ahluwalia et al. [64] evaluated the activity of AVH200®, a standardized Aloe vera extract which contains alin and acemannan on the activation, proliferation, and cytokine secretion of human blood T cells obtained from healthy individuals aged 18–60, and they found that it decreased CD25 and CD3 expression on CD3(+) T cells. Moreover, AVH200® exhibited concentration-dependent T cell proliferation suppression and IL-2, IFN-γ, and IL-17A reduction. Moreover, the anti-inflammatory effect of Aloe vera has also been investigated in an acetaminophen-induced hepatitis (inflammatory condition of the liver) mice model. The results of this study revealed that Aloe vera (150 mg/kg) reduced hepatic MDA, IL-12, and IL-18 levels and ALT and increased GSH content [65].
5. Anticancer Effects
Studies conducted in the years of the research focusing on cancer are mostly in vitro and in vivo studies. In vitro studies have the main purpose of identifying potential molecules with cytotoxic activity for later evaluation in in vivo studies and clinical trials. In addition, in vitro studies allow elucidating the mechanism of action by identifying promising pharmacological targets. In vivo studies allow us to understand the pharmacological activity and behavior in living organisms prior to their study in humans. Since clinical trials are very limited, and as it is not possible to confirm the anti-cancer activity of Aloe vera and its bioactive principles, it would be interesting for future research to focus on this activity based on the promising in vitro and in vivo results.
In vitro and in vivo studies included here are aimed at evaluating cytotoxic and antitumor activity against a variety of cancer types using a diversity of cell lines and animal models (breast and gynecological cancers such as cervical cancer and ovarian cancer, malignant conditions of the gastrointestinal tract (i.e., oral cavity, esophagus, colon) and accessory digestive organs (pancreas), osteosarcomas, and melanoma). One clinical trial focused on the efficacy of Aloe vera on ocular surface squamous neoplasia; this clinical trial has been included at the end of this section.
MCF-7 cells, which express estrogen receptor, are the most popular breast cancer cell line, and the immortal HeLa cell line are the oldest and most used cervical cancer cells [66][67]. Aloe vera crude extracts (40%, 50%, and 60% for 6, 24, and 48 h) reduced cell viability of cancer cell lines (human breast MCF-7 and cervical HeLa) through apoptosis induction (chromatin condensation and fragmentation and apoptotic bodies appearance in sub-G0/G1 phases) and modulation of effector genes expression (an increase in cyclin D1, CYP1A1, and CYP1A2 expression and a decrease in p21 and bax expression) [68]. Moreover, the isolated compound aloe-emodin has resulted to be an effective anticancer agent against both MCF-7 cells and HeLa cells by inducing mitochondrial and endoplasmic reticulum apoptosis and inhibiting metastasis oxidative stress [69][70][71][72]. Furthermore, a recent study demonstrated that Aloe vera extract (300 mg/kg) and training (swimming) combined exerted a protective anticancer effect in mice with breast cancer by inhibiting the COX pathway (COX-2 reduction levels) and prostaglandin E2 production [73]. Finally, aloesin reduced tumor growth in in vitro and in vivo models of ovarian cancers by inhibiting the MAPK signaling pathway [74].
For malignant conditions of gastrointestinal tract and accessory digestive organs, emodin (10, 20, 30, 40 μM for 24 and 48 h) decreased cell proliferation and Bcl-2 protein levels and increased caspase-3 protein expression and Bax protein levels in human oral mucosa carcinoma KB cells [75]. Moreover, aloe-emodin has been shown to effectively suppress esophageal TE1 cancer cells in a concentration-dependent manner (from 2.5 µM to 20 µM concentrations assayed) through inhibiting AKT and ERK phosphorylation and reducing the number of cells in the S phase [76]. Furthermore, Aloe polysaccharide induced autophagy alone and in combination with radiation in pancreatic carcinoma BxPC-3 cells as evidenced in ULK1 mRNA expression upregulation and BECN1 and BCL-2 mRNA expression downregulation [77]. Finally, several in vitro and in vivo studies were performed to evaluate the potential anticancer properties of Aloe vera and its isolated compounds in colon cancer (fourth most common cancer and the third leading death cause) [78]. Chen et al. [79] exhibited cytotoxic properties of aloe-emodin on colon cancer cells at 10, 20, and 40 μM concentrations through activating the apoptotic pathway, increasing ROS production, and cytosolic calcium levels and up-regulating ER stress-related proteins. Moreover, Aloe vera powder and extract 1% and 3% protected C57BL/6J mice from aberrant crypt foci colorectal cancer by increasing hepatic phase II enzyme glutathione S-transferase mRNA levels [80]. Furthermore, Aloe vera gel (200 or 400 mg/kg/day orally) reduced inducible NO synthase and COX2 expression, NF-kB activation, and cell cycle progression, inducing cellular factors in BALB/c female mice with induced colitis-associated colon carcinogenesis.
Osteosarcomas are uncommon bone tumors in which malignant cells produce osteoid [81]. Aloe-emodin has also resulted to be a promising photosensitive agent against the human osteosarcoma MG-63 cell line via ROS/JNK signaling pathway as evidenced in an increase of caspases, cytochrome c, CHOP, and GRP78 expression [82][83].
For melanoma (malignant transformation of melanocytes), aloe-emodin protected against metastatic human melanoma cells by decreasing cell proliferation, increasing cell differentiation, and transamidating activity of transglutaminase and dabrafenib antiproliferative activity [84][85].
Regarding clinical trials conducted in recent years on anticancer activity, Damani et al. [86] reported the efficacy of Aloe vera eye drops 3 times daily for 3 months in the regression of ocular surface squamous neoplasia in a 64-year-old Hispanic woman. On the other hand, Koo et al. [87] stated that aloe polysaccharide could reduce tobacco associated diseases such as cancer due to its ability to increase urinary excretion of benzo(a)pyrene and cotinine.
6. Antidiabetic Effect
Diabetes is a chronic disease presenting with high levels of glucose in blood because of an insulin resistance or an insulin deficiency. Studies on the effect of Aloe vera in diabetes and related complications have been investigated mainly in animal models induced by streptozotocin. Consistent evidence supports that oxidative stress is a main cause of the beginning and the progression of diabetes complications such as nephropathies and neuropathies. Hence, using this experimental model, Aloe vera showed to reduce blood glucose levels, to increase insulin levels, and to improve pancreatic islets (number, volume, area, and diameter) [88], and this medicinal plant protected from oxidative stress-induced diabetic nephropathy and anxiety/depression-like behaviors [89]. Moreover, Aloe vera topical administration (60 mg/mL, four times daily for 3 days of eye drops) favored corneal re-epithelialization in streptozotocin-induced diabetic Wistar rats with corneal alkali burn injury [90]. Furthermore, experiments with genetically modified animals have revealed that Aloe vera polysaccharides (100 µg/g for 3 weeks) are responsible for the decrease of blood glucose levels [91]. A recent in vitro study showed that the action mechanism of Aloe vera polysaccharides antidiabetic effect is related to its ability to inhibit apoptosis and endoplasmic reticulum stress signaling [91]. In another in vitro study using a high-glucose-induced toxicity cell model, the compound aloe-emodin (20 μM) protected RIN-5F cells derived from rat pancreatic β-cells from glucotoxicity through an apoptotic and anti-inflammatory effects [92]. Lastly, the intake of Aloe vera (300 mg twice day for 4 weeks) decreased fasting blood glucose in pre-diabetic subjects [93].
