1. Radiography
Conventional radiography remains an important diagnostic and monitoring tool for arthritis treatment. Currently, radiography is the reference research method, with a reasonable level of reproducibility
[1]. Modern radiography is an inexpensive and readily available method that allows for a wide coverage of affected areas. In addition, there are validated assessment methods and scoring systems that provide longitudinal comparisons in Juvenile idiopathic arthritis (JIA)
[2].
The main disadvantage of radiography in pediatric patients is the use of ionizing radiation. In addition, the method is not sufficiently sensitive for detecting early osteochondral changes and assessing the inflammatory process, as it allows for only bone structure assessment, while the pathological process begins in the synovial membrane. The destruction of the epiphyseal cartilage leads to persistent inflammation and hypertrophy of the synovial membrane. Only erosive changes after a significant loss of cartilage become evident on radiographs
[3]. Therefore, the value of this method is undeniable in the diagnosis of rheumatoid arthritis (RA) in the presence of erosion.
Radiographs are rarely useful in the diagnosis of JIA because, in the early stages, they are often normal, and the growth of bone tissue may occur earlier with the disease
[4][5]. For example, on radiographs, the presence of growth lines or transverse lines migrating from the growth plate may indicate underlying chronic inflammation. Although they are not specific to inflammation, they can manifest as malnutrition, endocrinopathies, or fractures. In the early stages of the disease, the narrowing of the joint spaces can be observed in 5% of patients, erosion in 10%, and accelerated bone growth in 20% (more often with damage to the knee joint)
[6]. Radiographs can also reveal a disease pattern that suggests a rare alternative diagnosis, such as congenital chondrocalcinosis (pyrophosphate arthropathy). At the same time, a competent assessment of the X-ray images of bones and joints in children—considering age and, in many cases, sex characteristics—will help reduce the number of “errors in the work of a rheumatologist”
[1]. Thus, radiography plays an important but limited role in the early diagnosis of RA.
2. Ultrasound
Ultrasound plays an important role in pediatric rheumatology and is one of the most commonly used techniques. This method is cost-effective, readily available, and non-radiating. It allows for the outlining of inflammatory and structural changes in arthritis, aids in the narrowing of the differential diagnosis, and helps to determine the activity of the disease, identify subclinical diseases, monitor treatment, and assess the severity of joint damage.
The criteria for evaluating ultrasound data are as follows: the amount of intra-articular effusion, the thickness of the synovial membrane, and articular hyaline cartilage. The most common ultrasound result in arthritis is the establishment of inflammatory lesions of the peripheral joints, articular cavity (synovitis), and tendon sheaths (tenosynovitis), along with the detection of bursitis, enthesopathy, and erosions
[7].
For example, after arthroplasty, an ultrasound is used to diagnose and monitor postoperative complications, which include the abnormal accumulation of fluid in the area of the endoprosthesis, hematomas at various stages of resorption and organization, abscesses, tendon damage, and neuropathies, such as peroneal nerve palsy after knee joint and sciatic nerve injury during hip arthroplasty
[8]. However, the visual image in this method significantly depends on the anatomical and physiological characteristics of a particular patient, which can present difficulties in childhood, considering the characteristics of a growing organism
[9]. For example, for juvenile groups, there are no norms/pathological metric criteria for the thickness of the synovial membrane and cartilage. An ultrasound examination is significantly inferior in identifying central erosive changes located in the center of large joints. It cannot penetrate the bone because of the acoustic shadow from the overlying bone (some areas are inaccessible) and the low penetration of the ultrasound beam into the central part of the connection with high-frequency transducers. The limitations of this method include the inability to investigate changes in the bone marrow associated with the active phase of the course
[10].
In young children, for whom synovial tissue is difficult to distinguish from the adjacent hypoechoic epiphyseal cartilage, the assessment of the synovium is challenging. In patients with an advanced stage of the disease, the thickening of the synovial membrane and its vascularization may reflect very little restructuring activity against the background of long-term inflammation
[9]. The Doppler ultrasound analyzes synovial blood flow and can show the activity of the process; however, the physiologically profuse vascularization of the epiphyseal cartilage must be distinguished from the synovial hypervascularization associated with inflammation. A potential trap for error in the ultrasound study may be the physiologically pronounced vascularization of the synovial membrane and enthesis in healthy children due to the differentiation of the bone and joint system and the abundant blood supply to the emerging tissues
[5].
