Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Bogdan Cretu | -- | 1400 | 2022-07-20 07:43:15 | | | |
| 2 | Camila Xu | -1 word(s) | 1399 | 2022-07-20 08:04:03 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Nistor, C.; Ciuche, A.; Cucu, A.; Serban, B.; Cursaru, A.; Cretu, B.; Cirstoiu, C. Clavicular Malignancies. Encyclopedia. Available online: https://encyclopedia.pub/entry/25308 (accessed on 06 March 2026).
Nistor C, Ciuche A, Cucu A, Serban B, Cursaru A, Cretu B, et al. Clavicular Malignancies. Encyclopedia. Available at: https://encyclopedia.pub/entry/25308. Accessed March 06, 2026.
Nistor, Claudiu-Eduard, Adrian Ciuche, Anca-Pati Cucu, Bogdan Serban, Adrian Cursaru, Bogdan Cretu, Catalin Cirstoiu. "Clavicular Malignancies" Encyclopedia, https://encyclopedia.pub/entry/25308 (accessed March 06, 2026).
Nistor, C., Ciuche, A., Cucu, A., Serban, B., Cursaru, A., Cretu, B., & Cirstoiu, C. (2022, July 20). Clavicular Malignancies. In Encyclopedia. https://encyclopedia.pub/entry/25308
Nistor, Claudiu-Eduard, et al. "Clavicular Malignancies." Encyclopedia. Web. 20 July, 2022.
Copy Citation
The clavicle, or collar bone, is a long (6 inches in adults), tubular, S-shaped bone that is subcutaneous throughout and can be considered “special” for several reasons. It is the first bone to ossify in the embryo, with its two first ossification centers developing between the fifth and sixth weeks of gestation. Malignant clavicular tumors present with local pain, a palpable firm mass or pathological bone fracture, or with the clinical symptoms of the primary tumor (in cases of metastasis).
clavicular malignancies
clavicular resection and reconstruction
clavicular metastasis
1. Introduction
Primary clavicular tumors constitute less than 1% of all bone tumors. Due to this rarity, treating physicians have limited experience with their diagnosis, classification, treatment options, and prognosis [1].
Malignant clavicle tumors may include primary and secondary malignancies and neighboring tumors with clavicular invasion. The importance of this pathology derives from the particular anatomical location of the clavicle, relating to structures of vital importance, as well as the limited reconstructive possibilities after surgical treatment. For primary or single secondary tumors, the optimal treatment is complete or partial resection, with or without subsequent reconstruction. A reported series of cases exhibit the presence of tumors in both the acromial end and diaphyseal region [2][3][4]; however, there is not yet any standardized algorithm for their management. Notably, the clavicle can be considered a “special” type of bone from the perspectives of its embryology, morphology, localization, and function [2][3][5].
2. The Clavicle: A “Special Bone”
The clavicle, or collar bone, is a long (6 inches in adults), tubular, S-shaped bone that is subcutaneous throughout and can be considered “special” for several reasons. It is the first bone to ossify in the embryo, with its two first ossification centers developing between the fifth and sixth weeks of gestation. It is also the last bone to fully ossify at the age of 25–26 years. Unlike other long bones, the clavicle develops via intramembranous ossification [2][3][6][7][8][9][10][11][12].
The clavicle is the only long bone in the human body that is positioned horizontally. It acts as a link between the upper limbs and the thorax, connecting the axial to the appendicular skeleton. Although still under debate, Inman and Saunders propose that the clavicle serves three primary functions: protection of the underlying neurovascular structures, a bony framework for the attachment of muscles, and strut support for the scapula [13].
The structure of the clavicle differs from other long bones in that it almost lacks a medullary cavity and comprises dense trabecular bone with a reduced vascular supply. It offers attachment to several muscles, including the deltoid, trapezius, and pectoralis muscles, and thereby contributes to the upper extremity movement. It also harbors paramount cervicothoracic structures, including the brachial plexus, the subclavian artery, and the pulmonary apex [7][9][11].
3. Clavicular Tumors: Diagnosis
Malignant clavicular tumors present with local pain, a palpable firm mass or pathological bone fracture, or with the clinical symptoms of the primary tumor (in cases of metastasis). Clavicular chondrosarcomas may present with skin ulceration, swelling, or, in rare cases, Horner’s syndrome or even thoracic outlet syndrome [14][15]. Surgical treatment is performed with the dual aims of removing tumoral tissue and alleviating symptoms.