7. Antioxidant Properties
Antioxidants are compounds that prevent or slow down biomolecule oxidative damage caused by ROS through free radical scavenging, metal chelation, and enzyme regulation [94]. Kumar et al. 2017 [95] investigated the potential antioxidant activity of crude methanolic extracts of Aloe vera from six agro-climatic zones of India using different in vitro methods (i.e., DPPH, metal chelating, and reducing power assay). Antioxidant activity was higher in those species collected in Northern India than in Southern India, which is related to a high content in alkaloids, glycosides, phenolic compounds, flavonoids, and saponin glycosides. Moreover, Aloe vera ethanol extract protected, particularly human microvascular endothelial cells, against hydrogen peroxide and 4-hydroxynonenal-induced toxicity by reducing ROS production and HNE-protein adducts formation [96]. The antioxidant activity of Aloe vera is, at least in part, due to anthraquinones and related compounds (10 µM) which possess peroxyl radical scavenging activity and reducing capacity [97].
Apart from these in vitro assays, in a clinical trial with 53 healthy volunteers, the intake of Aloe vera gel extract (14 days) increased total antioxidant capacity of plasma of subjects [98].
8. Bone Protection
In vitro studies with isolated Aloe vera compounds have been aimed at studying the potential protective effect on bone pathogenesis. Aloe-emodin induced chondrogenic differentiation on clonal mouse chondrogenic ATDC5 cells which is related to bone formation through BMP-2 and MAPK-signaling pathway activation [99]. Moreover, aloin has resulted to be beneficial in osteoporosis and osteopenia disorders by suppressing receptor activator of NFĸB ligand (RankL) induced through NF-κB inhibition in mouse macrophage RAW 264.7 cells [100][101].
9. Cardioprotective Effect
In vivo models of ischemia-reperfusion injury are commonly employed to evaluate the cardioprotective activity of Aloe vera. Aloe vera administered with gastric gavage previous to abdominal aorta and spinal cord ischemia increased antioxidant enzymes activity (SOD, CAT, and GPx) and reduced lipid peroxidation level (MDA content), edema, hemorrhage, and inflammatory cell migration in Wistar albino rats [102][103]. Moreover, barbaloin, also known as aloin, (20 mg/kg/day, 5 days) administered intragastrically reduced myocardial oxidative stress and inflammatory response and increased AMPK signaling in Sprague-Dawley rats in a myocardial ischemia/reperfusion injury [104]. Esmat et al. [105] demonstrated that this compound (50 mg/kg body weight, twice weekly over 2 weeks), administered intramuscularly, had non-atherogenic activity and iron chelating properties. Another compound isolated from Aloe vera and investigated for its cardioprotective properties is aloe-emodin. In an in vitro model of heme protein (hemoglobin), it was demonstrated that aloe-emodin (100 μM) had its maximum activity as an anti-aggregatory agent as evidenced in structural alterations of β sheet and the appearance of α helices [106]. On the other hand, an in vivo study revealed that aloe-emodin could alleviate hyperlipidemia by reducing total cholesterol and low-density lipoprotein-cholesterol levels at doses of 50 and 100 mg/kg for 6 weeks in male Wistar rats [107]. Regarding clinical studies, a double-blind randomized controlled trial showed that Aloe vera 300 mg and 500 mg/twice day for 4 and 8 weeks reduced HbA1C, total cholesterol, LDL, and triglyceride levels in pre-diabetic patients [92]. Furthermore, the oral gavage administration of Aloe vera (30 mg/kg/day for 1 month) resulted to decrease ischemic fiber degeneration by preventing the formation of lipid peroxides, increasing antioxidant enzymes, and up-regulating the transcription factor NRF1 in Wistar albino rats [108].
10. Antimicrobial and Prebiotic Activity
Different studies have been carried out to evaluate the antimicrobial activity of Aloe vera and its main constituents. Most of these studies are in vitro and focus on the antibacterial activity. One of the most studied bacteria are Staphlococcus aureus and Pseudomonas aeruginosa. Hence, Aloe vera aqueous extract reduced growth and biofilm formation against methicillin resistant Staphylococcus aureus [109]. Moreover, this bacteria has also been inhibited by Aloe vera gel (50% and 100% concentrations), along with other oral pathogens obtained from patients with periapical and periodontal abscess including Actinobacillus actinomycetemcomitans, Clostridium bacilli, and Streptococcus mutans using disc diffusion, micro-dilution, and agar dilution methods [110]. One of the compounds attributed to antibacterial activity against Staphylococcus aureus is aloe-emodin which acts by inhibiting biofilm development and extracellular protein production [111]. In the case of Pseudomonas aeruginosa, Aloe vera extracts have shown to inhibit the growth of multidrug-resistant Pseudomonas aeruginosa isolated from burned patients with wounds infections at MIC50 and MIC90 values of 200 µg/mL [112]. Pseudomonas aeruginosa growth and biofilm formation inhibition has been also demonstrated for Aloe vera inner gel. This Aloe vera inner gel also inhibited other Gram-negative bacteria (Helicobacter pylori and Escherichia coli) as well as the fungus Candida albicans [113]. Moreover, in another study, Aloe vera hydroalcoholic extract showed antibacterial activity against Enterococcus faecalis, an infecting microorganism of the root canals of teeth, with inhibition zones of 13 mm (saturated) and 9.6 mm (diluted) [114]. Furthermore, concentrations up to 1 mg/mL of Aloe vera aqueous extracts could inhibit Mycobacterium tuberculosis growth, which is the pathogen responsible for causing tuberculosis, one of the most lethal infectious diseases worldwide [115]. Finally, in a clinical trial with 53 healthy volunteers, the daily drinking of Aloe vera gel extract for 14 days exerted an antimicrobial activity as shown in a reduction of Lactobacillus spp. number [98].
Antiviral activity of Aloe vera has been investigated for herpes simplex virus type 1 and H1N1 subtype influenza virus. Aloe vera extract gel (concentrations from 0.2% to 5%) showed antiviral activity against herpes simplex virus type 1 on Vero cells by inhibiting its growth [116]. On the other hand, in vitro studies have demonstrated that Aloe polysaccharides decreased H1N1 subtype influenza virus replication and viral adsorption period by interacting with influenza virus particles. Moreover, in vivo studies with SPF BALB/c mice infected with PR8(H1N1) improved clinical symptoms and lung damage [117].
