
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Cătălina Ionescu | -- | 2613 | 2022-07-22 18:35:45 | | | |
| 2 | Conner Chen | + 3 word(s) | 2616 | 2022-07-25 05:58:49 | | | | |
| 3 | Conner Chen | Meta information modification | 2616 | 2022-07-25 06:12:28 | | | | |
| 4 | Conner Chen | Meta information modification | 2616 | 2022-07-28 10:26:00 | | | | |
| 5 | Conner Chen | Meta information modification | 2616 | 2022-07-28 10:29:31 | | |
Video Upload Options
Angiogenesis is the process of developing new blood vessels from pre-existing ones.
1. Formation and Remodeling of Blood Vessels
2. The Angiogenic Balance: Synthetic and Endogenous Regulators
2.1. Synthetic Modulators of Angiogenesis
2.2. Endogenous Regulators of Angiogenesis
| Activator | Description/Structure | Receptor(s)/Cellular Targets | Mechanism of Action |
References |
|---|---|---|---|---|
| FGF family |
|
|
|
[32][43][44][45][46][47] |
| VEGF family |
|
|
|
[31][32][48][49][50] |
| Ang 1 |
|
|
|
[32][51][52][53][54] |
| Ephrins |
|
|
|
[32][55][56][57] |
| MMPs |
|
|
|
[32][58][59][60] |
| Inhibitor | Description/Structure | Receptor(s)/Cellular Targets | Mechanism of Action | References |
|---|---|---|---|---|
| Endostatin |
|
|
|
[35][61][62][63] |
| Tumstatin |
|
|
|
[35][64] |
| Angiostatin |
|
|
|
[35][65][66][67] |
| TSPs |
|
|
|
[35][41][42][68][69][70][71] |
| 2-ME |
|
|
|
[35][72][73] |
3. Physiological and Pathological Angiogenesis
The balance of activators and inhibitors is shown in Figure 2. Besides its role in embryonic development, angiogenesis appears as a normal process in adults, in female reproductive functions [83][84][85][86][87] and in tissue regeneration (ex. wounds healing) [88] (Figure 2B). Under certain conditions, it can appear as a disequilibrium in the synthesis of the endogenous factors that control angiogenesis, and an abnormal angiogenesis can occur. It can be either insufficient, leading to the impossibility of the body healing wounds or participating in normal organ regeneration, or it can lead to the ischemia of a part of the body, such as myocardial, peripheral of intestinal ischemia. Other complications include ulcers, infertility and hair loss (Figure 2A).
As mentioned above, excessive angiogenesis can favor tumor growth and metastasis appearance or it can induce the evolution of diseases such as rheumatoid arthritis, psoriasis, etc. (Figure 2C) [89][90].
Excessive angiogenesis is also linked to a series of eye diseases, which can lead to blindness. It is the cause of visual loss in the case of age-related macular degeneration. Patients who suffer from proliferative diabetic retinopathy are known to have higher VEGF levels when compared to healthy persons [91]. Increased VEGF levels cause uncontrolled angiogenesis in these patients.
