Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Caterina Sagnelli | -- | 1882 | 2022-07-21 16:08:32 | | | |
| 2 | Vivi Li | Meta information modification | 1882 | 2022-07-22 05:12:06 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Iannuzzo, G.; Cuomo, G.; Lorenzo, A.D.; Tripaldella, M.; Mallardo, V.; Idelson, P.I.; Sagnelli, C.; Sica, A.; Creta, M.; Baltar, J.; et al. Dyslipidemia in Transplant Patients. Encyclopedia. Available online: https://encyclopedia.pub/entry/25402 (accessed on 07 February 2026).
Iannuzzo G, Cuomo G, Lorenzo AD, Tripaldella M, Mallardo V, Idelson PI, et al. Dyslipidemia in Transplant Patients. Encyclopedia. Available at: https://encyclopedia.pub/entry/25402. Accessed February 07, 2026.
Iannuzzo, Gabriella, Gianluigi Cuomo, Anna Di Lorenzo, Maria Tripaldella, Vania Mallardo, Paola Iaccarino Idelson, Caterina Sagnelli, Antonello Sica, Massimiliano Creta, Javier Baltar, et al. "Dyslipidemia in Transplant Patients" Encyclopedia, https://encyclopedia.pub/entry/25402 (accessed February 07, 2026).
Iannuzzo, G., Cuomo, G., Lorenzo, A.D., Tripaldella, M., Mallardo, V., Idelson, P.I., Sagnelli, C., Sica, A., Creta, M., Baltar, J., Crocetto, F., Bresciani, A., Gentile, M., Calogero, A., & Giallauria, F. (2022, July 21). Dyslipidemia in Transplant Patients. In Encyclopedia. https://encyclopedia.pub/entry/25402
Iannuzzo, Gabriella, et al. "Dyslipidemia in Transplant Patients." Encyclopedia. Web. 21 July, 2022.
Copy Citation
Cardiovascular disease is the most important cause of death worldwide in recent years; an increasing trend is also shown in organ transplant patients subjected to immunosuppressive therapies, in which cardiovascular diseases represent one of the most frequent causes of long-term mortality. This is also linked to immunosuppressant-induced dyslipidemia, which occurs in 27 to 71% of organ transplant recipients.
cardiovascular disease
dyslipidemia
immunosuppressive therapy
organ transplant
1. Introduction
Atherosclerosis is defined as the accumulation of fatty and fibrous material in the intima layer of an artery, inducing formation of atheroma (i.e., atherosclerotic plaque). Over time, plaque continues to grow, increasing its calcium and fibrous material content, and it can lead to tissue ischemia by obstructing the lumen of the vessel or disrupting itself by occluding the lumen of a distal vessel [1]. Depending on the affected artery, atherosclerotic cardiovascular disease (ASCVD) can cause acute coronary syndromes (ACS), ischemic stroke or transient cerebral ischemic attacks (TIA), and peripheral artery disease (PAD).
In 2019, there were an estimated 523 million cases of cardiovascular diseases (CVD), causing 18.5 million deaths [2]. Moreover, CVDs are a relevant cause of disability, bringing about 194 million and 143 million disability-adjusted life years (DALYs) for ischemic heart disease and stroke, respectively [2].
Dyslipidemia, that is, an alteration in lipid metabolism, is a well-known risk factor for ASCVD development; in particular, low-density lipoprotein cholesterol (LDL) circulating levels are unequivocally established as the principal determinant of atherosclerotic plaque formation and progression [3].
Atherosclerosis is a long process, beginning in the first decades of life, even in people without specific genetic characteristics, regardless of the presence of symptoms [4].
In addition to lipids, other risk factors have been identified in atherosclerosis, such as hyperglycemia, hypertension, tobacco use, and visceral adiposity [5][6][7][8].
Moreover, chronic kidney disease (CKD) is a well-known independent risk factor for atherosclerosis, and hemodialysis patients have a higher inflammatory status and more severe impaired blood flow [9].
All the above-mentioned factors contribute to plaque formation, triggering activation of inflammatory pathways, with consequent accumulation of fibrous material and plaque growth [1].
In patients who underwent solid organ transplantation and who were subjected to immunosuppressive therapies, dyslipidemia is very common; consequently, CVDs represent a frequent cause of long-term mortality in these patients, being estimated as the first cause of death in heart and kidney transplant recipients [10][11], and the second in liver transplant recipients [12].
Particularly in heart transplant recipients, atherosclerosis seems to be more aggressive, increasing the risk of vasculopathy progressively every 5 years, with an additional risk of 10% every 2 years after the transplant [13]. In addition, in these patients a particular form of coronary atherosclerosis was found, named cardiac allograft vasculopathy (CAV), which is morphologically different from typical atheromatous plaque [14].