Finally, there are other studies which support the prebiotic potential of Aloe vera defined as “a substrate that is selectively utilized by host microorganisms conferring a health benefit”. Aloe vera mucilage (rich in acemannan) could improve gastrointestinal health by increasing short chain fatty acids and modifying bacterial composition [118]. Moreover, acemannan and fructans from Aloe vera increased bacterial growth, especially Bifidobacterium spp. population [119].
11. Other Effects
Aloe vera has also been investigated for treating reproductive health care problems. The results of these works carried out with experimental animals are contradictory. While Asgharzade et al. [120] demonstrated that Aloe vera ethanol extract (150 and 300 mg/kg) had negative effects on spermatogenesis and sperm quality in Wistar rats, Erhabor and Idu [121] observed that Aloe vera ethanol extract (400 mg/kg) improved male sexual behavior (mount frequency and latency, intromission frequency and latency, and testosterone levels) and Behmanesh et al. [122] that Aloe vera extract increased body and testis weights, spermatocyte and spermatids quantity, and seminiferous tubule diameter and height.
Aloe vera processed gel prevented of ovoalbumin-induced food allergy by exerting an anti-inflammatory action (histamine, mast cell protease-1, and IgE reduction) [123].
At the blood level, the oral administration of Aloe vera gel prevented and restored lymphopenia and erythropenia as well as IgA secretion on cyclophosphamide-induced genetically modified mice [124]. Moreover, Aloe vera ethanol extract (200 mg/kg, 400 mg/kg, and 600 mg/kg) normalized levels of white blood cells, red blood cells, and platelet count through antioxidant mechanisms [125].
Regarding diseases of the musculoskeletal system, aloe-emodin showed to reduce viable cell numbers (concentrations ≥10 µM) and to induce apoptosis by arresting G2/M phase (concentrations ≥20 µM) in MH7A human synovial fibroblast-like cells, aloe-emodin being a promising agent to treat rheumatoid arthritis and a complementary treatment to methotrexate [126]. Moreover, Aloe vera lyophilized extract ointment reduced tendon lesions and increased non-collagenous proteins in Wistar rats with partial transection of the calcaneal tendon [127].
The dose of 10 mg/kg of Aloe vera aqueous extract (3 times daily for a week) resulted to be the most effective in morphine withdrawal syndrome in morphine-dependent female rats as shown in agitation, disparity, and floppy eyelids reduction [128].
Finally, highlighting the protective effect of Aloe vera gel extract (seven weeks, 500 mg/kg b.w. daily) on pulmonary tissue of cigarette smoke induced in Balb/c mice by reducing mucin production, citrulline and NO levels, and peroxidative damage [129].
References
- Surjushe, A.; Vasani, R.; Saple, D.G. Aloe vera: A short review. Indian J. Dermatol. 2008, 53, 163–166.
- Malik, I.; Zarnigar, H.N. Aloe vera-A Review of its Clinical Effectiveness. Int. Res. J. Phar. 2003, 4, 75–79.
- Maan, A.A.; Nazir, A.; Khan, M.K.I.; Ahmad, T.; Zia, R.; Murid, M.; Abrar, M. The therapeutic properties and applications of Aloe vera: A review. J. Herb. Med. 2018, 12, 1–10.
- Sholehvar, F.; Mehrabani, D.; Yaghmaei, P.; Vahdati, A. The effect of Aloe vera gel on viability of dental pulp stem cells. Dent. Traumatol. 2016, 32, 390–396.
- Lin, H.; Honglang, L.; Weifeng, L.; Junmin, C.; Jiantao, Y.; Junjing, G. The mechanism of alopolysaccharide protecting ulceralive colitis. Bio. Pharm. 2017, 88, 145–150.
- Songsiripradubboon, S.; Kladkaew, S.; Trairatvorakul, C.; Sangvanich, P.; Soontornvipart, K.; Banlunara, W.; Thunyakitpisal, P. Stimulation of dentin regeneration by using acemannan in teeth with lipopolysaccharide-induced pulp inflammation. J. Endod. 2017, 43, 1097–1103.
- Nejaim, Y.; Silva, A.I.; Vasconcelos, T.V.; Silva, E.J.; de Almeida, S.M. Evaluation of radioprotective effect of Aloe vera and zinc/copper compounds against salivary dysfunction in irradiated rats. J. Oral Sci. 2014, 56, 191–194.
- Kumar, G.R.; Devanand, G.; John, B.D.; Ankit, Y.; Khursheed, O.; Sumit, M. Preliminary antiplaque efficacy of Aloe vera mouthwash on 4 day plaque re-growth model: Randomized control trial. Ethiop. J. Health Sci. 2014, 24, 139–144.
- Pradeep, A.R.; Garg, V.; Raju, A.; Singh, P. Adjunctive local delivery of Aloe vera gel in patients with type 2 diabetes and chronic periodontitis: A randomized, controlled clinical trial. J. Periodontol. 2016, 87, 268–274.
- Vangipuram, S.; Jha, A.; Bhashyam, M. Comparative efficacy of Aloe vera mouthwash and chlorhexidine on periodontal health: A randomized controlled trial. J. Clin. Exp. Dent. 2016, 8, e442.
- Yeturu, S.K.; Acharya, S.; Urala, A.S.; Pentapati, K.C. Effect of Aloe vera, chlorine dioxide, and chlorhexidine mouth rinses on plaque and gingivitis: A randomized controlled trial. J. Oral Bio. Craniofac. Res. 2016, 6, 55–59.
- Moghaddam, A.A.; Radafshar, G.; Jahandideh, Y.; Kakaei, N. Clinical evaluation of effects of local application of Aloe vera gel as an adjunct to scaling and root planning in patients with chronic periodontitis. J. Dent. 2017, 18, 165–172.
- Ipshita, S.; Kurian, I.G.; Dileep, P.; Kumar, S.; Singh, P.; Pradeep, A.R. One percent alendronate and Aloe vera gel local host modulating agents in chronic periodontitis patients with class II furcation defects: A randomized, controlled clinical trial. J. Investig. Clin. Dent. 2018, 9, e12334.
- Kurian, I.G.; Dileep, P.; Ipshita, S.; Pradeep, A.R. Comparative evaluation of subgingivally-delivered 1% metformin and Aloe vera gel in the treatment of intrabony defects in chronic periodontitis patients: A randomized, controlled clinical trial. J. Investig. Clin. Dent. 2018, 9, e12324.
- Fallahi, H.R.; Hamadzade, H.; Nezhad, A.M.; Zandian, D.; Taghizadeh, M. Effect of Aloe vera mouthwash on postoperative complications after impacted third molar surgery: A randomized, double-blind clinical trial. J. Oral Maxillofac. Surg. Med. Path. 2016, 28, 392–396.