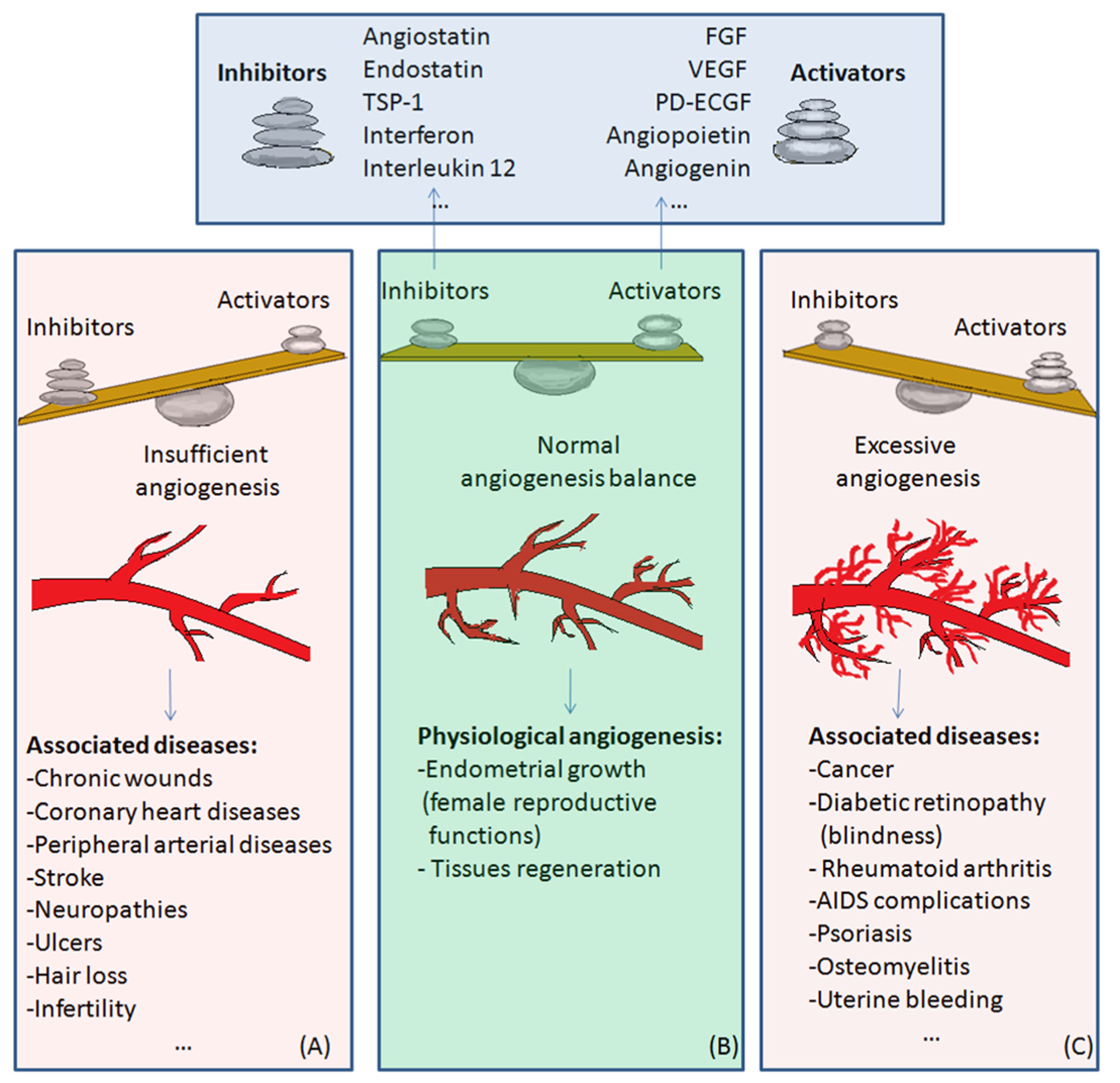
Figure 2. The balance of activators and inhibitors in: (A)—insufficient angiogenesis; (B)—normal angiogenesis; (C)—excessive angiogenesis. Abbreviations: FGF: fibroblast growth factor, VEGF: vascular endothelial growth factor, PD-ECGF: platelet-derived endothelial cell growth factor, TSP-1: thrombospondin-1. Normal angiogenesis is the balanced action of angiogenesis activators and inhibitors. In the case of preponderant action of angiogenesis inhibitors, insufficient angiogenesis appears, leading to diseases such as chronic wounds, cardiovascular diseases, neuropathies, ulcers, hair loss, and infertility (Figure 2A). Physiological angiogenesis appears as a normal process in female reproductive functions and in tissue regeneration (Figure 2B). On the contrary, if the action of angiogenesis activators prevails, complications in diseases such as cancer, diabetic retinopathy, rheumatoid arthritis, AIDS, psoriasis, osteomyelitis or uterine bleeding may appear (Figure 2C).