While bone tumors can arise spontaneously, a substantial number occur in the context of a hereditary disorder, thus necessitating a detailed family history for every new case. Some of the most common primitive tumors in the clavicle include eosinophilic granuloma and tumors secondary to hematological disease [16]. Plasmacytoma, osteosarcoma, Ewings sarcoma, and post-radiotherapy sarcomas may also occur in the collarbone [17]. Although the literature describes a multitude of malignant lesions that may exist in the clavicle, this is not a common occurrence (Figure 1) [18][19][20][21][22][23][24].
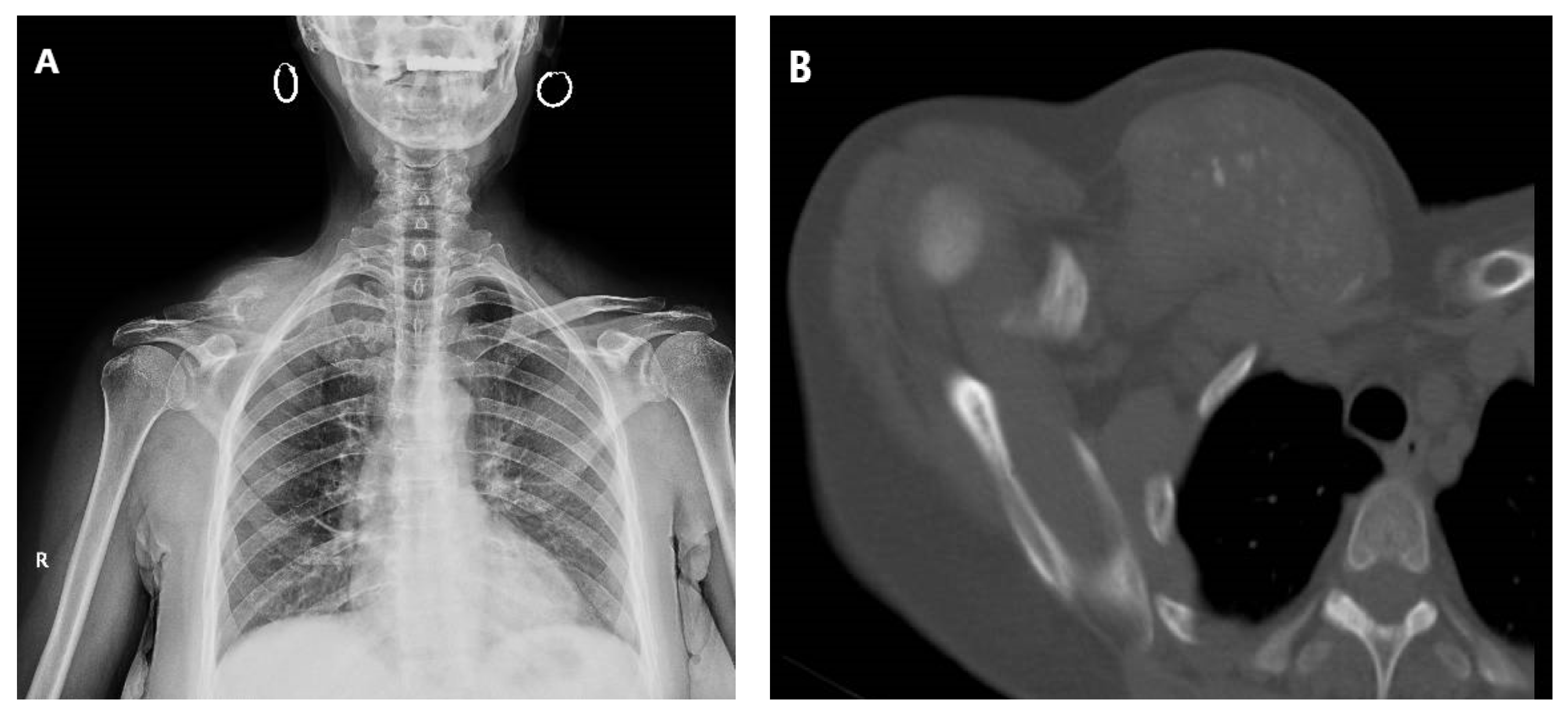 Figure 1. Plain radiograph (A) and tomography (B) revealing extensive locoregional clavicle metastasis in a 60-year-old female, secondary to cervix adenocarcinoma. The patient presented with multiple metastases at diagnosis.