- Kalra, M.; Garg, N.; Rallan, M.; Pathivada, L.; Yeluri, R. Comparative evaluation of fresh Aloe barbadensis plant extract and mineral trioxide aggregate as pulpotomy agents in primary molars: A 12-month follow-up study. Contemp. Clin. Dent. 2017, 8, 106–111.
- Nimma, V.L.; Talla, H.V.; Bairi, J.K.; Gopaldas, M.; Bathula, H.; Vangdoth, S. Holistic healing through herbs: Effectiveness of Aloe vera on post extraction socket healing. J. Clin. Diagn. Res. 2017, 11, 83–86.
- Prabhakar, A.R.; Karuna, Y.M.; Yavagal, C.; Deepak, B.M. Cavity disinfection in minimally invasive dentistry-comparative evaluation of Aloe vera and propolis: A randomized clinical trial. Contemp. Clin. Dent. 2015, 6, S24–S31.
- Sahebjamee, M.; Mansourian, A.; Mohammad, M.H.; Zadeh, M.T.; Bekhradi, R.; Kazemian, A.; Doroudgar, K. Comparative efficacy of Aloe vera and benzydamine mouthwashes on radiation-induced oral mucositis: A triple-blind, randomised, controlled clinical trial. Oral Health Prev. Dent. 2015, 13, 309–315.
- Mansouri, P.; Haghighi, M.; Beheshtipour, N.; Ramzi, M. The effect of Aloe vera solution on chemotherapy-induced stomatitis in clients with lymphoma and leukemia: A randomized controlled clinical trial. Int. J. Community Nurs. Midwifery 2016, 4, 119–126.
- Anuradha, A.; Patil, B.; Asha, V.R. Evaluation of efficacy of Aloe vera in the treatment of oral submucous fibrosis–a clinical study. J. Oral Path. Med. 2017, 46, 50–55.
- Singh, N.; Hebbale, M.; Mhapuskar, A.; Ul, S.N.; Thopte, S.; Singh, S. Effectiveness of Aloe vera and Antioxidant along with Physiotherapy in the Management of Oral Submucous Fibrosis. J. Contemp. Dent. Pract. 2016, 17, 78–84.
- Panahi, Y.; Khedmat, H.; Valizadegan, G.; Mohtashami, R.; Sahebkar, A. Efficacy and safety of Aloe vera syrup for the treatment of gastroesophageal reflux disease: A pilot randomized positive-controlled trial. J. Tradit. Chin. Med. 2015, 35, 632–636.
- Park, C.H.; Son, H.U.; Yoo, C.Y.; Lee, S.H. Low molecular-weight gel fraction of Aloe vera exhibits gastroprotection by inducing matrix metalloproteinase-9 inhibitory activity in alcohol-induced acute gastric lesion tissues. Pharm. Biol. 2017, 55, 2110–2115.
- Sahebnasagh, A.; Ghasemi, A.; Akbari, J.; Alipour, A.; Lashkardoost, H.; Ala, S.; Salehifar, E. Successful treatment of acute radiation proctitis with Aloe vera: A preliminary randomized controlled clinical trial. J. Altern. Complement. Med. 2017, 23, 858–865.
- Størsrud, S.; Pontén, I.; Simrén, M. A pilot study of the effect of Aloe barbadensis Mill. extract (AVH200®) in patients with irritable bowel syndrome: A randomized, double-blind, placebo-controlled study. J. Gastrointestin. Liver Dis. 2015, 24, 275–280.
- Rahmani, N.; Khademloo, M.; Vosoughi, K.; Assadpour, S. Effects of Aloe vera cream on chronic anal fissure pain, wound healing and hemorrhaging upon defection: A prospective double blind clinical trial. Eur. Rev. Med. Pharmacol. Sci. 2014, 18, 1078–1084.
- Moriyama, M.; Moriyama, H.; Uda, J.; Kubo, H.; Nakajima, Y.; Goto, A.; Hayakawa, T. Beneficial effects of the genus Aloe on wound healing, cell proliferation, and differentiation of epidermal keratinocytes. PLoS ONE 2016, 11, e0164799.
- Hormozi, M.; Assaei, R.; Boroujeni, M.B. The effect of Aloe vera on the expression of wound healing factors (TGFβ1 and bFGF) in mouse embryonic fibroblast cell: In vitro study. Biomed. Pharm. 2017, 88, 610–616.
- Negahdari, S.; Galehdari, H.; Kesmati, M.; Rezaie, A.; Shariati, G. Wound healing activity of extracts and formulations of Aloe vera, henna, adiantum capillus-veneris, and myrrh on mouse dermal fibroblast cells. Int. J. Prevent. Med. 2017, 8, 18.
- Teplicki, E.; Ma, Q.; Castillo, D.E.; Zarei, M.; Hustad, A.P.; Chen, J.; Li, J. The Effects of Aloe vera on Wound Healing in Cell Proliferation, Migration, and Viability. Wounds 2018, 30, 263–268.
- De Oliveira, A.C.L.; Tabrez, S.; Shakil, S.; Khan, M.I.; Asghar, M.N.; Matias, B.D.; de Carvalho, R.M. Mutagenic, antioxidant and wound healing properties of Aloe vera. J. Ethnopharmacol. 2018, 227, 191–197.
- Curto, E.M.; Labelle, A.; Chandler, H.L. Aloe vera: An in vitro study of effects on corneal wound closure and collagenase activity. Vet. Ophthamol. 2014, 17, 403–410.
- Liu, F.W.; Liu, F.C.; Wang, Y.R.; Tsai, H.I.; Yu, H.P. Aloin protects skin fibroblasts from heat stress-induced oxidative stress damage by regulating the oxidative defense system. PLoS ONE 2015, 10, e0143528.
- Wahedi, H.M.; Jeong, M.; Chae, J.K.; Do, S.G.; Yoon, H.; Kim, S.Y. Aloesin from Aloe vera accelerates skin wound healing by modulating MAPK/Rho and Smad signaling pathways in vitro and in vivo. Phytomedicine 2017, 28, 19–26.
- Brandão, M.L.; Reis, P.R.M.; Araújo, L.A.D.; Araújo, A.C.V.; Santos, M.H.D.A.S.; Miguel, M.P. Evaluation of wound healing treated with latex derived from rubber trees and Aloe vera extract in rats. Acta Cir. Bras. 2016, 31, 570–577.
- Oryan, A.; Mohammadalipour, A.; Moshiri, A.; Tabandeh, M.R. Topical application of Aloe vera accelerated wound healing, modeling, and remodeling: An experimental study. Annals Plast. Surg. 2016, 77, 37–46.
- Takzaree, N.; Hadjiakhondi, A.; Hassanzadeh, G.; Rouini, M.R.; Manayi, A.; Zolbin, M.M. Transforming growth factor-β (TGF-β) activation in cutaneous wounds after topical application of Aloe vera gel. Can. J. Physiol. Pharm. 2016, 94, 1285–1290.