References
- Eguchi, M.; Masuda, H.; Asahara, T. Endothelial progenitor cells for postnatal vasculogenesis. Clin. Exp. Nephrol. 2007, 11, 18–25.
- Murasawa, S.; Asahara, T. Endothelial Progenitor Cells for Vasculogenesis. Physiology 2005, 20, 36–42.
- Asahara, T.; Masuda, H.; Takahashi, T.; Kalka, C.; Pastore, C.; Silver, M.; Kearne, M.; Magner, M.; Isner, J.M. Bone marrow origin of endothelial progenitor cells responsible for postnatal vasculogenesis in physiological and pathological neovascularization. Circ. Res. 1999, 85, 221–228.
- Carmeliet, P. Angiogenesis in health and disease. Nat. Med. 2003, 9, 653–660.
- Djonov, V.; Baum, O.; Burri, P.H. Vascular remodeling by intussusceptive angiogenesis. Cell Tissue Res. 2003, 314, 107–117.
- Djonov, V.; Schmid, M.; Tschanz, S.A.; Burri, P.H. Intussusceptive Angiogenesis: Its Role in Embryonic Vascular Network Formation. Circ. Res. 2000, 86, 286–292.
- Tomanek, R.J.; Schatteman, G.C. Angiogenesis: New insights and therapeutic potential. Anat. Rec. 2000, 261, 126–135.
- Couffinhal, T.; Dufourcq, P.; Daret, D.; Duplaa, C. The mechanisms of angiogenesis. Medical and therapeutic applications. Rev. Méd. Interne 2001, 22, 1064–1082.
- Bussolino, F.; Mantovani, A.; Persico, G. Molecular mechanisms of blood vessel formation. Trends Biochem. Sci. 1997, 22, 251–256.
- Ribatti, D.; Crivellato, E. “Sprouting angiogenesis”, a reappraisal. Dev. Biol. 2012, 372, 157–165.
- Tanigawa, N.; Amaya, H.; Matsumura, M.; Shimomatsuya, T.; Horiuchi, T.; Muraoka, R.; Iki, M. Extent of tumor vascularization correlates with prognosis and hematogenous metastasis in gastric carcinomas. Cancer Res. 1996, 56, 2671–2676.
- Scholz, D.; Cai, W.J.; Schaper, W. Arteriogenesis, a new concept of vascular adaptation in occlusive disease. Angiogenesis 2001, 4, 247–257.
- Heil, M.; Wagner, S.; Schaper, W. Arterial regeneration by collateral artery growth (arteriogenesis). Drug Discov. Today Dis. Models 2004, 1, 265–271.
- Stephan, D.; Weltin, D.; Zaric, V.; Chapelon, D.; Da Silva, A.; Lugnier, C. Angiogenèse: De la physiologie à la thérapeutique. Réanim. Urgences 2000, 9, 534–544.
- Levy, A.P.; Levy, N.S.; Goldberg, N.A. Post-transcriptional Regulation of Vascular Endothelial Growth Factor by Hypoxia. J. Biol. Chem. 1996, 271, 2746–2753.
- Rosca, E.V.; Koskimaki, J.E.; Rivera, C.G.; Pandey, N.B.; Tamiz, A.P.; Popel, A.S. Anti-angiogenic peptides for cancer therapeutics. Curr. Pharm. Biotechnol. 2011, 12, 1101–1116.
- Fan, T.P.; Jaggar, R.; Bicknell, R. Controlling the vasculature: Angiogenesis, anti-angiogenesis and vascular targeting of gene therapy. Trends Pharmacol. Sci. 1995, 16, 57–66.
- Quesada, A.R.; Munoz-Chapuli, R.; Medina, M.A. Anti-Angiogenic Drugs: From Bench to Clinical Trials. Med. Res. Rev. 2006, 26, 483–530.
- Nangia-Makker, P.; Baccarini, S.; Raz, A. Carbohydrate-recognition and angiogenesis. Cancer Metastasis Rev. 2000, 19, 51–57.