Figure 1. Plain radiograph (A) and tomography (B) revealing extensive locoregional clavicle metastasis in a 60-year-old female, secondary to cervix adenocarcinoma. The patient presented with multiple metastases at diagnosis.Tumors originating in the lung, anterior chest wall (bones/soft tissue), breast, anterior mediastinum, or thyroid can invade the clavicle. Notably, the skeleton is the third site for metastasis, after the lung and liver [25]. In all of these cases, the management algorithm considers the tumor’s origin, the structures invaded, and the size of the chest wall defect after tumor resection with respect to the oncological principle of free margins [26].
Given the proximity of the clavicle to major vessels, nerves, and the thorax, there is a need for standard imaging—including plain film, computed tomography, and magnetic resonance imaging—to evaluate bone destruction and invasion of surrounding tissues (muscles, vessels, and nerves). Whole-body scintigraphy using technetium-99m methylene diphosphonate (99 mTc MDP) and positron emission tomography scan (PET scan) studies are required to diagnose metastases in the bones or other structures. Importantly, the high variability of the radiological appearance complicates the diagnosis of these masses alone [17].
Chondrosarcoma is the second most common bone cancer, with 20% occurring in the shoulder girdle, up to 1% being metastasis from other cancers, and only rare occurrences in the clavicular location (Figure 2) [27]. On the other hand, one-third of chest wall tumors are chondrosarcomas, making this the most common primary bone tumor of the chest wall [17]. Clavicle chondrosarcoma exhibits a lesion-like appearance, similar to that found in other skeletal regions, with specific intratumoral calcifications present in bulky soft tissue masses [28]. Clavicular osteosarcoma is not associated with the classic periosteal reaction or with the mineralized matrix, making imaging-based diagnosis difficult.
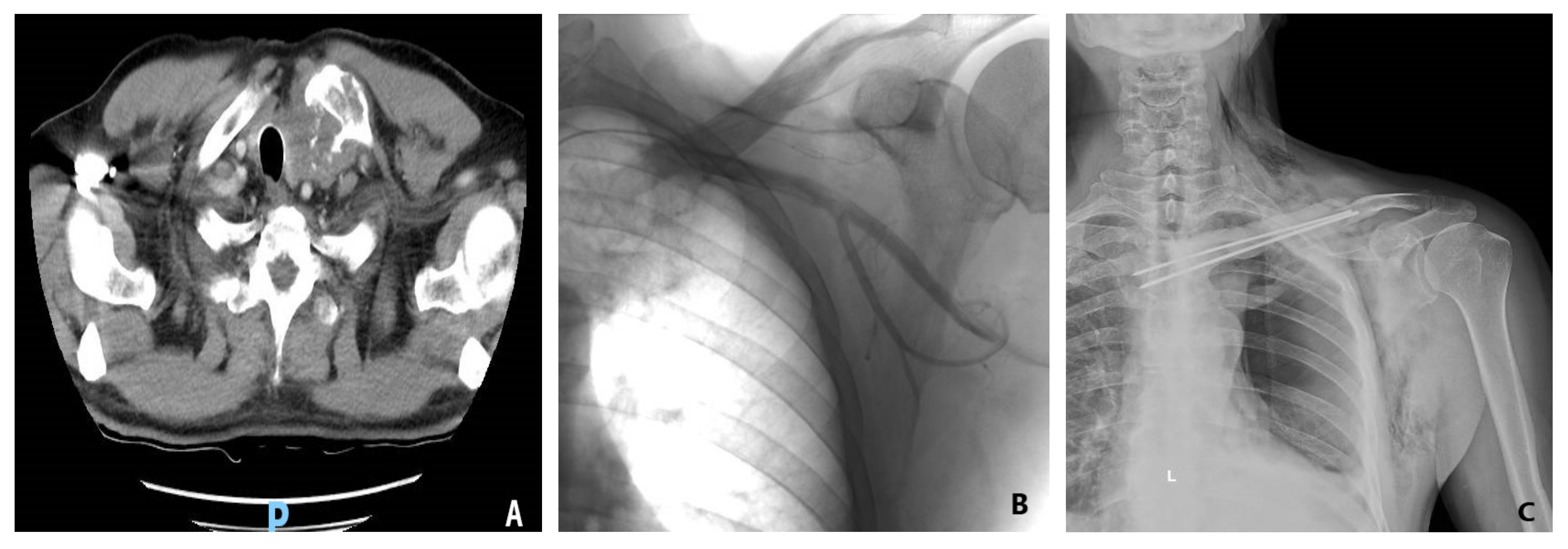 Figure 2. (A) Preoperative tomography of a 66-year-old male diagnosed with clavicle condrosarcoma. (B) Preoperative angiography and embolization of the tumor were performed prior to resection to limit intraoperative blood loss. (C) Postoperative image of acrylic cement reinforced with Kirschner brooches reconstruction used after tumoral resection.