- Yos Adi Prakoso, K. The Effects of Aloe vera Cream on the Expression of CD4+ and CD8+ Lymphocytes in Skin Wound Healing. J. Trop. Med. 2018, 2018, 6218303.
- Sari, Y.; Purnawan, I.; Kurniawan, D.W.; Sutrisna, E. A comparative study of the effects of Nigella sativa oil gel and Aloe vera gel on wound healing in diabetic rats. J. Evid. Based Integr. Med. 2018, 23.
- Yao, R.; Tanaka, M.; Misawa, E.; Saito, M.; Nabeshima, K.; Yamauchi, K.; Furukawa, F. Daily Ingestion of Aloe vera Gel Powder Containing Aloe Sterols Prevents Skin Photoaging in OVX Hairless Mice. J. Food Sci. 2016, 81, 2849–2857.
- Saito, M.; Tanaka, M.; Misawa, E.; Yao, R.; Nabeshima, K.; Yamauchi, K.; Furukawa, F. Oral administration of Aloe vera gel powder prevents UVB-induced decrease in skin elasticity via suppression of overexpression of MMPs in hairless mice. Biosci. Biotech. Biochem. 2016, 80, 1416–1424.
- Misawa, E.; Tanaka, M.; Saito, M.; Nabeshima, K.; Yao, R.; Yamauchi, K.; Furukawa, F. Protective effects of Aloe sterols against UVB-induced photoaging in hairless mice. Photodermatol. Photoimmunomol. Photomed. 2017, 33, 101–111.
- Bala, S.; Chugh, N.A.; Bansal, S.C.; Garg, M.L.; Koul, A. Protective role of Aloe vera against X-ray induced testicular dysfunction. Andrologia 2017, 49, 12697.
- Bala, S.; Chugh, N.A.; Bansal, S.C.; Garg, M.L.; Koul, A. Radiomodulatory effects of Aloe vera on hepatic and renal tissues of X-ray irradiated mice. Mut. Res. 2018, 811, 1–15.
- Lin, L.X.; Wang, P.; Wang, Y.T.; Huang, Y.; Jiang, L.; Wang, X.M. Aloe vera and Vitis vinifera improve wound healing in an in vivo rat burn wound model. Mol. Med. Rep. 2016, 13, 1070–1076.
- Rodrigues, D.; Viotto, A.C.; Checchia, R.; Gomide, A.; Severino, D.; Itri, R.; Martins, W.K. Mechanism of Aloe vera extract protection against UVA: Shelter of lysosomal membrane avoids photodamage. Photochem. Photobiol. Sci. 2016, 15, 334–350.
- Avijgan, M.; Kamran, A.; Abedini, A. Effectiveness of Aloe vera gel in chronic ulcers in comparison with conventional treatments. Iran. J. Med. Sci. 2016, 41, S30.
- Leng, H.; Pu, L.; Xu, L.; Shi, X.; Ji, J.; Chen, K. Effects of Aloe polysaccharide, a polysaccharide extracted from Aloe vera, on TNF-α-induced HaCaT cell proliferation and the underlying mechanism in psoriasis. Mol. Med. Rep. 2018, 18, 3537–3543.
- Hekmatpou, D.; Mehrabi, F.; Rahzani, K.; Aminiyan, A. The effect of Aloe vera gel on prevention of pressure ulcers in patients hospitalized in the orthopedic wards: A randomized triple-blind clinical trial. BMC Complement. Altern. Med. 2018, 18, 1–11.
- Irani, P.S.; Varaie, S. Comparison of the effect of Aloe vera Gel and Nitrofurazone 2% on epithelialization and granulation tissue formation regarding superficial second-degree burns. Iran. J. Med. Sci. 2016, 41, S3.
- Molazem, Z.; Mohseni, F.; Younesi, M.; Keshavarzi, S. Aloe vera gel and cesarean wound healing; a randomized controlled clinical trial. Global J. Health Sci. 2015, 7, 203.
- Burusapat, C.; Supawan, M.; Pruksapong, C.; Pitiseree, A.; Suwantemee, C. Topical Aloe vera gel for accelerated wound healing of split-thickness skin graft donor sites: A double-blind, randomized, controlled trial and systematic review. Plast. Reconstr. Surg. 2018, 142, 217–226.
- Tanaka, M.; Yamamoto, Y.; Misawa, E.; Nabeshima, K.; Saito, M.; Yamauchi, K.; Furukawa, F. Aloe sterol supplementation improves skin elasticity in Japanese men with sunlight-exposed skin: A 12-week double-blind, randomized controlled trial. Clin. Cosmet. Invest. Dermat. 2016, 9, 435–442.
- Tanaka, M.; Misawa, E.; Yamauchi, K.; Abe, F.; Ishizaki, C. Effects of plant sterols derived from Aloe vera gel on human dermal fibroblasts in vitro and on skin condition in Japanese women. Clinical. Cosmet. Invest. Dermat. 2015, 8, 95–104.
- Tanaka, M.; Yamamoto, Y.; Misawa, E.; Nabeshima, K.; Saito, M.; Yamauchi, K.; Furukawa, F. Effects of aloe sterol supplementation on skin elasticity, hydration, and collagen score: A 12-week double-blind, randomized, controlled trial. Skin Pharmacol. Physiol. 2016, 29, 309–317.
- Ahmadloo, N.; Kadkhodaei, B.; Omidvari, S.; Mosalaei, A.; Ansari, M.; Nasrollahi, H.; Mohammadianpanah, M. Lack of prophylactic effects of Aloe vera gel on radiation induced dermatitis in breast cancer patients. Asian Pac. J. Cancer Prev. 2017, 18, 1139–1143.
- Hoopfer, D.; Holloway, C.; Gabos, Z.; Alidrisi, M.; Chafe, S.; Krause, B.; Hanson, J. Three-arm randomized phase III trial: Quality Aloe and placebo cream versus powder as skin treatment during breast cancer radiation therapy. Clin. Breast Cancer 2015, 15, 181–190.
- Ma, Y.; Tang, T.; Sheng, L.; Wang, Z.; Tao, H.; Zhang, Q.; Qi, Z. Aloin suppresses lipopolysaccharide-induced inflammation by inhibiting JAK1-STAT1/3 activation and ROS production in RAW264. 7 cells. Int. J. Mol. Med. 2018, 42, 1925–1934.
- Jiang, K.; Guo, S.; Yang, C.; Yang, J.; Chen, Y.; Shaukat, A.; Deng, G. Barbaloin protects against lipopolysaccharide (LPS)-induced acute lung injury by inhibiting the ROS-mediated PI3K/AKT/NF-κB pathway. Int. Immunopharm. 2018, 64, 140–150.