- Funasaka, T.; Raz, A.; Nangia-Makker, P. Galectin-3 in angiogenesis and metastasis. Glycobiology 2014, 24, 886–891.
- Nangia-Makker, P.; Hogan, V.; Honjo, Y.; Baccarini, S.; Tait, L.; Bresalier, R.; Raz, A. Inhibition of human cancer cell growth and metastasis in nude mice by oral intake of modified citrus pectin. J. Natl. Cancer. Inst. 2002, 94, 1854–1862.
- Johnstone, K.D.; Karoli, T.; Liu, L.; Dredge, K.; Copeman, E.; Li, C.P.; Davis, K.; Hammond, E.; Bytheway, I.; Kostewicz, E.; et al. Synthesis and biological evaluation of polysulfated oligosaccharide glycosides as inhibitors of angiogenesis and tumor growth. J. Med. Chem. 2010, 53, 1686–1699.
- Barragan-Montero, V.; Awwad, A.; Combemale, S.; de Santa Barbara, P.; Jover, B.; Molès, J.P.; Montero, J.L. Synthesis of Mannose-6-Phosphate Analogues and their Utility as Angiogenesis Regulators. ChemMedChem 2011, 6, 1771–1774.
- Ionescu, C.; Sippelli, S.; Toupet, L.; Barragan-Montero, V. New mannose derivatives: The tetrazole analogue of mannose-6-phosphate as angiogenesis inhibitor. Bioorg. Med. Chem. Lett. 2016, 26, 636–639.
- Combemale, S.; Assam-Evoung, J.N.; Houaidji, S.; Bibi, R.; Barragan-Montero, V. Gold Nanoparticles Decorated with Mannose-6-phosphate Analogues. Molecules 2014, 19, 1120–1149.
- Volpert, O.; Jackson, D.; Bouck, N.; Linzer, D.I. The insulin-like growth factor II/Mannose 6 -phosphate receptor is required for proliferin-induced angiogenesis. Endocrinology 1996, 137, 3871–3876.
- Doyagüez, G.E.; Carrero, P.; Madrona, A.; Rodriguez-Salamanca, P.; Martínez-Gualda, B.; Camarasa, M.J.; Jimeno, M.L.; Bennallack, P.R.; Finnell, J.G.; Tsang, T.M.; et al. Galloyl Carbohydrates with Antiangiogenic Activity Mediated by Capillary Morphogenesis Gene 2 (CMG2) Protein Binding. J. Med. Chem. 2019, 62, 3958–3970.
- Cryan, L.M.; Bazinet, L.; Habeshian, K.A.; Cao, S.; Clardy, J.; Christensen, K.A.; Rogers, M.S. 1,2,3,4,6-Penta-O-galloyl-β-D-glucopyranose inhibits angiogenesis via inhibition of capillary morphogenesis gene 2. J. Med. Chem. 2013, 56, 1940–1945.
- Huh, J.E.; Lee, E.O.; Kim, M.S.; Kang, K.S.; Kim, C.H.; Cha, B.C.; Surh, Y.J.; Kim, S.H. Penta-O-galloyl-beta-D-glucose suppresses tumor growth via inhibition of angiogenesis and stimulation of apoptosis: Roles of cyclooxygenase-2 and mitogen-activated protein kinase pathways. Carcinogenesis 2005, 26, 1436–1445.
- Al Sabti, H. Therapeutic angiogenesis in cardiovascular disease. J. Cardiothorac. Surg. 2007, 2, 49.
- Pandya, N.M.; Dhalla, N.S.; Santani, D.D. Angiogenesis—A new target for future therapy. Vascul. Pharmacol. 2006, 44, 265–274.
- Bouıs, D.; Kusumanto, Y.; Meijer, C.; Mulder, N.H.; Hospers, G.A. A review on pro- and anti-angiogenic factors as targets of clinical intervention. Pharmacol. Res. 2006, 53, 89–103.
- Al Kawas, H.; Saaid, I.; Jank, P.; Westhoff, C.C.; Denkert, C.; Pross, T.; Weiler, K.B.S.; Karsten, M.M. How VEGF-A and its splice variants affect breast cancer development—clinical implications. Cell Oncol. 2022, 45, 227–239.
