Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Vinicius Facco Rodrigues | -- | 1373 | 2022-07-19 14:07:40 | | | |
| 2 | Camila Xu | Meta information modification | 1373 | 2022-07-20 03:59:39 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Rodrigues, V.F.; Righi, R.D.R.; Costa, C.A.D.; Antunes, R.S. Smart Hospitals and IoT Sensors: The Healthcare Future. Encyclopedia. Available online: https://encyclopedia.pub/entry/25281 (accessed on 07 February 2026).
Rodrigues VF, Righi RDR, Costa CAD, Antunes RS. Smart Hospitals and IoT Sensors: The Healthcare Future. Encyclopedia. Available at: https://encyclopedia.pub/entry/25281. Accessed February 07, 2026.
Rodrigues, Vinicius Facco, Rodrigo Da Rosa Righi, Cristiano André Da Costa, Rodolfo Stoffel Antunes. "Smart Hospitals and IoT Sensors: The Healthcare Future" Encyclopedia, https://encyclopedia.pub/entry/25281 (accessed February 07, 2026).
Rodrigues, V.F., Righi, R.D.R., Costa, C.A.D., & Antunes, R.S. (2022, July 19). Smart Hospitals and IoT Sensors: The Healthcare Future. In Encyclopedia. https://encyclopedia.pub/entry/25281
Rodrigues, Vinicius Facco, et al. "Smart Hospitals and IoT Sensors: The Healthcare Future." Encyclopedia. Web. 19 July, 2022.
Copy Citation
Hospitals are already adopting sensor devices of many types to monitor medical processes. Patients and medical staff can now wear sensors that provide movement and health conditions information in near-real time. Additionally, many sensors can monitor physical settings generating information about the environment and medical equipment. This set of sensors has the potential to provide information to support decision-making processes and medical data analytics. Internet of Things (IoT) is spreading among several areas, paving the way to a new industrial revolution.
healthcare 4.0
internet of things
sensors
1. Introduction
Healthcare 4.0 is coming [1][2]. Hospitals are already adopting sensor devices of many types to monitor medical processes. Patients and medical staff can now wear sensors that provide movement and health conditions information in near-real time. Additionally, many sensors can monitor physical settings generating information about the environment and medical equipment. This set of sensors has the potential to provide information to support decision-making processes and medical data analytics [1][3]. Currently, the analysis of data from medical settings takes place reactively [4]. Medical staff take action to tackle problems with the patients’ health only when critical situations occur. A physician decides the actions to take based solely on traditional examination data from the patient.
This situation exemplifies the reactiveness of medical processes taking action only after an emergency. Further, this process is individual for each patient. It does not contain a centralized analysis of the medical environment. Ideally, decision making should employ a global analysis of the medical processes, generated in real time using data from all patients and the medical environment. In this context, patient remote health monitoring becomes crucial [5]. That would allow proactive data analysis to predict critical situations before they occur.
On top of such infrastructures, it is feasible to employ artificial intelligence technologies [2][5][6]. Among many strategies, three stand out: (i) data prediction [7]; (ii) pattern recognition [8]; and (iii) data correlation [9]. Data prediction allows to forecast measurements and situations, anticipating problems and the required countermeasures. In turn, pattern recognition offers strategies to identify situations that have already occurred in the past. Lastly, data correlation combines information from multiple parameters to identify the source of specific situations. For instance, data correlation strategies are currently employed for ICU patients with Coronavirus Disease 2019 (COVID-19) to identify the relation between many indicators [10].
Figure 1 presents an overview of future medical processes. Internet of Things (IoT) is spreading among several areas, paving the way to a new industrial revolution [6][11]. In hospitals, this is not different [4]. This context encompasses the numerous sensor devices scattered all over the hospital setting generating information from various assets, including the patient and the medical team. Currently, artificial intelligence applications emerge to handle an increasing data volume. It supports the medical team by providing information to help them perceive dangerous situations and patient condition deterioration. Medical processes are highly critical, and errors or delays in handling critical situations may harm the patient and even lead to death. With a wide variety of data provided by IoT technology, centralized systems provide a global analysis of data from patients improving healthcare services.