- Li, C.Y.; Suzuki, K.; Hung, Y.L.; Yang, M.S.; Yu, C.P.; Lin, S.P.; Fang, S.H. Aloe metabolites prevent LPS-induced sepsis and inflammatory response by inhibiting mitogen-activated protein kinase activation. Am. J. Chin. Med. 2017, 45, 847–861.
- Thunyakitpisal, P.; Ruangpornvisuti, V.; Kengkwasing, P.; Chokboribal, J.; Sangvanich, P. Acemannan increases NF-κB/DNA binding and IL-6/-8 expression by selectively binding Toll-like receptor-5 in human gingival fibroblasts. Carb. Polymers 2017, 161, 149–157.
- Na, H.S.; Song, Y.R.; Kim, S.; Heo, J.Y.; Chung, H.Y.; Chung, J. Aloin Inhibits Interleukin (IL)-1β− Stimulated IL-8 Production in KB Cells. J. Periodontol. 2016, 87, 108–115.
- Ahluwalia, B.; Magnusson, M.K.; Isaksson, S.; Larsson, F.; Öhman, L. Effects of Aloe barbadensis Mill. extract (AVH200®) on human blood T cell activity in vitro. J Ethnopharm. 2016, 179, 301–309.
- Werawatganon, D.; Linlawan, S.; Thanapirom, K.; Somanawat, K.; Klaikeaw, N.; Rerknimitr, R.; Siriviriyakul, P. Aloe vera attenuated liver injury in mice with acetaminophen-induced hepatitis. BMC Complement. Altern. Med. 2014, 14, 229.
- Capes-Davis, A.; Theodosopoulos, G.; Atkin, I.; Drexler, H.G.; Kohara, A.; MacLeod, R.A.; Freshney, R.I. Check your cultures! A list of cross-contaminated or misidentified cell lines. Int. J. Cancer 2010, 127, 1–8.
- Holliday, D.L.; Speirs, V. Choosing the right cell line for breast cancer research. Breast Cancer Res. 2011, 13, 215.
- Hussain, A.; Sharma, C.; Saniyah, K.; Kruti, S.; Shafiul, H. Aloe vera inhibits proliferation of human breast and cervical cancer cells and acts synergistically with cisplatin. Asian Pac. J. Cancer Prev. 2015, 16, 2939–2946.
- Luo, J.; Yuan, Y.; Chang, P.; Li, D.; Liu, Z.; Qu, Y. Combination of aloe-emodin with radiation enhances radiation effects and improves differentiation in human cervical cancer cells. Mol. Med. Rep. 2014, 10, 731–736.
- Chen, Q.; Tian, S.; Zhu, J.; Li, K.T.; Yu, T.H.; Yu, L.H.; Bai, D.Q. Exploring a novel target treatment on breast cancer: Aloe-emodin mediated photodynamic therapy induced cell apoptosis and inhibited cell metastasis. Anticancer Agents Med. Chem. 2016, 16, 763–770.
- Tseng, H.S.; Wang, Y.F.; Tzeng, Y.M.; Chen, D.R.; Liao, Y.F.; Chiu, H.Y.; Hsieh, W.T. Aloe-emodin enhances tamoxifen cytotoxicity by suppressing Ras/ERK and PI3K/mTOR in breast cancer cells. Am. J. Chin. Med. 2017, 45, 337–350.
- Trybus, W.; Krol, T.; Trybus, E.; Stachurska, A.; Kopacz-Bednarska, A.; Krol, G. Induction of mitotic catastrophe in human cervical cancer cells after administration of aloe-emodin. Anticancer Res. 2018, 38, 2037–2044.
- Shirali, S.; Barari, A.; Hosseini, S.A.; Khodadi, E. Effects of six weeks endurance training and Aloe vera supplementation on COX-2 and VEGF levels in mice with breast cancer. Asian Pac. J. Cancer Prev. 2017, 18, 31–36.
- Zhang, L.Q.; Lv, R.W.; Qu, X.D.; Chen, X.J.; Lu, H.S.; Wang, Y. Aloesin Suppresses Cell Growth and Metastasis in Ovarian Cancer SKOV3 Cells through the Inhibition of the MAPK Signaling Pathway. Anal. Cell Pathol. 2017, 2017.
- Liu, Y.Q.; Meng, P.S.; Zhang, H.C.; Liu, X.; Wang, M.X.; Cao, W.W.; Zhang, Z.G. Inhibitory effect of aloe emodin mediated photodynamic therapy on human oral mucosa carcinoma in vitro and in vivo. Biomed. Pharmacother. 2018, 97, 697–707.
- Chang, X.; Zhao, J.; Tian, F.; Jiang, Y.; Lu, J.; Ma, J.; Liu, K. Aloe-emodin suppresses esophageal cancer cell TE1 proliferation by inhibiting AKT and ERK phosphorylation. Oncol. Lett. 2016, 12, 2232–2238.
- Xu, C.; Xu, F. Radio sensitizing effect of Aloe polysaccharide on pancreatic cancer bxpc-3 cells. Pak. J. Pharm. Sci. 2016, 29, 1123–1126.
- Rawla, P.; Sunkara, T.; Barsouk, A. Epidemiology of colorectal cancer: Incidence, mortality, survival, and risk factors. Prz. Gastroenterol. 2019, 14, 89–103.
- Chen, Q.; Li, K.T.; Tian, S.; Yu, T.H.; Yu, L.H.; Lin, H.D.; Bai, D.Q. Photodynamic Therapy Mediated by Aloe-Emodin Inhibited Angiogenesis and Cell Metastasis Through Activating MAPK Signaling Pathway on HUVECs. Technol. Cancer Re. Treat. 2018, 17.
- Chihara, T.; Shimpo, K.; Kaneko, T.; Beppu, H.; Higashiguchi, T.; Sonoda, S.; Abe, F. Dietary Aloe vera gel powder and extract inhibit azoxymethane-induced colorectal aberrant crypt foci in mice fed a high-fat diet. Asian Pac. J. Cancer Prev. 2015, 16, 683–687.
- Ottaviani, G.; Jaffe, N. The epidemiology of osteosarcoma. Cancer Treat. Res. 2009, 152, 3–13.
- Li, K.T.; Chen, Q.; Wang, D.W.; Duan, Q.Q.; Tian, S.; He, J.W.; Bai, D.Q. Mitochondrial pathway and endoplasmic reticulum stress participate in the photosensitizing effectiveness of AE-PDT in MG 63 cells. Cancer Med. 2016, 5, 3186–3193.
- Tu, P.; Huang, Q.; Ou, Y.; Du, X.; Li, K.; Tao, Y.; Yin, H. Aloe-emodin-mediated photodynamic therapy induces autophagy and apoptosis in human osteosarcoma cell line MG-63 through the ROS/JNK signaling pathway. Oncol. Rep. 2016, 35, 3209–3215.
- Ali, Z.; Yousaf, N.; Larkin, J. Melanoma epidemiology, biology and prognosis. EJC Suppl. 2013, 11, 81–91.