Several risk factors are involved in the pathogenesis of the atherosclerotic process in these patients, such as transplant rejection, hypertension, dyslipidemia, and diabetes; however, hypercholesterolemia and hypertriglyceridemia are the most frequent metabolism abnormalities in clinical practice [15]. Immunosuppressor-mediated hyperlipidemia is characterized by an increase in LDL cholesterol, VLDL cholesterol, and/or an increase in total plasma triglycerides, mainly VLDL triglycerides [16][17].
2. Role of Dyslipidemia in Atherosclerosis
Dyslipidemia is defined as an abnormal concentration of lipids in the blood, and it can be present despite normal total cholesterol levels if there is an increase of lipoproteins that carry the cardiovascular risk factor.
Lipoproteins are constituted of lipids (such as cholesterol and triglycerides) and proteins called apolipoproteins. Different lipoproteins are distinguished by size, lipid content, and type of apolipoprotein.
Low-density lipoproteins (LDL) are small molecules, rich in ApoB-100 apolipoprotein, and are unequivocally correlated with ASCVD [3].
Very low-density lipoproteins (VLDL) and their remnants are rich in triglycerides and are also associated with ASCVD; however, this association seems to be related to the blood concentration of ApoB-containing particles rather than the concentration of triglycerides itself [18].
High-density lipoproteins (HDL) are the smallest lipoproteins and are abundant in apolipoprotein ApoA-I and ApoA-II; their function is to pick up cholesterol, which is internalized and carried to the liver or steroidogenic organs. Probably due to this role, HDL circulating levels are inversely associated with ASCVD [19], but there is no evidence that increasing these levels could reduce cardiovascular risk [20].
Lipoprotein(a) (Lp(a)) is similar to LDL but contains apolipoprotein Apo(a) in addition to ApoB. This particle, thanks to its small diameter, can pass through the endothelial barrier, provoking atherogenesis. Moreover, because they have a structure similar to plasminogen, pro-coagulant and pro-inflammatory effects have been shown [21].
The association between higher Lp(a) circulating concentrations and increased CVD risk has been assessed [22][23]; furthermore, a reduction in these levels in patients treated with proprotein convertase subtilisin/kexin 9 (PCSK9) inhibitors was shown to reduce CV risk [24][25].
Atherosclerosis is a long-lasting process, but dyslipidemia has been shown to play a key role at different stages.
In the initiation phase, the LDL particles, with a high cholesterol content, accumulate in the innermost layer (intima) of the vessel [26]. Here, these particles undergo an oxidation reaction and are phagocytosed by macrophages, which are transformed into foam cells [26]. As result, a localized inflammatory reaction begins, with the consequent release of cytokines and expression of adhesion molecules, attracting other monocytes circulating in the blood, transforming them into macrophages which in turn become foam cells [26].
Since inflammation plays a pivotal role in the atherosclerotic process, C-reactive protein (CRP) has been chosen as a prognostic marker for cardiovascular risk [27]. Of note, type 1 T helper lymphocytes (producing cytokines such as IFN-γ and TNF) have been found in human atherosclerotic plaques as promotors of atherogenesis, while regulatory T cells seem to mitigate this process [28][29].
In physiological conditions, the arterial endothelium has intrinsic properties preventing thrombus formation; however, the alteration of endothelium function, which loses its permeability and nitric oxide (NO)-mediated vasorelaxation capacity [30][31], may contribute to thrombus formation. In addition, other factors, such as flow alterations, may influence atherosclerosis initiation; indeed, plaques tend to form at flow disturbance sites, such as at the branching of vessels [32].
During plaque enlargement, due to high lipid levels, calcification of plaque may occur [33]; if calcification is very extended, plaque disruption and consequent thromboembolic events will be less probable [34].
Finally, plaque evolution and consequent complications depend on fibrous cap thickness and lipid core quantity. A thin fibrous cap determines more vulnerability and probable rupture [35]; when rupture of an atherosclerotic plaque occurs, the consequent exposure of thrombogenic material that is in the core (such as tissue factor) and circulating (thrombin) triggers formation of a thrombus [35].
Otherwise, when plaque has lower inflammatory cells and lipid content, greater collagen matrix content and thicker fibrous cap, a different complication called “plaque erosion” may occur, leading to formation of platelet-rich “white” clots.
The complication discussed so far typically occurs in coronary arteries, causing myocardial infarction [36]. In other vessels, atherosclerotic plaque growth may continue uninterrupted until the formation of flow-limiting lesions, causing PAD.
In addition to dyslipidemia, other risk factors contribute to the atherosclerotic process. Arterial hypertension causes endothelial dysfunction through shear stress [32], and in addition it increases levels of angiotensin II, which activates the prescription of nuclear factor-κB (NF-κB), responsible for inflammatory pathways [37].
Type 2 diabetes mellitus causes insulin resistance and accumulation of visceral adipose tissue, which contains inflammatory cells and increases circulating pro-inflammatory cytokines levels [5].