Figure 2. (A) Preoperative tomography of a 66-year-old male diagnosed with clavicle condrosarcoma. (B) Preoperative angiography and embolization of the tumor were performed prior to resection to limit intraoperative blood loss. (C) Postoperative image of acrylic cement reinforced with Kirschner brooches reconstruction used after tumoral resection.Laboratory examinations are relatively unimportant for diagnosing clavicular tumors, except in cases of metastasis, where screening for specific tumor markers might indicate the primary tumor. Preoperative staging is followed by a biopsy (fine needle/excisional or incisional) to confirm whether the tumor is primary or secondary, thus establishing the final diagnosis.
4. Surgical Management and Reconstruction of Clavicular Malignancies
In cases requiring reconstruction, several aspects must be considered: what structure is missing, what is left, what should be replaced, and what are the available means of reconstruction. Reconstruction is influenced by the location, size, and depth of the defect, the viability and quality of adjacent structures (previous radiotherapy, presence of scars), and previous surgery in the area [26]. Post-resection reconstructive methods are limited in cases of unique primary or secondary clavicular tumors. The external third resection of the clavicle does not require reconstruction as long as the coracoclavicular ligaments remain attached but, of course, such cases are rare in discussions of malignancies.
Partial or complete claviculectomy involves substantial peri-operative risks, such as lesions of the subclavian plexus or the brachial plexus, as well as infectious risks [29][30][31]. Post-resection reconstruction of the partial or total claviculectomy is important for several reasons—including maintaining the biomechanics of the scapular girdle, protecting the vessels and nerves, reducing pain, and maintaining the anatomical appearance of the shoulder. One reconstructive method following a complete resection of the clavicle is with a vascularized autograft fibula or rib, and several case reports describe the surgical technique but without comparing claviculectomy with reconstructive procedures [32][33][34]. Alternative reconstruction options involve acrylic cement reinforced with plate and screws or with Kirschner brooches, which may avoid possible complications secondary to complete resection of the collarbone (Figure 2). After reviewing five cases treated with this procedure, the researchers concluded that bone cement prosthesis for bone defect reconstruction after tumor resection can maintain the contour of the shoulder and reduce the complications ascribed to the claviculectomy, and the procedure is effective and feasible [35]. Moreover, the “Oklahoma prosthesis” reconstructive method, with a cement allograft, has been successfully used to maintain the biomechanical integrity of the scapular girdle in cases of clavicular middle third secondary tumors that invade the sternum and rib. The technique consists of an en bloc clavilculectomy and chest wall resection with a method of reconstruction using a single methyl methacrylate and prolene composite prosthesis in a configuration resembling the state of Oklahoma [36].
Due to the small number of studies analyzing clavicular malignancies treated by resection and reconstruction, and the fact that the vast majority of these studies are case reports or include only a small number of cases, it cannot be firmly stated that reconstruction is the best option in terms of preserving scapular girdle functionality and long-term survival rates. To state that reconstruction is mandatory after claviculectomy, there is a need for studies focused on specific patient groups, with analyses of functionality over time and long-term patient survival.
References
- Dahlin, D.C.; Unni, K.K. Bone Tumors: General Aspects and Data on 8542 Cases, 4th ed.; Thomas: Springfield, IL, USA, 1986.