- Tabolacci, C.; Cordella, M.; Turcano, L.; Rossi, S.; Lentini, A.; Mariotti, S.; De Maria, R. Aloe-emodin exerts a potent anticancer and immunomodulatory activity on BRAF-mutated human melanoma cells. Eur. J. Pharmacol. 2015, 762, 283–292.
- Damani, M.R.; Shah, A.R.; Karp, C.L.; Orlin, S.E. Treatment of ocular surface squamous neoplasia with topical Aloe vera drops. Cornea 2015, 34, 87–89.
- Koo, H.J.; Lee, K.R.; Kim, H.S.; Lee, B.M. Detoxification effects of Aloe polysaccharide and propolis on the urinary excretion of metabolites in smokers. Food Chem. Toxicol. 2019, 130, 99–108.
- Noor, A.; Gunasekaran, S.; Vijayalakshmi, M.A. Improvement of insulin secretion and pancreatic β-cell function in streptozotocin-induced diabetic rats treated with Aloe vera extract. Pharmacogn. Res. 2017, 9, 99.
- Arora, M.K.; Sarup, Y.; Tomar, R.; Singh, M.; Kumar, P. Amelioration of diabetes-induced diabetic nephropathy by Aloe vera: Implication of oxidative stress and hyperlipidemia. J. Diet. Suppl. 2019, 16, 227–244.
- Atiba, A.; Wasfy, T.; Abdo, W.; Ghoneim, A.; Kamal, T.; Shukry, M. Aloe vera gel facilitates re-epithelialization of corneal alkali burn in normal and diabetic rats. Clin. Ophthalmol. 2015, 9, 2019–2026.
- Kim, K.; Chung, M.H.; Park, S.; Cha, J.; Baek, J.H.; Lee, S.Y.; Choi, S.Y. ER stress attenuation by Aloe-derived polysaccharides in the protection of pancreatic β-cells from free fatty acid-induced lipotoxicity. Biochem. Biophys. Res. Commun. 2018, 500, 797–803.
- Alshatwi, A.A.; Subash-Babu, P. Aloe-Emodin Protects RIN-5F (Pancreatic β-cell) Cell from Glucotoxicity via Regulation of Pro-Inflammatory Cytokine and Downregulation of Bax and Caspase 3. Biomol. Ther. 2016, 24, 49–56.
- Alinejad-Mofrad, S.; Foadoddini, M.; Saadatjoo, S.A.; Shayesteh, M. Improvement of glucose and lipid profile status with Aloe vera in pre-diabetic subjects: A randomized controlled-trial. J. Diabetes Metab. Disord. 2015, 14, 22.
- Wang, H.C.; Brumaghim, J.L. Polyphenol compounds as antioxidants for disease prevention: Reactive oxygen species scavenging, Enzyme regulation, and metal chelation mechanisms in E. coli and human cells. In Oxidative Stress: Diagnostics, Prevention, and Therapy; American Chemical Society: Washington, DC, USA, 2011; pp. 99–175.
- Kumar, S.; Yadav, M.; Yadav, A.; Rohilla, P.; Yadav, J.P. Antiplasmodial potential and quantification of aloin and aloe-emodin in Aloe vera collected from different climatic regions of India. BMC Complement. Altern. Med. 2017, 17, 369.
- Cesar, V.; Jozić, I.; Begović, L.; Vuković, T.; Mlinarić, S.; Lepeduš, H.; Žarković, N. Cell-type-specific modulation of hydrogen peroxide cytotoxicity and 4-hydroxynonenal binding to human cellular proteins in vitro by antioxidant Aloe vera extract. Antioxidants 2018, 7, 125.
- Sun, Y.N.; Li, W.; Lee, S.H.; Jang, H.D.; Ma, J.Y.; Kim, Y.H. Antioxidant and anti-osteoporotic effects of anthraquinones and related constituents from the aqueous dissolved Aloe exudates. Nat. Prod. Res. 2017, 31, 2810–2813.
- Prueksrisakul, T.; Chantarangsu, S.; Thunyakitpisal, P. Effect of daily drinking of Aloe vera gel extract on plasma total antioxidant capacity and oral pathogenic bacteria in healthy volunteer: A short-term study. J. Complement. Integr. Med. 2015, 12, 159–164.
- Yang, M.; Li, L.; Heo, S.M.; Soh, Y. Aloe-emodin induces chondrogenic differentiation of ATDC5 cells via MAP kinases and BMP-2 signaling pathways. Biomol. Ther. 2016, 24, 395–401.
- Pengjam, Y.; Madhyastha, H.; Madhyastha, R.; Yamaguchi, Y.; Nakajima, Y.; Maruyama, M. NF-κB pathway inhibition by anthrocyclic glycoside aloin is key event in preventing osteoclastogenesis in RAW264. 7 cells. Phytomedicine 2016, 23, 417–428.
- Madhyastha, R.; Madhyastha, H.; Pengjam, Y.; Nurrahmah, Q.I.; Nakajima, Y.; Maruyama, M. The pivotal role of microRNA-21 in osteoclastogenesis inhibition by anthracycline glycoside aloin. J. Nat. Med. 2019, 73, 59–66.
- Yuksel, Y.; Guven, M.; Kaymaz, B.; Sehitoglu, M.H.; Aras, A.B.; Akman, T.; Cosar, M. Effects of Aloe vera on spinal cord Ischemia–Reperfusion injury of rats. J. Invest. Surg. 2016, 29, 389–398.
- Sahin, H.; Yener, A.U.; Karaboga, I.; Sehitoglu, M.H.; Dogu, T.; Altinisik, H.B.; Simsek, T. Protective effect of gel form of gastric gavage applicated Aloe vera on ischemia reperfusion injury in renal and lung tissue. Cell Mol. Biol. 2017, 63, 34–39.
- Zhang, P.; Liu, X.; Huang, G.; Bai, C.; Zhang, Z.; Li, H. Barbaloin pretreatment attenuates myocardial ischemia-reperfusion injury via activation of AMPK. Biochem. Biophys. Res. Commun. 2017, 490, 1215–1220.
- Esmat, A.Y.; Said, M.M.; Khalil, S.A. Aloin: A natural antitumor anthraquinone glycoside with iron chelating and non-atherogenic activities. Pharm. Biol. 2015, 53, 138–146.
- Furkan, M.; Alam, M.T.; Rizvi, A.; Khan, K.; Ali, A.; Naeem, A. Aloe emodin, an anthroquinone from Aloe vera acts as an anti aggregatory agent to the thermally aggregated hemoglobin. Spectrochim. Acta Part A: Mol. Biomol. Spectrosc. 2017, 179, 188–193.
- Ji, H.; Liu, Y.; He, F.; An, R.; Du, Z. LC–MS based urinary metabolomics study of the intervention effect of aloe-emodin on hyperlipidemia rats. J. Pharm. Biomed. Anal. 2018, 156, 104–115.