In conclusion, several factors are demonstrated favoring plaque formation, but dyslipidemia is certainly the main atherogenesis promoter, on which an intervention is desirable.
3. Dyslipidemia and Atherosclerosis in Transplant Recipients
In recent years, advances made in the field of solid organ transplants, as regards surgical techniques, infection prevention, and immunosuppressive therapy, have resulted in increasing survival of transplant recipients. Consequently, recent data have shown an increasing prevalence of CVD, which has become the leading cause of death following kidney [10] and heart transplant [11], and the second leading cause after liver transplant [12][38][39]. It should be considered that kidney transplantation can be a confounding factor, as it is often the final stage of long-lasting CKD, which is itself an important cardiovascular risk factor [40], although this had been underestimated by cardiovascular risk prediction models such as the Framingham Risk Score [41][42]. The latest European Society of Cardiology (ESC) guidelines on cardiovascular disease prevention have defined patients with moderate CKD as high risk for CVD, and those with severe CKD at very high risk [43].
For other solid organ transplant recipients, among causes of this increase in CVD, it should be considered that dyslipidemia occurs frequently in these patients.
The pathophysiological mechanisms through which an increase in circulating LDL levels favors atherosclerosis and consequently ASCVD have been presented in the previous chapter.
Prevalence of hyperlipidemia was estimated at 80% in kidney transplant recipients [44], 50% in heart transplant recipients [45], and about 70% in liver transplant recipients [15], compared to about 35% in the general population [46][47][48][49][50].
Multiple factors contribute to lipid alterations, such as genetic predisposition [44][45][46], dietary habits [51], and age; however, the main effect is due to immunosuppressants, which have shown intrinsic pharmacodynamic properties to cause dyslipidemia and hyperglycemia [52][53]. In line with these findings, serum total cholesterol concentration is higher in the first 3–6 months after transplantation, when immunosuppressants are administered at higher doses [54].
These drugs are responsible not only for the increase in LDL and triglycerides but are also associated with other atherosclerosis promoter factors. Arterial hypertension is a common side effect of immunosuppressants such as cyclosporine [55] and tacrolimus [56] and has been found in approximately 80% of transplant recipients [57]; corticosteroids, the oldest and most used immunosuppressants, have a well-known ability to cause hyperglycemia and diabetes [58], and this effect has been shown to be enhanced by cyclosporine and tacrolimus [59].
Furthermore, dyslipidemia can cause other complications, in addition to CVD, in solid organ transplant recipients. In kidney transplant recipients there is a higher concentration of oxidized LDL (oxLDL) particles [60], possibly due to increased inflammatory state [61] or higher concentration of pro-inflammatory triglycerides [62].
These higher oxLDL, levels, together with the proven lower HDL concentration, are associated with chronic allograft nephropathy (CAN) [63], which is the main cause of kidney transplant failure [64][65].
Finally, among the factors promoting atheroma formation and growth, a protracted activation of inflammation in transplant recipients has been demonstrated [66][67]. A particular consequence of inflammation, the cardiac allograft vasculopathy (CAV), has been observed after heart transplantation [68].
CAV is a particular form of coronary disease, which is responsible for about 10% of deaths after heart transplant [68]; it is distinguished from normal coronary atherosclerosis because these lesions, which appear as concentric intimal hyperplasia obliterating the lumen of the vessel, affect the intramuscular arteries and the microvascular bed [69].
The pathogenesis is mainly due to the formation of antibodies against donor antigens, which trigger an inflammatory response mediated by T lymphocytes directed against donor endothelial cells, which consequently proliferate and occlude the vessel lumen [70][71]. However, in addition to inflammation, other metabolic factors, including dyslipidemia, are also promoters of CAV [71].
Mechanisms of atherosclerosis in transplant patients are illustrated in Figure 1.