- Priemel, M.H.; Stiel, N.; Zustin, J.; Luebke, A.M.; Schlickewei, C.; Spiro, A.S. Bone tumours of the clavicle: Histopathological, anatomical and epidemiological analysis of 113 cases. J. Bone Oncol. 2019, 16, 100229.
- Kapoor, S.K.; Tiwari, A.; Kapoor, S. Primary tumours and tumorous lesions of clavicle. Int. Orthopaed. 2007, 32, 829–834.
- Klein, M.J.; Lusskin, R.; Becker, M.H.; Antopol, S.C. Osteoid osteoma of the clavicle. Clin. Orthop. 1979, 143, 162.
- Smith, J.; Yuppa, F.; Watson, R.C. Primary tumors and tumor-like lesions of the clavicle. Skelet. Radiol. 1988, 17, 235–246.
- Kumar, R.; Madewell, J.E.; Swischuk, L.E.; Lindell, M.M.; David, R. The clavicle: Normal and abnormal. RadioGraphics 1989, 9, 677–706.
- Bernat, A.; Huysmans, T.; Van Glabbeek, F.; Sijbers, J.; Gielen, J.; Van Tongel, A. The anatomy of the clavicle. Clin. Anat. 2013, 27, 712–723.
- Ogata, S.; Uhthoff, H.K. The early development and ossification of the human clavicle—An embryologic study. Acta Orthop. Scand. 1990, 61, 330–334.
- Ellis, H.; Johnson, D. Pectoral girdle, shoulder and axilla. In Gray’s Anatomy. The Anatomical Basis of Clinical Practice, 39th ed.; Standring, S., Ed.; Elsevier Churchill Livingstone: Edinburgh, UK, 2005; pp. 817–849.
- Smith, J.; McLachlan, D.L.; Huvos, A.G.; Higinbotham, N.L. Primary tumors of the clavicle and scapula. Am. J. Roentgenol. Radium Ther. Nucl. Med. 1975, 124, 113–123.
- Havet, E.; Duparc, F.; Tobenas-Dujardin, A.-C.; Muller, J.-M.; Delas, B.; Fréger, P. Vascular anatomical basis of clavicular non-union. Surg. Radiol. Anat. 2007, 30, 23–28.
- Pressney, I.; Saifuddin, A. Percutaneous image-guided needle biopsy of clavicle lesions: A retrospective study of diagnostic yield with description of safe biopsy routes in 55 cases. Skelet. Radiol. 2014, 44, 497–503.
- Inman, V.T.; Saunders, J.B.D.M. Observations on the function of the clavicle. Calif. Med. 1946, 65, 158–166.
- Huang, J.; Zhang, H.-Z.; Zheng, L.; Zhou, J.; Jiang, Z.-M. Clinicopathologic diagnosis of de-differentiated chondrosarcoma. Chin. J. Pathol. 2009, 38, 820–823.
- Kapoor, V.; Sudheer, V.; Waseem, M.; Cole, A.S.; Weeden, D.F. An Unusual Presentation of Chondrosarcoma of the Clavicle with Horner’s Syndrome. Sarcoma 2004, 8, 87–89.
- Ren, K.; Wu, S.; Shi, X.; Zhao, J.; Liu, X. Primary clavicle tumors and tumorous lesions: A review of 206 cases in East Asia. Arch. Orthop. Trauma. Surg. 2012, 132, 883–889.
- Smith, S.E.; Keshavjee, S. Primary chest wall tumors. Thorac. Surg. Clin. 2010, 20, 495–507.
- Fung, R.; Fasen, M.; Warda, F.; Natter, P.; Nedrud, S.; Fernandes, R.; Alkhasawneh, A.; Gandhi, G.Y. Clavicular Metastasis as an Initial Presentation of Papillary Thyroid Cancer. Case Rep. Endocrinol. 2021, 2021, 6662071.
- Singh, G.K.; Kaur, J.; Sharma, D.; Singh, G.; Singh, P. Isolated Clavicular Metastasis in a Patient with Endometrial Adenocarcinoma. Gynecol. Obstet. 2017, 5, 1000106.