- Lopes-Coelho, F.; Martins, F.; Pereira, S.A.; Jacinta Serpa, J. Anti-Angiogenic Therapy: Current Challenges and Future Perspectives. Int. J. Mol. Sci. 2021, 22, 3765.
- Nyberg, P.; Xie, L.; Kalluri, R. Endogenous Inhibitors of Angiogenesis. Cancer Res. 2005, 65, 3967–3979.
- Iruela-Arispe, M.L.; Dvorak, H.F. Angiogenesis: A dynamic balance of stimulators and inhibitors. Thromb. Haemost. 1997, 78, 672–677.
- Gospodarowicz, D. Purification of a fibroblast growth factor from bovine pituitary. J. Biol. Chem. 1975, 250, 2515–2520.
- Esch, F.; Baird, A.; Ling, N.; Ueno, N.; Hill, F.; Denoroy, L.; Klepper, R.; Gospodarowicz, D.; Böhlen, P.; Guillemin, R. Primary structure of bovine pituitary basic fibroblast growth factor (FGF) and comparison with the amino-terminal sequence of bovine brain acidic FGF. Proc. Natl. Acad. Sci. USA 1985, 82, 6507–6511.
- Senger, D.R.; Galli, S.J.; Dvorak, A.M.; Perruzzi, C.A.; Harvey, V.S.; Dvorak, H.F. Tumor cells secrete a vascular permeability factor that promotes accumulation of ascites fluid. Science 1983, 219, 983–9855.
- Leung, D.W.; Cachianes, G.; Kuang, W.J.; Goeddel, D.V.; Ferrara, N. Vascular endothelial growth factor is a secreted angiogenic mitogen. Science 1989, 246, 1306–1309.
- Guo, N.; Krutzsch, H.C.; Inman, J.K.; Roberts, D.D. Thrombospondin 1 and type I repeat peptides of thrombospondin 1 specifically induce apoptosis of endothelial cells. Cancer Res. 1997, 57, 1735–1742.
- Good, D.J.; Polverini, P.J.; Rastinejad, F.; Le Beau, M.M.; Lemons, R.S.; Frazier, W.A.; Bouck, N.P. A tumor suppressor-dependent inhibitor of angiogenesis is immunologically and functionally indistinguishable from a fragment of thrombospondin. Proc. Natl. Acad. Sci. USA 1990, 87, 6624–6628.
- Manetti, F.; Corelli, F.; Botta, M. Fibroblast growth factors and their inhibitors. Curr. Pharm. Des. 2000, 6, 1897–1924.
- Zakrzewska, M.; Marcinkowska, E.; Wiedlocha, A. FGF-1: From biology through engineering to potential medical applications. Crit. Rev. Clin. Lab. Sci. 2008, 45, 91–135.
- Yayon, A.; Klagsbrun, M.; Esko, J.D.; Leder, P.; Omitz, D.M. Cell surface, heparin-like molecules are required for binding of basic fibroblast growth factor to its high affinity receptor. Cell 1991, 64, 841–848.
- Roghani, M.; Mansukhani, A.; Dell’Era, P.; Bellosta, P.; Basilico, C.; Rifkin, D.B.; Moscatelli, D. Heparin increases the affinity of basic fibroblast growth factor for its receptor but is not required for binding. J. Biol. Chem. 1994, 269, 3976–3984.
- Friesel, R.E.; Maciag, T. Molecular mechanisms of angiogenesis: Fibroblast growth factor signal transduction. FASEB J. 1995, 9, 919–925.
- Hagedorn, M.; Bikfalvi, A. Target molecules for anti-angiogenic therapy: From basic research to clinical trials. Crit. Rev. Oncol. Hematol. 2000, 34, 89–110.