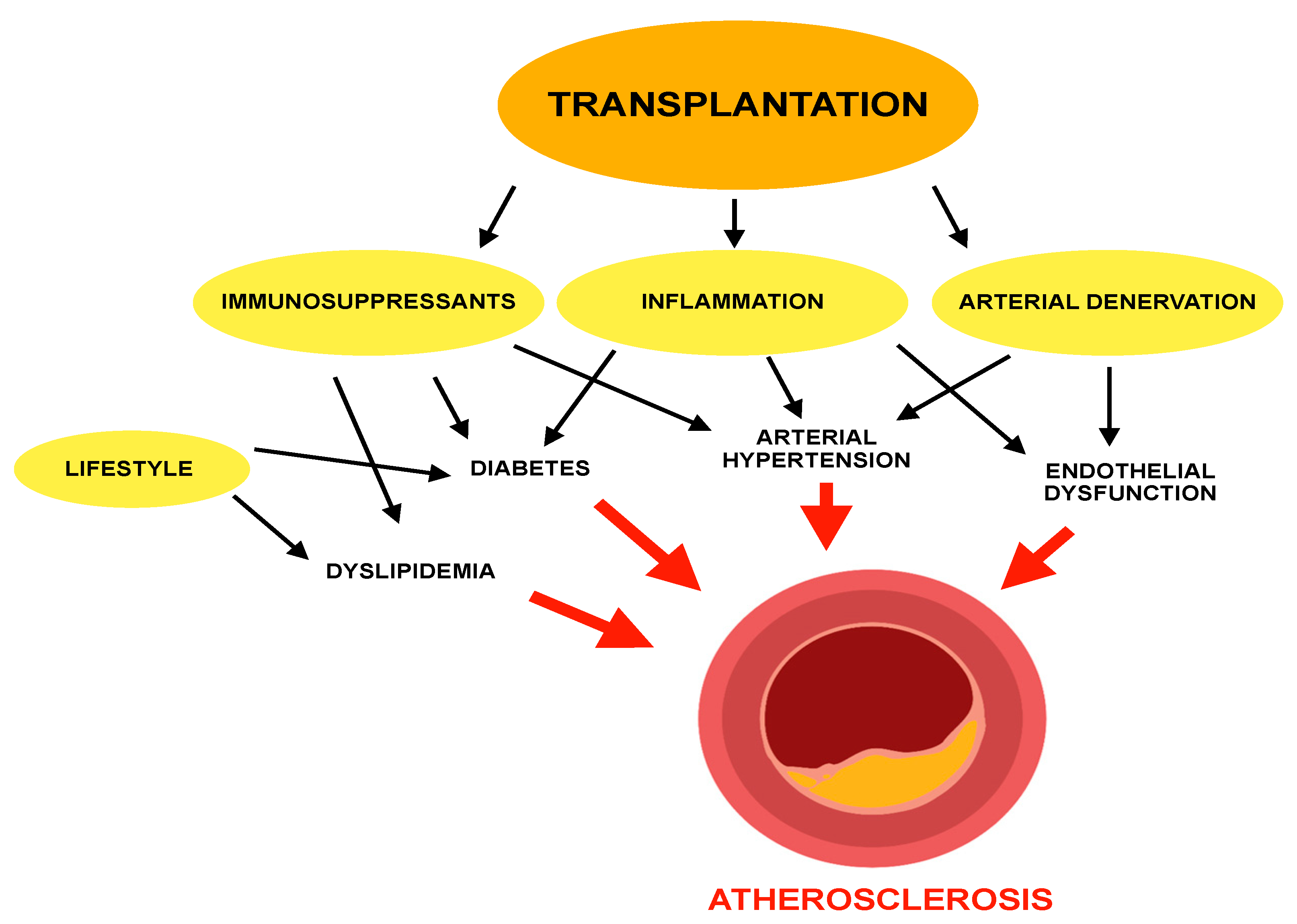
Figure 1. Mechanisms of atherosclerosis in transplant patients.
In addition to the effects on cardiovascular risk, increased circulating lipid levels can cause other diseases; in fact, it has been shown that when they are in excessive levels, lipids can also accumulate in non-adipose tissue and cause lipotoxicity, which mainly affects cardiac, skeletal muscle, and kidney tissues [72]. Furthermore, it must be emphasized that lipids have a strong pro-inflammatory effect, being able to enhance the release of molecules such as adipokines [73].
Therefore, atherogenesis and consequently ASCVD in transplant recipients can be considered the consequence on the one hand of the inflammatory state due to immune response against donor cells and on the other hand of the drugs administered to reduce this inflammatory response and transplant rejection.
References
- Libby, P.; Buring, J.E.; Badimon, L.; Hansson, G.K.; Deanfield, J.; Bittencourt, M.S.; Tokgözoğlu, L.; Lewis, E.F. Atherosclerosis. Nat. Rev. Dis. Primers 2019, 5, 56.
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update from the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021.
- Ference, B.A.; Ginsberg, H.N.; Graham, I.; Ray, K.K.; Packard, C.J.; Bruckert, E.; Hegele, R.A.; Krauss, R.M.; Raal, F.J.; Schunkert, H.; et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 2017, 38, 2459–2472.
- Fernández-Friera, L.; Peñalvo, J.L.; Fernández-Ortiz, A.; Ibañez, B.; López-Melgar, B.; Laclaustra, M.; Oliva, B.; Mocoroa, A.; Mendiguren, J.; Martínez de Vega, V.; et al. Prevalence, Vascular Distribution, and Multiterritorial Extent of Subclinical Atherosclerosis in a Middle-Aged Cohort: The PESA (Progression of Early Subclinical Atherosclerosis) Study. Circulation 2015, 131, 2104–2113.
- Rocha, V.Z.; Libby, P. Obesity, inflammation, and atherosclerosis. Nat. Rev. Cardiol. 2009, 6, 399–409.