According to Sudoł-Szopińska et al.
[11], the disadvantages of ultrasound include the following: low specificity in the ability to assess the state of the bone marrow, since several arthropathies exhibit the same spectrum of symptoms; a limited field of vision; a significant dependence on the expert’s experience and the quality of the equipment; and the need for special training.
To conduct a high-quality ultrasound scan, the doctor must be familiar with the changes occurring in a healthy developing joint; the change in the thickness of the epiphyseal cartilage should be compared with that in a healthy child of the same sex and age. According to Cherkasova
[12], ultrasound is important for the onset of the disease because it allows for the determination of the expansion of the joint spaces (effusion), the uneven thickening and edema of the synovial membrane, the hyper vascularization of the synovial membrane, intra-articular effusion, the erosion of the contours of the cortical layer of bones, the uneven thickness and heterogeneity of the hyaline cartilage structure, and the infiltration of soft tissues of varying severity.
Given the low level of correlation between clinical data and ultrasound indicators, it is necessary to conduct randomized controlled trials to evaluate not only the therapy received but also new imaging technologies. In the case of remission in a significant number of cases, the residual disease cannot be differentiated from chronic arthritis. The criteria for remission in ultrasound examination, in both adults and children with JIA, have not yet been established
[11]. Another disadvantage of ultrasound is that it does not provide any information about the structure of the intramedullary bone. It is known that edematous bone marrow lesions detected on MRI are important prognostic factors and are considered biomarkers of disease progression.
3. MRI
Owing to its indisputable sensitivity in visualizing early signs of soft tissue inflammation and bone changes, MRI has several advantages: the absence of ionizing radiation, multiplanarity, and the excellent contrast resolution of soft tissues, which makes it possible to evaluate all joint structures. This is the only method that can objectify the bone marrow. This is an indication for treatment to avoid irreversible joint destruction. However, long-term studies are needed to distinguish the bone marrow edema seen in healthy children from the bone marrow edema that develops before erosions in patients with JIA
[5]. The clinical significance of bone marrow edema in children with JIA remains unclear, and, owing to its high prevalence in healthy children, it can be considered a sign of normal bone maturation.
It is difficult to differentiate between synovial tissue and intra-articular fluid on MRI. However, the “inflamed” synovium, in contrast to intra-articular fluid, is enhanced by the intravenous administration of paramagnetic Gd-containing contrast agents, which facilitates its recognition
[13]. It is known that, on MRI, synovial thickening (≥2 mm) that increases after contrast administration is considered an indicator of ongoing inflammation (synovitis), as it has been shown to be treatable. In addition, as reported by Hemke et al. in 2017
[14], the thickness of the synovial membrane in the knee joints of healthy children does not exceed 1.8 mm. When clinical evaluation shows no signs of inflammation but synovial thickening is observed on MRI, it is usually interpreted as subclinical synovitis. It has previously been reported that synovial thickening on MRI is present in approximately 50% of JIA patients who are considered clinically inactive. However, another explanation for the synovial thickening observed on MRI is the persistent synovial changes following chronic inflammation. Because of this controversy, the clinical significance of synovial thickening on MRI remains unclear
[15]. According to the results of studies by van Gulik, MRI in younger patients with JIA may be a more effective additional method for monitoring disease activity. A significant proportion of children with clinically inactive JIA showed synovial thickening on MRI (34.6%). These results are consistent with previous studies on patients with JIA that examined the inconsistency between the clinical assessment and MRI findings
[16][17].
As there are currently no long-term studies evaluating synovial thickening on MRI in patients with clinically inactive JIA, it remains difficult to determine the causes of the observed synovial thickening on MRI.
In recent years, MRI has become increasingly used in JIA, despite some limitations in its application. During one routine MRI examination, only one joint can be examined with all the required sequential contrast enhancements. However, this increases the likelihood of allergic reactions and stressful conditions among children.