- Albuquerque, A.; Cardoso, H.; Marques, M.; Sarmento, J.A.; Baldaia, H.; Macedo, G. Longstanding Large Clavicular Metastasis of a Hepatocellular Carcinoma in a Non-cirrhotic Liver. Am. J. Gastroenterol. 2012, 107, S403.
- Hong, L.; Qiu, H.; Mei, Z.; Zhang, H.; Liu, S.; Cao, H. Ovarian cancer initially presenting with supra-clavicular lymph node metastasis: A case report. Oncol. Lett. 2018, 16, 505–510.
- Kumar, A.; Arora, N.; Pandove, P.K.; Anand, G.; Arora, B. Pulsatile Clavicular Swelling as the Sole Presentation of Asymptomatic Renal Cell Carcinoma with an Isolated Metastasis to the Clavicle: A Case Report. J. Clin. Diagn. Res. JCDR 2016, 10, PD07–PD08.
- Karabi, K.; Ghosh, T.; Bhattacharya, S.; Ghosh, S. Clavicular metastasis, an initial manifestation of a malignant pheochromocytoma—A case report. J. Cytol. 2007, 24, 189.
- Ganapathy, K.; Ghosh, M. Clavicular metastasis from malignant trigeminal schwannoma. J. Clin. Neurosci. 2003, 10, 485–492.
- Manoso, M.W.; Healey, J.H. Metastatic cancer to the bone. In Cancer: Principles and Practice of Oncology, 7th ed.; DeVita, V.T., Hellman, S., Rosenberg, S.A., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2005; pp. 2368–2380.
- Ferraro, P.; Cugno, S.; Liberman, M.; Danino, M.A.; Harris, P.G. Principles of Chest Wall Resection and Reconstruction. Thorac. Surg. Clin. 2010, 20, 465–473.
- Marulli, G.; Duranti, L.; Cardillo, G.; Luzzi, L.; Carbone, L.; Gotti, G.; Perissinotto, E.; Rea, F.; Pastorino, U. Primary chest wall chondrosarcomas: Results of surgical resection and analysis of prognostic factors. Eur. J. Cardio-Thorac. Surg. 2014, 45, e194–e201.
- Resnick, D. Sternocostoclavicular hyperostosis. Am. J. Roentgenol. 1980, 135, 1278.
- Turra, S.; Gigante, C. Primary clavicular localisation of Ewing’s tumour treated by total cleidectomy. Case report and review of the literature. Ital. J. Orthop. Traumatol. 1988, 14, 389–393.
- Yang, Q.; Li, J.; Yang, Z.; Li, X.; Li, Z. Limb sparing surgery for bone tumours of the shoulder girdle: The oncological and functional results. Int. Orthop. 2009, 34, 869–875.
- Lord, J.W., Jr.; Wright, I.S. Total claviculectomy for neurovascular compression in the thoracic outlet. Surg. Gynecol. Obstet. 1993, 176, 609–612.
- Lenoir, H.; Williams, T.; Kerfant, N.; Robert, M.; Le Nen, D. Free vascularized fibular graft as a salvage procedure for large clavicular defect: A two cases report. Orthop. Traumatol. Surg. Res. 2013, 99, 859–863.
- Guelinckx, P.J.; Sinsel, N.K. The “Eve” Procedure: The Transfer of Vascularized Seventh Rib, Fascia, Cartilage, and Serratus Muscle to Reconstruct Difficult Defects. Plast. Reconstr. Surg. 1996, 97, 527–535.
- Momberger, N.G.; Smith, J.; Coleman, D.A. Vascularized fibular grafts for salvage reconstruction of clavicle nonunion. J. Shoulder Elb. Surg. 2000, 9, 389–394.
- Lin, B.; He, Y.; Xu, Y.; Sha, M. Outcome of bone defect reconstruction with clavicle bone cement prosthesis after tumor resection: A case series study. BMC Musculoskelet. Disord. 2014, 15, 183.
- Vartanian, S.M.; Colaco, S.; Orloff, L.E.; Theodore, P.R. Oklahoma Prosthesis: Resection of Tumor of Clavicle and Chest Wall Reconstructed with a Custom Composite Graft. Ann. Thorac. Surg. 2006, 82, 332–334.
More
Information
Subjects:
Oncology; Orthopedics
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
13.7K
Revisions:
2 times
(View History)
Update Date:
20 Jul 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