- Després, J.P. Body fat distribution and risk of cardiovascular disease: An update. Circulation 2012, 126, 1301–1313.
- Messner, B.; Bernhard, D. Smoking and cardiovascular disease: Mechanisms of endothelial dysfunction and early atherogenesis. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 509–515.
- Poznyak, A.; Grechko, A.V.; Poggio, P.; Myasoedova, V.A.; Alfieri, V.; Orekhov, A.N. The Diabetes Mellitus-Atherosclerosis Connection: The Role of Lipid and Glucose Metabolism and Chronic Inflammation. Int. J. Mol. Sci. 2020, 21, E1835.
- Recio-Mayoral, A.; Banerjee, D.; Streather, C.; Kaski, J.C. Endothelial dysfunction, inflammation and atherosclerosis in chronic kidney disease—A cross-sectional study of predialysis, dialysis and kidney-transplantation patients. Atherosclerosis 2011, 216, 446–451.
- Israni, A.K.; Snyder, J.J.; Skeans, M.A.; Peng, Y.; Maclean, J.R.; Weinhandl, E.D.; Kasiske, B.L.; PORT Investigators. Predicting coronary heart disease after kidney transplantation: Patient Outcomes in Renal Transplantation (PORT) Study. Am. J. Transplant. 2010, 10, 338–353.
- Kobashigawa, J.A.; Starling, R.C.; Mehra, M.R.; Kormos, R.L.; Bhat, G.; Barr, M.L.; Sigouin, C.S.; Kolesar, J.; Fitzsimmons, W. Multicenter retrospective analysis of cardiovascular risk factors affecting long-term outcome of de novo cardiac transplant recipients. J. Heart Lung Transplant. 2006, 25, 1063–1069.
- Albeldawi, M.; Aggarwal, A.; Madhwal, S.; Cywinski, J.; Lopez, R.; Eghtesad, B.; Zein, N.N. Cumulative risk of cardiovascular events after orthotopic liver transplantation. Liver Transpl. 2012, 18, 370–375.
- Warden, B.A.; Duell, P.B. Management of dyslipidemia in adult solid organ transplant recipients. J. Clin. Lipidol. 2019, 13, 231–245.
- Patel, C.B.; Holley, C.L. Cardiac Allograft Vasculopathy: A Formidable Foe. J. Am. Coll. Cardiol. 2019, 74, 52–53.
- Hüsing, A.; Kabar, I.; Schmidt, H.H. Lipids in liver transplant recipients. World J. Gastroenterol. 2016, 22, 3315–3324.
- Kockx, M.; Kritharides, L. Hyperlipidaemia in immunosuppression. Curr. Opin. Lipidol. 2016, 27, 631–632.
- Rodríguez, F.O.R.; Santiago, J.C.; Jiménez, G.M.; Carreño Rodríguez, Y.R.; Meléndez, A.R.; Medina Uicab, C.J.; Salas, L.N.; Quiñones Gamero, M.A.; Ramírez, C.D.R.G.; Covarrubias, L.G.; et al. Post-Transplant Cholesterol and Triglyceride Behavior: Effects of Sex, Age of the Recipient, and Type of Donor. Transplant. Proc. 2020, 52, 1157–1162.
- Ference, B.A.; Kastelein, J.J.P.; Ray, K.K.; Ginsberg, H.N.; Chapman, M.J.; Packard, C.J.; Laufs, U.; Oliver-Williams, C.; Wood, A.M.; Butterworth, A.S.; et al. Association of Triglyceride-Lowering LPL Variants and LDL-C-Lowering LDLR Variants with Risk of Coronary Heart Disease. JAMA 2019, 321, 364–373.
- Ajala, O.N.; Demler, O.V.; Liu, Y.; Farukhi, Z.; Adelman, S.J.; Collins, H.L.; Ridker, P.M.; Rader, D.J.; Glynn, R.J.; Mora, S. Anti-Inflammatory HDL Function, Incident Cardiovascular Events, and Mortality: A Secondary Analysis of the JUPITER Randomized Clinical Trial. J. Am. Heart Assoc. 2020, 9, e016507.
- AIM-HIGH Investigators; Boden, W.E.; Probstfield, J.L.; Anderson, T.; Chaitman, B.R.; Desvignes-Nickens, P.; Koprowicz, K.; McBride, R.; Teo, K.; Weintraub, W. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N. Engl. J. Med. 2011, 365, 2255–2267.
- Van der Valk, F.M.; Bekkering, S.; Kroon, J.; Yeang, C.; Van den Bossche, J.; van Buul, J.D.; Ravandi, A.; Nederveen, A.J.; Verberne, H.J.; Scipione, C.; et al. Oxidized Phospholipids on Lipoprotein(a) Elicit Arterial Wall Inflammation and an Inflammatory Monocyte Response in Humans. Circulation 2016, 134, 611–624.