There are also relative contraindications for MRI, such as claustrophobia and embedded metal fragments
[13]. MRI also has a high cost, a limited availability, a lack of standardized longitudinal prevalence and prospective studies, and, importantly, the need for sedation in young children (4–6 years of age) for proper examination.
At the same time, indications for MRI have changed, shifting towards the early detection of JIA. There has been an overall increase in the clinical demand for high-quality imaging. If multiple joints are affected, MRI of all the affected joints should be performed. However, these studies are time-consuming and expensive. Children need to lie still during the study, which is not always feasible for them; therefore, an alternative study is proposed. Currently, MRI of the whole body is widely used according to the protocol. Whole-body MRI is a diagnostic technique that allows for images of the entire body to be obtained in a single scan. There is no standard protocol for examining full-body MRIs in patients with JIA. Various pulse sequences are used for this purpose. The examination can be performed in the sagittal, coronal, and axial planes with or without contrast. Whole-body MRI can play an important role in assessing both active and asymptomatic joints for effusion, especially in areas that are not readily accessible to clinical methods (temporomandibular joint and sacroiliac joint)
[5][18].
4. Passive Microwave Radiometry (MWR)
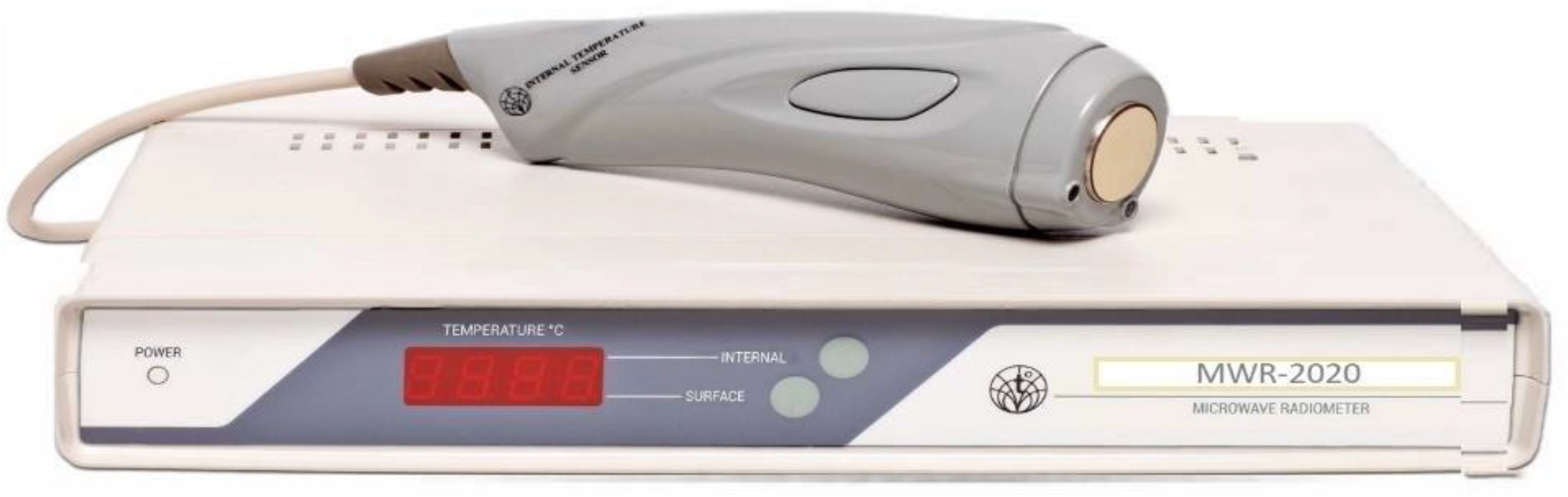
An analysis of the literature and the research has identified a relatively new but little developed method for JIA using MWR. Recently, the MWR method of functional diagnostics has begun to spread widely, which consists of the dynamic mapping of physical fields and radiation from the human body and the method of MWR using MWR-2020 (former RTM-01-RES) or similar devices. MWR-2020 (www.mmwr.co.uk, accessed on 1 May 2020) measures the intensity of passive thermal radiation in microwave and infrared (IR) frequencies (Figure 1).