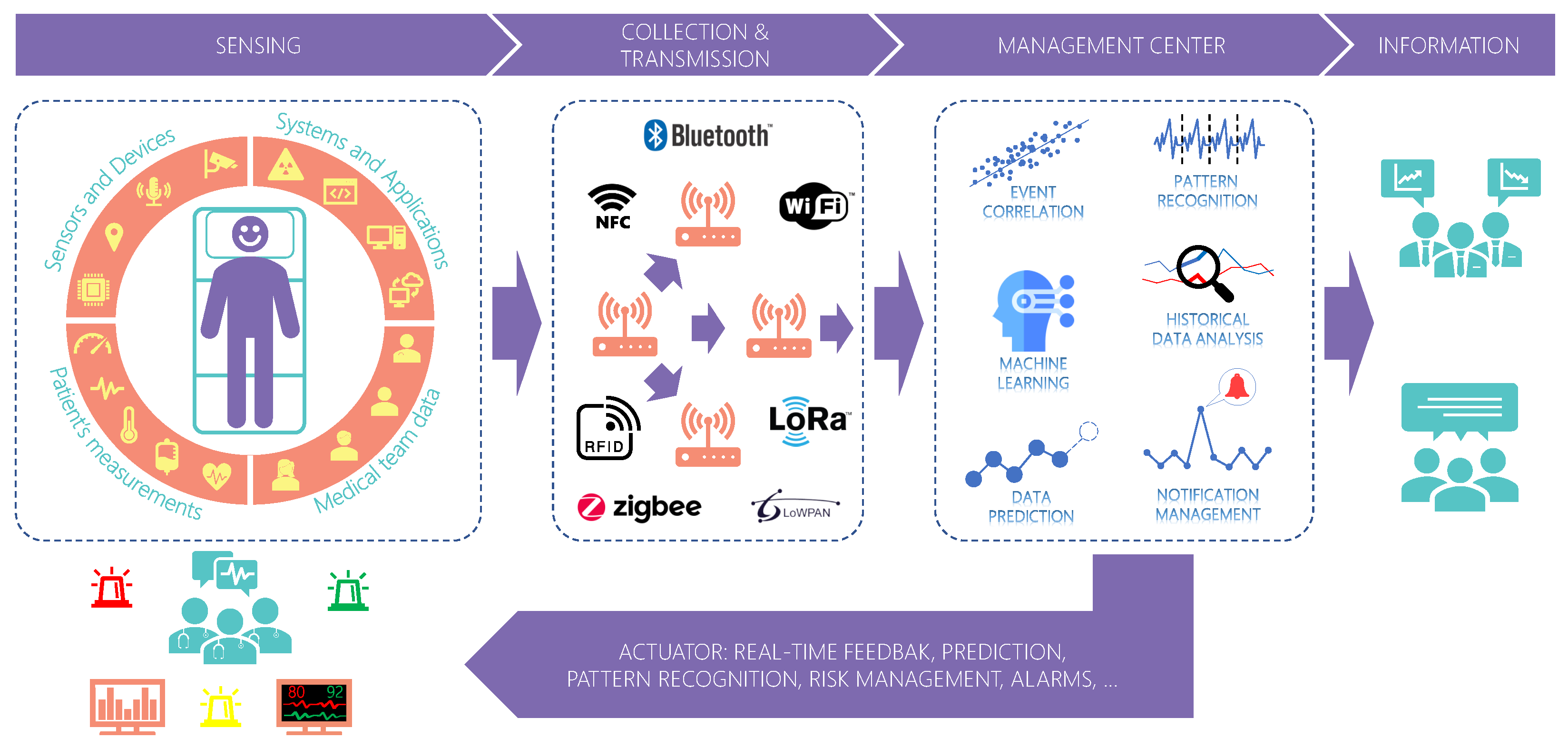 Figure 1. Real-time data acquisition, analysis, and feedback in healthcare. Sensors close to the patient and medical staff generate numerous information collected and transmitted for remote processing. Several applications can profit from this information for further analysis and real-time feedback to actuators.
Figure 1. Real-time data acquisition, analysis, and feedback in healthcare. Sensors close to the patient and medical staff generate numerous information collected and transmitted for remote processing. Several applications can profit from this information for further analysis and real-time feedback to actuators.Although positive, centralized systems suffer from scalability problems which may increase the delay in data transmission. Scalability is the ability of a system to maintain its performance and quality of service (QoS) regardless of the input workload and internal processing [12]. Centralized systems concentrate data processing at a single point. As the number of sensors and applications connected increases, the system can lose performance due to network overload. That would cause instabilities in the data flow to different systems, which can be critical depending on the application. Therefore, a sensor data middleware for medical settings must provide QoS to the applications.