- Gentile, M.; Simeon, V.; Iannuzzo, G.; Mattiello, A.; Donata di Taranto, M.; Panico, S.; Rubba, P. Lipoprotein (a) is an independent predictor of cardiovascular events in Mediterranean women (Progetto Atena). Eur. J. Prev. Cardiol. 2020, 27, 2248–2250.
- Nordestgaard, B.G.; Chapman, M.J.; Ray, K.; Borén, J.; Andreotti, F.; Watts, G.F.; Ginsberg, H.; Amarenco, P.; Catapano, A.; Descamps, O.S.; et al. Lipoprotein(a) as a cardiovascular risk factor: Current status. Eur. Heart J. 2010, 31, 2844–2853.
- O’Donoghue, M.L.; Fazio, S.; Giugliano, R.P.; Stroes, E.S.G.; Kanevsky, E.; Gouni-Berthold, I.; Im, K.; Lira Pineda, A.; Wasserman, S.M.; Češka, R.; et al. Lipoprotein(a), PCSK9 Inhibition, and Cardiovascular Risk. Circulation 2019, 139, 1483–1492.
- Iannuzzo, G.; Gentile, M.; Bresciani, A.; Mallardo, V.; Di Lorenzo, A.; Merone, P.; Cuomo, G.; Pacileo, M.; Sarullo, F.M.; Venturini, E.; et al. Inhibitors of Protein Convertase Subtilisin/Kexin 9 (PCSK9) and Acute Coronary Syndrome (ACS): The State-of-the-Art. J. Clin. Med. 2021, 10, 1510.
- Navab, M.; Ananthramaiah, G.M.; Reddy, S.T.; Van Lenten, B.J.; Ansell, B.J.; Fonarow, G.C.; Vahabzadeh, K.; Hama, S.; Hough, G.; Kamranpour, N.; et al. The oxidation hypothesis of atherogenesis: The role of oxidized phospholipids and HDL. J. Lipid Res. 2004, 45, 993–1007.
- Ridker, P.M. A Test in Context: High-Sensitivity C-Reactive Protein. J. Am. Coll. Cardiol. 2016, 67, 712–723.
- Libby, P.; Lichtman, A.H.; Hansson, G.K. Immune effector mechanisms implicated in atherosclerosis: From mice to humans. Immunity 2013, 38, 1092–1104.
- Nus, M.; Mallat, Z. Immune-mediated mechanisms of atherosclerosis and implications for the clinic. Expert Rev. Clin. Immunol. 2016, 12, 1217–1237.
- Gimbrone, M.A.; García-Cardeña, G. Endothelial Cell Dysfunction and the Pathobiology of Atherosclerosis. Circ. Res. 2016, 118, 620–636.
- Di Minno, A.; Gentile, M.; Iannuzzo, G.; Calcaterra, I.; Tripaldella, M.; Porro, B.; Cavalca, V.; Di Taranto, M.D.; Tremoli, E.; Fortunato, G.; et al. Endothelial function improvement in patients with familial hypercholesterolemia receiving PCSK-9 inhibitors on top of maximally tolerated lipid lowering therapy. Thromb. Res. 2020, 194, 229–236.
- Chatzizisis, Y.S.; Coskun, A.U.; Jonas, M.; Edelman, E.R.; Feldman, C.L.; Stone, P.H. Role of endothelial shear stress in the natural history of coronary atherosclerosis and vascular remodeling: Molecular, cellular, and vascular behavior. J. Am. Coll. Cardiol. 2007, 49, 2379–2393.
- Ruiz, J.L.; Hutcheson, J.D.; Aikawa, E. Cardiovascular calcification: Current controversies and novel concepts. Cardiovasc. Pathol. 2015, 24, 207–212.
- Huang, H.; Virmani, R.; Younis, H.; Burke, A.P.; Kamm, R.D.; Lee, R.T. The impact of calcification on the biomechanical stability of atherosclerotic plaques. Circulation 2001, 103, 1051–1056.
- Bentzon, J.F.; Otsuka, F.; Virmani, R.; Falk, E. Mechanisms of plaque formation and rupture. Circ. Res. 2014, 114, 1852–1866.
- Libby, P. Mechanisms of acute coronary syndromes and their implications for therapy. N. Engl. J. Med. 2013, 368, 2004–2013.
- Kranzhöfer, R.; Browatzki, M.; Schmidt, J.; Kübler, W. Angiotensin II activates the proinflammatory transcription factor nuclear factor-kappaB in human monocytes. Biochem. Biophys. Res. Commun. 1999, 257, 826–828.
- Tsai, H.I.; Liu, F.C.; Lee, C.W.; Kuo, C.F.; See, L.C.; Chung, T.T.; Yu, H.P. Cardiovascular disease risk in patients receiving organ transplantation: A national cohort study. Transpl. Int. 2017, 30, 1161–1171.