Figure 1. MWR2020 (former RTM-01-RES).
The spatial representation of the temperature distribution using MWR and IR inside and on the surface of the body helps to determine the zone of the pathological process and possibly its qualitative properties
[19][20]. The essence of the biophysical noninvasive method of MWR is to measure the intrinsic electromagnetic radiation of internal tissues and to identify temperature anomalies of the internal tissues of the body and skin
[21]. The methods for detecting skin temperature have a long history. However, individual skin temperature values fluctuate widely, which often leads to diagnostic errors. In recent years, methods have been developed for measuring the temperature distribution from the surface to the interior of the body, with the detection of the internal temperature profile
[22][23]. The ambient temperature is of great methodological importance for the accurate measurement of the depth temperature
[24]. The method has several positive properties: no radiation exposure; the ability to carry out multiple measurements; non-invasiveness; high sensitivity, which allows for the detection of pathology at the preclinical stage; the simplicity and compactness of the equipment; the clarity of the results; and no contraindications
[25][26].
The rationale for using MWR is the increase in temperature during inflammation. The development of chronic inflammation in JIA is mediated by various disorders of the immune system. The inflammation correlates with changes in the synthesis of a significant spectrum of immune mediators and cytokines. At the same time, proinflammatory cascades of cytokines in different forms of the disease often differ
[27]. The use of MWR in JIA involves the search for a local inflammatory process because of the biochemical processes of local, complex vascular-mesenchymal tissue reactions in response to injury.
The inflammatory process, including immunopathological a priori, as a rule, has a higher temperature than those of the surrounding tissues. This does not depend on the etiological factor but may depend on the time of inflammation and the predominance of the exudative or proliferative process. The reactivity of an organism can also be a significant factor.
Systemic signs are recorded using clinical, biochemical, immunological, and other methods. As a rule, local temperature changes precede structural changes. Therefore, in a clinically inactive state, it is possible to visually assess the presence or absence of an inflammatory process in the osteoarticular system (e.g., synovitis, tenosynovitis, and enthesitis).
JIA is characterized by a chronic non-suppurative inflammatory process of the synovial membrane. The morphological substrate of arthritis manifestations, especially those associated with enthesitis, is an inflammatory fibrosing process with primary localization in tendon-ligamentous structures, its attachment points to the bone, and the synovial membrane of the joints with further lymphoid infiltration and hyperplasia
[28][29].
There are few studies on the use of MWR in JIA, particularly in adult patients. The emergence of research has depended significantly on new equipment and computers. For example, as early as 1987, a strong correlation was found between the microwave thermographic index and the measured clinical and laboratory parameters in a study that scanned 52 knees. This method has been proven to be reproducible, fast, and easy to use at the bedside without a controlled environment, but it has not been clinically followed up
[30].
Studies on the application of the MWR method in pediatric patients have since been conducted. The MWR method was used to determine the depth and skin temperatures in the projection of the knee joints in healthy children aged 8–12 years for comparative analysis. Girls (
n = 22, age 10.0 ± 0.3 years) and boys (
n = 21, age 10.1 ± 0.3 years) were included in the study. During treatment, children aged 6–17 years (
n = 43) in the clinic with a diagnosis of JIA were examined. Standards for the depth temperature in the knee joints of healthy children were established, depending on the measurement zone. It was also shown that the ΔT = t max–t min of the depth temperature in the norm was 1.5–1.6 °C, and that of the skin was 1.4 –1.7 °C. It was found that the temperature field of the skin under normal conditions practically repeats the pattern of the deep temperature field; the lowest temperature was noted above the patella. Clinical visual assessment of the temperature data provides an instant idea of thermal asymmetry. MWR allows for the comparison of the indicators of children with JIA (knee joints) with those of healthy children, assessing the thermal asymmetry of depth and skin temperatures by fields and fields of temperature difference and thermograms of internal and skin temperatures
[31].