- Guven, M.; Gölge, U.H.; Aslan, E.; Sehitoglu, M.H.; Aras, A.B.; Akman, T.; Cosar, M. The effect of Aloe vera on ischemia—Reperfusion injury of sciatic nerve in rats. Biomed. Pharmacother. 2016, 79, 201–207.
- Saddiq, A.A.; Al-Ghamdi, H. Aloe vera extract: A novel antimicrobial and antibiofilm against methicillin resistant Staphylococcus aureus strains. Pak. J. Pharm. Sci. 2018, 31, 2123–2130.
- Jain, S.; Rathod, N.; Nagi, R.; Sur, J.; Laheji, A.; Gupta, N.; Prasad, S. Antibacterial Effect of Aloe vera Gel against Oral Pathogens: An In-vitro Study. J. Clin. Diagn. Res. 2016, 10, 41–44.
- Xiang, H.; Cao, F.; Ming, D.; Zheng, Y.; Dong, X.; Zhong, X.; Wang, L. Aloe-emodin inhibits Staphylococcus aureus biofilms and extracellular protein production at the initial adhesion stage of biofilm development. Appl. Microbiol. Biotechnol. 2017, 101, 6671–6681.
- Goudarzi, M.; Fazeli, M.; Azad, M.; Seyedjavadi, S.S.; Mousavi, R. Aloe vera gel: Effective therapeutic agent against multidrug-resistant Pseudomonas aeruginosa isolates recovered from burn wound infections. Chemother. Res. Pract. 2015, 2015.
- Cataldi, V.; Di Bartolomeo, S.; Di Campli, E.; Nostro, A.; Cellini, L.; Di Giulio, M. In vitro activity of Aloe vera inner gel against microorganisms grown in planktonic and sessile phases. Int. J. Immunopathol. Pharmacol. 2015, 28, 595–602.
- Karkare, S.R.; Ahire, N.P.; Khedkar, S.U. Comparative evaluation of antimicrobial activity of hydroalcoholic extract of Aloe vera, garlic, and 5% sodium hypochlorite as root canal irrigants against Enterococcus faecalis: An in vitro study. J. Indian Soc. Pedod. Prev. Dent. 2015, 33, 274–278.
- Arjomandzadegan, M.; Emami, N.; Habibi, G.; Farazi, A.A.; Kahbazi, M.; Sarmadian, H.; Jabbari, M.; Hosseini, H.; Ramezani, M. Antimycobacterial activity assessment of three ethnobotanical plants against Mycobacterium Tuberculosis: An In Vitro study. Int. J. Mycobacteriol. 2016, 1, 108–109.
- Rezazadeh, F.; Moshaverinia, M.; Motamedifar, M.; Alyaseri, M. Assessment of Anti HSV-1 Activity of Aloe vera Gel Extract: An In Vitro Study. J. Dent. 2016, 17, 49–54.
- Sun, Z.; Yu, C.; Wang, W.; Yu, G.; Zhang, T.; Zhang, L.; Zhang, J.; Wei, K. Aloe Polysaccharides Inhibit Influenza A Virus Infection-A Promising Natural Anti-flu. Drug. Front. Microbiol. 2018, 9, 2338.
- Gullón, B.; Gullón, P.; Tavaria, F.; Alonso, J.L.; Pintado, M. In vitro assessment of the prebiotic potential of Aloe vera mucilage and its impact on the human microbiota. Food Funct. 2015, 6, 525–531.
- Quezada, M.P.; Salinas, C.; Gotteland, M.; Cardemil, L. Acemannan and Fructans from Aloe vera (Aloe barbadensis Miller) Plants as Novel Prebiotics. J. Agric. Food Chem. 2017, 65, 10029–10039.
- Asgharzade, S.; Rafieian-Kopaei, M.; Mirzaeian, A.; Reiisi, S.; Salimzadeh, L. Aloe vera toxic effects: Expression of inducible nitric oxide synthase (iNOS) in testis of Wistar rat. Iran. J. Basic Med. Sci. 2015, 18, 967–973.
- Erhabor, J.O.; Idu, M. Aphrodisiac potentials of the ethanol extract of Aloe barbadensis Mill. root in male Wistar rats. BMC Complement. Altern. Med. 2017, 17, 360.
- Behmanesh, M.A.; Najafzadehvarzi, H.; Poormoosavi, S.M. Protective Effect of Aloe vera Extract against Bisphenol A Induced Testicular Toxicity in Wistar Rats. Cell 2018, 20, 278–283.
- Lee, D.; Kim, H.S.; Shin, E.; Do, S.G.; Lee, C.K.; Kim, Y.M.; Lee, M.B.; Min, K.Y.; Koo, J.; Kim, S.J.; et al. Polysaccharide isolated from Aloe vera gel suppresses ovalbumin-induced food allergy through inhibition of Th2 immunity in mice. Biomed. Pharmacother. 2018, 101, 201–210.
- Im, S.A.; Kim, K.H.; Kim, H.S.; Lee, K.H.; Shin, E.; Do, S.G.; Jo, T.H.; Park, Y.I.; Lee, C.K. Processed Aloe vera gel ameliorates cyclophosphamide-induced immunotoxicity. Int. J. Mol. Sci. 2014, 15, 19342–19354.
- Iftkhar, A.; Hasan, I.J.; Sarfraz, M.; Jafri, L.; Ashraf, M.A. Nephroprotective Effect of the Leaves of Aloe barbadensis (Aloe vera) against Toxicity Induced by Diclofenac Sodium in Albino Rabbits. West Indian Med. J. 2015, 64, 462–467.
- Hashiguchi, M.; Suzuki, K.; Kaneko, K.; Nagaoka, I. Effect of aloe-emodin on the proliferation and apoptosis of human synovial MH7A cells; a comparison with methotrexate. Mol. Med. 2017, 15, 4398–4404.
- Aro, A.A.; Esquisatto, M.A.; Nishan, U.; Perez, M.O.; Rodrigues, R.A.; Foglio, M.A.; Carvalho, J.E.; Gomes, L.; Vidal Bde, C.; Pimentel, E.R. Effect of Aloe vera application on the content and molecular arrangement of glycosaminoglycans during calcaneal tendon healing. Microsc. Res. Tech. 2014, 77, 964–973.
- Shahraki, M.R.; Mirshekari, H.; Sabri, A. Aloe vera Aqueous Extract Effect on Morphine Withdrawal Syndrome in Morphine-Dependent Female Rats. Int. J. High Risks Behav. Addict. 2014, 3, e11358.
- Koul, A.; Bala, S.; Yasmeen Arora, N. Aloe vera affects changes induced in pulmonary tissue of mice caused by cigarette smoke inhalation. Environ. Toxicol. 2015, 30, 999–1013.
More
Information
Subjects:
Plant Sciences
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
4.1K
Revisions:
3 times
(View History)
Update Date:
27 Jul 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