- Meyer, M.; Clauss, M.; Lepple-Wienhues, A.; Waltenberger, J.; Augustin, H.G.; Ziche, M.; Lanz, C.; Büttner, M.; Rziha, H.J.; Dehio, C. A novel vascular endothelial growth factor encoded by Orf virus, VEGF-E, mediates angiogenesis via signalling through VEGFR-2 (KDR) but not VEGFR-1 (Flt-1) receptor tyrosine kinases. EMBO J. 1999, 18, 363–374.
- Veikkola, T.; Alitalo, K. VEGFs, receptors and angiogenesis. Semin. Cancer Bio. 1999, 9, 211–220.
- Koblizek, T.I.; Weiss, C.; Yancopoulos, G.D.; Deutsch, U.; Risau, W. Angiopoietin-1 induces sprouting angiogenesis in vitro. Curr. Biol. 1998, 8, 529–532.
- Maisonpierre, P.C.; Suri, C.; Jones, P.F.; Bartunkova, S.; Wiegand, S.J.; Radziejewski, C.; Compton, D.; McClain, J.; Aldrich, T.H.; Papadopoulos, N.; et al. Angiopoietin-2, a natural antagonist for Tie2 that disrupts in vivo angiogenesis. Science 1997, 277, 55–60.
- Yu, X.; Seegar, T.M.C.; Dalton, A.C.; Tzvetkova-Robev, D.; Goldgur, Y.; Rajashankar, K.R.; Nikolov, D.B.; Barton, W.A. Structural basis for angiopoietin-1–mediated signaling initiation. Proc. Natl. Acad. Sci. USA 2013, 110, 7205–7210.
- Fagiani, E.; Christofori, G. Angiopoietins in angiogenesis. Cancer Lett. 2013, 328, 18–26.
- Cheng, N.; Brantley, D.M.; Chen, J. The ephrins and Eph receptors in angiogenesis. Cytokine Growth Factor Rev. 2002, 13, 75–85.
- Salvucci, O.; Tosato, G. Essential roles of EphB receptors and EphrinB ligands in endothelial cell function and angiogenesis. Adv. Cancer Res. 2012, 114, 21–57.
- Kullander, K.; Klein, R. Mechanisms and functions of Eph and ephrin signalling. Nat. Rev. Mol. Cell Biol. 2002, 3, 475–486.
- Zitka, O.; Kukacka, J.; Krizkova, S.; Huska, D.; Adam, V.; Masarik, M.; Prusa, R.; Kizek, R. Matrix metalloproteinases. Curr. Med. Chem. 2010, 17, 3751–3768.
- Johnson, L.L.; Dyer, R.; Hupe, D.J. Matrix metalloproteinases. Curr. Opin. Chem. Biol. 1998, 2, 466–471.
- Boire, A.; Covic, L.; Agarwal, A.; Jacques, S.; Sherifi, S.; Kuliopulos, A. PAR1 is a matrix metalloprotease-1 receptor that promotes invasion and tumorigenesis of breast cancer cells. Cell 2005, 120, 303–313.
- Sasaki, T.; Larsson, H.; Kreuger, J.; Salmivirta, M.; Claesson-Welsh, L.; Lindahl, U.; Hohenester, E.; Timpl, R. Structural basis and potential role of heparin/heparan sulfate binding to the angiogenesis inhibitor endostatin. EMBO J. 1999, 18, 6240–6248.
- O’Reilly, M.S.; Boehm, T.; Shing, Y.; Fukai, N.; Vasios, G.; Lane, W.S.; Flynn, E.; Birkhead, J.R.; Olsen, B.R.; Folkman, J. Endostatin: An endogenous inhibitor of angiogenesis and tumor growth. Cell 1997, 88, 277–285.
- Kim, Y.M.; Jang, J.W.; Lee, O.H.; Yeon, J.; Choi, E.Y.; Kim, K.W.; Lee, S.-T.; Kwon, Y.G. Endostatin inhibits endothelial and tumor cellular invasion by blocking the activation and catalytic activity of matrix metalloproteinase. Cancer Res. 2000, 60, 5410–5413.