- Bostom, A.D.; Brown, R.S.; Chavers, B.M.; Coffman, T.M.; Cosio, F.G.; Culver, K.; Curtis, J.J.; Danovitch, G.M.; Everson, G.T.; First, M.R.; et al. Prevention of post-transplant cardiovascular disease—Report and recommendations of an ad hoc group. Am. J. Transplant. 2002, 2, 491–500.
- Gansevoort, R.T.; Correa-Rotter, R.; Hemmelgarn, B.R.; Jafar, T.H.; Heerspink, H.J.; Mann, J.F.; Matsushita, K.; Wen, C.P. Chronic kidney disease and cardiovascular risk: Epidemiology, mechanisms, and prevention. Lancet 2013, 382, 339–352.
- Weiner, D.E.; Tighiouart, H.; Elsayed, E.F.; Griffith, J.L.; Salem, D.N.; Levey, A.S.; Sarnak, M.J. The Framingham predictive instrument in chronic kidney disease. J. Am. Coll. Cardiol. 2007, 50, 217–224.
- Mansell, H.; Stewart, S.A.; Shoker, A. Validity of cardiovascular risk prediction models in kidney transplant recipients. Sci. World J. 2014, 2014, 750579.
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337.
- Markell, M.S.; Armenti, V.; Danovitch, G.; Sumrani, N. Hyperlipidemia and glucose intolerance in the post-renal transplant patient. J. Am. Soc. Nephrol. 1994, 4, S37–S47.
- Becker, D.M.; Markakis, M.; Sension, M.; Vitalis, S.; Baughman, K.; Swank, R.; Kwiterovich, P.O.; Pearson, T.A.; Achuff, S.; Baumgartner, W.A.; et al. Prevalence of hyperlipidemia in heart transplant recipients. Transplantation 1987, 44, 323–325.
- Pan, L.; Yang, Z.; Wu, Y.; Yin, R.X.; Liao, Y.; Wang, J.; Gao, B.; Zhang, L.; China National Survey of Chronic Kidney Disease Working Group. The prevalence, awareness, treatment and control of dyslipidemia among adults in China. Atherosclerosis 2016, 248, 2–9.
- Tóth, P.P.; Potter, D.; Ming, E.E. Prevalence of lipid abnormalities in the United States: The National Health and Nutrition Examination Survey 2003–2006. J. Clin. Lipidol. 2012, 6, 325–330.
- González-Amieva, A.; López-Miranda, J.; Marín, C.; Pérez-Martinez, P.; Gómez, P.; Paz-Rojas, E.; Arizón, J.M.; Jiménez-Perepérez, J.A.; Concha, M.; Pérez-Jiménez, F. The apo A-I gene promoter region polymorphism determines the severity of hyperlipidemia after heart transplantation. Clin. Transplant. 2003, 17, 56–62.
- Taegtmeyer, A.B.; Breen, J.B.; Smith, J.; Rogers, P.; Kullak-Ublick, G.A.; Yacoub, M.H.; Banner, N.R.; Barton, P.J. Effect of ABCB1 genotype on pre- and post-cardiac transplantation plasma lipid concentrations. J. Cardiovasc. Transl. Res. 2011, 4, 304–312.
- Numakura, K.; Kagaya, H.; Yamamoto, R.; Komine, N.; Saito, M.; Hiroshi, T.; Akihama, S.; Inoue, T.; Narita, S.; Tsuchiya, N.; et al. Characterization of clinical and genetic risk factors associated with dyslipidemia after kidney transplantation. Dis. Markers 2015, 2015, 179434.
- Pinto, A.S.; Chedid, M.F.; Guerra, L.T.; Cabeleira, D.D.; Kruel, C.D.P. Dietary management for dyslipidemia in liver transplant recipients. Arq. Bras. Cir. Dig. 2016, 29, 246–251.
- Miller, L.W. Cardiovascular toxicities of immunosuppressive agents. Am. J. Transplant. 2002, 2, 807–818.
- Claes, K.; Meier-Kriesche, H.U.; Schold, J.D.; Vanrenterghem, Y.; Halloran, P.F.; Ekberg, H. Effect of different immunosuppressive regimens on the evolution of distinct metabolic parameters: Evidence from the Symphony study. Nephrol. Dial. Transplant. 2012, 27, 850–857.
- Miller, L.W.; Schlant, R.C.; Kobashigawa, J.; Kubo, S.; Renlund, D.G. 24th Bethesda conference: Cardiac transplantation. Task Force 5: Complications. J. Am. Coll. Cardiol. 1993, 22, 41–54.
- Sander, M.; Lyson, T.; Thomas, G.D.; Victor, R.G. Sympathetic neural mechanisms of cyclosporine-induced hypertension. Am. J. Hypertens. 1996, 9, 121S–138S.