2. Related Work of Smart Hospitals and IoT Sensors
Table 1 summarizes the main articles published in the last four years and their goal and QoS strategy. Among different QoS methods, studies focus mainly on four common strategies: (i) scheduling protocols [13][14]; (ii) data prioritization [13][14][15][16][17][18][19][20]; (iii) routing protocols [20][21][22][23][24][25]; (iv) resource management [14][19]. Studies have examined the use of data prioritization to reduce transmission time. This strategy encompasses distinct classes for each data type, prioritizing high-priority packets. Some approaches use admission control algorithms to ensure a network’s quality. Thus, an algorithm checks the current network state and estimates the future state to decide whether to allow new connections. Cloud environments commonly use resource elasticity, and some researchers use it as a way to provide QoS. During overloaded conditions, such strategies use VM allocation and migration strategies to enhance the performance of some modules. Finally, some researchers also employ routing and scheduling protocols to improve the performance of networks and reduce transmission delays. The routing algorithms determine the most optimal route for transmitting data based on network conditions. On the other hand, scheduling protocols control the time slot assignment for each data transmission and their order based on the amount and type of data.
Table 1. Summary of the research and QoS strategies in healthcare solutions.
| Paper | Year | Real Time | QoS Strategy | Description |
|---|---|---|---|---|
| [26] | 2019 | ✓ | Video smoothing | QoS control algorithm to 5G telemedicine. |
| [16] | 2019 | Data prioritization | Slicing framework for eHealth media applications over 5G networks. | |
| [17] | 2019 | Service differentiation, data categorization and prioritization | Medical grade QoS solution. | |
| [13] | 2019 | ✓ | Service differentiation, routing protocol | QoS-aware multipath algorithm for medical data transmission in a SDN. |
| [27] | 2019 | Clock synchronization | Protocol for QoS and energy efficiency in WBAN. | |
| [18] | 2019 | ✓ | Traffic differentiation | IoT architecture for data access. |
| [19] | 2020 | ✓ | Data prioritization and data rate adaptation | IoT architecture for data access. |
| [23] | 2020 | ✓ | Channel selection | Dynamic channel and superframe selection scheme in IEEE 802.15.6 WBANs to avoid interference. |
| [24] | 2020 | ✓ | Routing protocol | Strategy for selecting an optimal end-to-end route in WBAN. |
| [25] | 2020 | Routing protocol | Routing protocol for WBAN medical data. | |
| [20] | 2020 | Routing protocol and data prioritization | WBAN architecture. | |
| [21] | 2021 | Routing protocol | QoS optimization in IoMT remote health monitoring. | |
| [22] | 2021 | Routing protocol | Routing algorithm for WBAN health monitoring. | |
| [14] | 2021 | Data prioritization, energy control, packet scheduling protocol and data rate adaptation | Patient monitoring using WBAN. | |
| [15] | 2021 | ✓ | Data prioritization | OpenFlow traffic shaping in the Fog using SDN for e-health services. |
| [28] | 2022 | ✓ | Dynamic resource allocation | Private cloud with dynamic resource management for health services. |
| [29] | 2022 | ✓ | Communication protocol | IoT architecture employing edge and fog computing for health services. |
Several studies present QoS strategies for Wireless Body Area Network (WBAN) infrastructures [14][20][22][23][24][25][27]. A WBAN comprises a private network of connected sensors transmitting data to a master node that relays the information to upper network layers. Energy consumption and interference are the main problems studies seek to resolve by employing routing protocols and channel selection strategies. Their primary focus is to improve network transmission from the WBAN to the upper network layers. Such strategies can solve the internal problems of WBANs; however, they do not focus on multiple WBANs simultaneously. In other words, initiatives focusing on WBAN propose QoS strategies only within the WBAN boundaries and not the higher level which consumes data. Recent advances employ fog computing as a new solution to bridge the gap between the sensors and the cloud to decrease response time. Some strategies employ fog to provide data processing closer to the sensors and, therefore, remove network hops needed to reach the cloud [28][29]. Despite its advantages, fog solutions still require data extraction and transmission from the sensors and the fog nodes. Depending on the infrastructure, the volume of data and the quality of the transmission channel can still impose restrictions and impact the QoS.