- Sudhakar, A.; Sugimoto, H.; Yang, C.; Lively, J.; Zeisberg, M.; Kalluri, R. Human tumstatin and human endostatin exhibit distinct antiangiogenic activities mediated by αvβ3 and α5β1 integrins. Proc. Natl. Acad. Sci. USA 2003, 100, 4766–4771.
- O’Reilly, M.S.; Holmgren, L.; Shing, Y.; Chen, C.; Rosenthal, R.A.; Moses, M.; Lane, W.S.; Cao, Y.; Sage, E.; Folkman, J. Angiostatin: A novel angiogenesis inhibitor that mediates the suppression of metastases by a Lewis lung carcinoma. Cell 1994, 79, 315–328.
- Geiger, J.H.; Cnudde, S.E. What the structure of angiostatin may tell us about its mechanism of action. J. Thromb. Haemost. 2004, 2, 23–34.
- Troyanovsky, B.; Levchenko, T.; Mansson, G.; Matvijenko, O.; Holmgren, L. Angiomotin: An angiostatin binding protein that regulates endothelial cell migration and tube formation. J. Cell Biol. 2001, 152, 1247–1254.
- Iruela-Arispe, M.L.; Lombardo, M.; Krutzsch, H.C.; Lawler, J.; Roberts, D.D. Inhibition of angiogenesis by thrombospondin-1 is mediated by 2 independent regions within the type 1 repeats. Circulation 1999, 100, 1423–1431.
- Adams, J.; Lawler, J. The thrombospondin family. Curr. Biol. 1993, 3, 188–190.
- Bornstein, P. Thrombospondins function as regulators of angiogenesis. J. Cell Commun. Signal 2009, 3, 189–200.
- Mirochnik, Y.; Kwiatek, A.; Volpert, O.V. Thrombospondin and apoptosis: Molecular mechanisms and use for design of complementation treatments. Curr. Drug Targets 2008, 9, 851–862.
- Pribluda, V.S.; Gubish, E.R., Jr.; Lavallee, T.M.; Treston, A.; Swartz, G.M.; Green, S.J. 2-Methoxyestradiol: An endogenous antiangiogenic and antiproliferative drug candidate. Cancer Metastasis Rev. 2000, 19, 173–179.
- Yue, T.L.; Wang, X.; Louden, C.S.; Gupta, S.; Pillarisetti, K.; Gu, J.L.; Hart, T.K.; Lysko, P.G.; Feuerstein, G.Z. 2-Methoxyestradiol, an endogenous estrogen metabolite, induces apoptosis in endothelial cells and inhibits angiogenesis: Possible role for stress-activated protein kinase signaling pathway and Fas expression. Mol. Pharmacol. 1997, 51, 951–962.
- Peach, C.J.; Mignone, V.W.; Arruda, M.A.; Diana, C.; Alcobia, D.C.; Stephen, J.; Hill, S.J.; Kilpatrick, L.E.; Woolard, J. Molecular Pharmacology of VEGF-A Isoforms: Binding and Signalling at VEGFR2. Int. J. Mol. Sci. 2018, 19, 1264.
- Zhou, Y.; Zhu, X.; Cui, H.; Shi, J.; Yuan, G.; Shi, S.; Hu, Y. The Role of the VEGF Family in Coronary Heart Disease. Front. Cardiovasc. Med. 2021, 8, 738325.
- Ferrara, N.; Adamis, A.P. Ten years of anti-vascular endothelial growth factor therapy. Nat. Rev. Drug Discov. 2016, 15, 385–403.