- Wang, J.; Guo, R.; Liu, S.; Chen, Q.; Zuo, S.; Yang, M.; Zuo, X. Molecular mechanisms of FK506-induced hypertension in solid organ transplantation patients. Chin. Med. J. 2014, 127, 3645–3650.
- Singer, D.R.; Jenkins, G.H. Hypertension in transplant recipients. J. Hum. Hypertens. 1996, 10, 395–402.
- Arner, P.; Gunnarsson, R.; Blomdahl, S.; Groth, C.G. Some characteristics of steroid diabetes: A study in renal-transplant recipients receiving high-dose corticosteroid therapy. Diabetes Care 1983, 6, 23–25.
- Drachenberg, C.B.; Klassen, D.K.; Weir, M.R.; Wiland, A.; Fink, J.C.; Bartlett, S.T.; Cangro, C.B.; Blahut, S.; Papadimitriou, J.C. Islet cell damage associated with tacrolimus and cyclosporine: Morphological features in pancreas allograft biopsies and clinical correlation. Transplantation 1999, 68, 396–402.
- Ghanem, H.; van den Dorpel, M.A.; Weimar, W.; Man in ’T Veld, A.J.; El-Kannishy, M.H.; Jansen, H. Increased low density lipoprotein oxidation in stable kidney transplant recipients. Kidney Int. 1996, 49, 488–493.
- Taylor, J.E.; Scott, N.; Hill, A.; Bridges, A.; Henderson, I.S.; Stewart, W.K.; Belch, J.J. Oxygen free radicals and platelet and granulocyte aggregability in renal transplant patients. Transplantation 1993, 55, 500–504.
- Sutherland, W.H.; Walker, R.J.; Ball, M.J.; Stapley, S.A.; Robertson, M.C. Oxidation of low density lipoproteins from patients with renal failure or renal transplants. Kidney Int. 1995, 48, 227–236.
- Bosmans, J.L.; Holvoet, P.; Dauwe, S.E.; Ysebaert, D.K.; Chapelle, T.; Jürgens, A.; Kovacic, V.; Van Marck, E.A.; De Broe, M.E.; Verpooten, G.A. Oxidative modification of low-density lipoproteins and the outcome of renal allografts at 1 1/2 years. Kidney Int. 2001, 59, 2346–2356.
- Yates, P.J.; Nicholson, M.L. The aetiology and pathogenesis of chronic allograft nephropathy. Transpl. Immunol. 2006, 16, 148–157.
- Najafian, B.; Kasiske, B.L. Chronic allograft nephropathy. Curr. Opin. Nephrol. Hypertens. 2008, 17, 149–155.
- Ruiz, M.C.; Medina, A.; Moreno, J.M.; Gómez, I.; Ruiz, N.; Bueno, P.; Asensio, C.; Osuna, A. Relationship between oxidative stress parameters and atherosclerotic signs in the carotid artery of stable renal transplant patients. Transplant. Proc. 2005, 37, 3796–3798.
- Urbanowicz, T.K.; Michalak, M.; Gąsecka, A.; Olasińska-Wiśniewska, A.; Perek, B.; Rodzki, M.; Bociański, M.; Jemielity, M. A Risk Score for Predicting Long-Term Mortality Following Off-Pump Coronary Artery Bypass Grafting. J. Clin. Med. 2021, 10, 3032.
- Khush, K.K.; Cherikh, W.S.; Chambers, D.C.; Goldfarb, S.; Hayes, D., Jr.; Kucheryavaya, A.Y.; Levvey, B.J.; Meiser, B.; Rossano, J.W.; Stehlik, J.; et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-fifth Adult Heart Transplantation Report-2018, Focus Theme: Multiorgan Transplantation. J. Heart Lung Transplant. 2018, 37, 1155–1168.
- Lu, W.H.; Palatnik, K.; Fishbein, G.A.; Lai, C.; Levi, D.S.; Perens, G.; Alejos, J.; Kobashigawa, J.; Fishbein, M.C. Diverse morphologic manifestations of cardiac allograft vasculopathy: A pathologic study of 64 allograft hearts. J. Heart Lung Transplant. 2011, 30, 1044–1050.
- Schmauss, D.; Weis, M. Cardiac allograft vasculopathy: Recent developments. Circulation 2008, 117, 2131–2141.
- Lee, F.; Nair, V.; Chih, S. Cardiac allograft vasculopathy: Insights on pathogenesis and therapy. Clin. Transplant. 2020, 34, e13794.
- Nishi, H.; Higashihara, T.; Inagi, R. Lipotoxicity in Kidney, Heart, and Skeletal Muscle Dysfunction. Nutrients 2019, 11, 1664.
- Mancuso, P. The role of adipokines in chronic inflammation. Immunotargets Ther. 2016, 5, 47–56.
More
Information
Subjects:
Medicine, General & Internal
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
678
Revisions:
2 times
(View History)
Update Date:
22 Jul 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