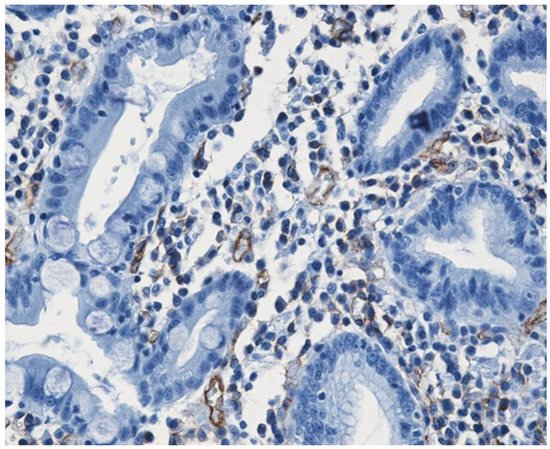
- Mateescu, G.O.; Comanescu, M.; Mehedinţi, R.; Niculescu, Z.; Bold, A.; Panduru, L.; Cernea, D. Immunohistochemical expression of growth factors in the exocrine pancreas of patients with chronic liver diseases. Rom. J. Morphol. Embryol. 2010, 51, 303–307.
- Braile, M.; Marcella, S.; Cristinziano, L.; Galdiero, M.R.; Luca Modestino, L.; Ferrara, A.L.; Varricchi, G.; Marone, G.; Loffredo, S. VEGF-A in Cardiomyocytes and Heart Diseases. Int. J. Mol. Sci. 2020, 21, 5294.
- Oliver, R.C.; Tervonen, T. Diabetes-a risk factor for periodontitis in adults? J. Periodontol. 1994, 65, 530–538.
- Yalda, B.; Offenbacher, S.; Collins, J.G. Diabetes as a modifier of periodontal disease expression. Periodontology 2000 1994, 6, 37–49.
- Minchenko, A.; Bauer, T.; Salceda, S.; Caro, J. Hypoxic stimulation of vascular endothelial growth factor expression in vitro and in vivo. Lab. Investig. 1994, 71, 374–379. Available online: https://pubmed.ncbi.nlm.nih.gov/7933988/ (accessed on 4 July 2022).
- Teshima-Kondo, S.; Kondo, K.; Prado-Lourenco, L.; Gonzalez-Herrera, I.; Rokutan, K.; Bayard, F.; Arnal, J.F.; Prats, A.C. Hyperglycemia up-regulates translation of the fibroblast growth factor 2 mRNA in mouse aorta via internal ribosome entry site. FASEB J. 2004, 18, 1583–1585.
- Groothius, P.G. Angiogenesis and vascular remodelling in female reproductive organs. Angiogensis 2005, 8, 87–88.
- Gargett, C.E.; Rogers, P.A.W. Human endometrial angiogenesis. Reproduction 2001, 121, 181–186.
- Okada, H.; Tsuzuki, T.; Shindoh, H.; Nishigaki, A.; Yasuda, K.; Kanzaki, H. Regulation of decidualization and angiogenesis in the human endometrium: Mini review. J. Obstet. Gynaecol. Res. 2014, 40, 1180–1187.
- Chung, A.S.; Lee, J.; Ferrara, N. Targeting the tumour vasculature: Insights from physiological angiogenesis. Nat. Rev. Cancer 2010, 10, 505–514.
- Boldeanu, L.; Dijmărescu, A.L.; Radu, M.; Siloşi, C.A.; Popescu-Drigă, M.V.; Poenariu, I.S.; Siloşi, I.; Boldeanu, M.V.; Novac, M.B.; Novac, L.V. The role of mediating factors involved in angiogenesis during implantation. Rom. J. Morphol. Embryol. 2020, 61, 665–672.
- Singer, A.J.; Clark, R.A. Cutaneous Wound Healing. N. Engl. J. Med. 1999, 341, 738–746.
- Pandya, N.M.; Dhalla, N.S.; Santani, D.D. Angiogenesis—A new target for future therapy. Vascul. Pharmacol. 2006, 44, 265–274.
- Stephan, D.; Weltin, D.; Zaric, V.; Chapelon, D.; Da Silva, A.; Lugnier, C. Angiogenèse: De la physiologie à la thérapeutique. Réanim. Urgences 2000, 9, 534–544.
- Adamis, A.P.; Miller, J.W.; Bernal, M.T. Increased vascular endothelial growth factor levels in the vitreous of eyes with proliferative diabetic retinopathy. Am. J. Ophthalmol. 1994, 118, 445–450.