Within a hospital, there are many critical locations, such as operating rooms, in which a system can provide helpful data from patients and physicians. Most strategies focus on remote health sites, like nursing homes, and only WBANs for patient health monitoring. In addition, a healthcare system has two main actors: the sensors at the hardware level, generating information, and the users at the application level, which consume and process data from the system. Strategies focus mainly on the first level to provide QoS in data transmission from the sensor to the network. Furthermore, although some initiatives present concerns regarding real time, they do not focus intensely on this issue. In general, solutions that focus on real time only consider improving time delay from priority packets or providing an architecture that supports real-time data transmissions.
References
- Tortorella, G.L.; Saurin, T.A.; Fogliatto, F.S.; Rosa, V.M.; Tonetto, L.M.; Magrabi, F. Impacts of Healthcare 4.0 digital technologies on the resilience of hospitals. Technol. Forecast. Soc. Change 2021, 166, 120666.
- Paul, S.; Riffat, M.; Yasir, A.; Mahim, M.N.; Sharnali, B.Y.; Naheen, I.T.; Rahman, A.; Kulkarni, A. Industry 4.0 Applications for Medical/Healthcare Services. J. Sens. Actuator Netw. 2021, 10, 43.
- Giatrakos, N.; Katzouris, N.; Deligiannakis, A.; Artikis, A.; Garofalakis, M.; Paliouras, G.; Arndt, H.; Grasso, R.; Klinkenberg, R.; Ponce De Leon, M.; et al. Interactive Extreme-Scale Analytics: Towards Battling Cancer. IEEE Technol. Soc. Mag. 2019, 38, 54–61.
- Da Costa, C.A.; Pasluosta, C.F.; Eskofier, B.; da Silva, D.B.; da Rosa Righi, R. Internet of Health Things: Toward intelligent vital signs monitoring in hospital wards. Artif. Intell. Med. 2018, 89, 61–69.
- Poncette, A.S.; Mosch, L.; Spies, C.; Schmieding, M.; Schiefenhövel, F.; Krampe, H.; Balzer, F. Improvements in Patient Monitoring in the Intensive Care Unit: Survey Study. J. Med. Internet Res. 2020, 22, e19091.
- Song, H.; Bai, J.; Yi, Y.; Wu, J.; Liu, L. Artificial Intelligence Enabled Internet of Things: Network Architecture and Spectrum Access. IEEE Comput. Intell. Mag. 2020, 15, 44–51.
- Nyce, C.; Cpcu, A. Predictive Analytics White Paper; American Institute for CPCU. Insurance Institute of America: Malvern, PA, USA, 2007; pp. 9–10.
- Tveter, D. The Pattern Recognition Basis of Artificial Intelligence, 1st ed.; IEEE Press: Piscataway, NJ, USA, 1997.
- Williams, A.M.; Liu, Y.; Regner, K.R.; Jotterand, F.; Liu, P.; Liang, M. Artificial intelligence, physiological genomics, and precision medicine. Physiol. Genom. 2018, 50, 237–243.
- Liu, Y.; Gao, W.; Guo, W.; Guo, Y.; Shi, M.; Dong, G.; Ge, Q.; Zhu, J.; Lu, J. Prominent coagulation disorder is closely related to inflammatory response and could be as a prognostic indicator for ICU patients with COVID-19. J. Thromb. Thrombolysis 2020, 50, 825–832.
- Marques, G.; Pitarma, R. mHealth: Indoor Environmental Quality Measuring System for Enhanced Health and Well-Being Based on Internet of Things. J. Sens. Actuator Netw. 2019, 8, 43.
- Bondi, A.B. Characteristics of Scalability and Their Impact on Performance. In Proceedings of the 2nd International Workshop on Software and Performance, Ottawa, ON, Canada, 17–20 September 2000; Association for Computing Machinery: New York, NY, USA, 2000. WOSP ’00. pp. 195–203.
- Venkatesh, K.; Srinivas, L.; Krishnan, M.M.; Shanthini, A. QoS improvisation of delay sensitive communication using SDN based multipath routing for medical applications. Future Gener. Comput. Syst. 2019, 93, 256–265.
- Kathuria, M.; Gambhir, S. Reliable packet transmission in WBAN with dynamic and optimized QoS using multi-objective lion cooperative hunt optimizer. Multimed. Tools Appl. 2021, 80, 10533–10576.
- Bardalai, P.; Medhi, N.; Bargayary, B.; Saikia, D.K. OpenHealthQ: OpenFlow based QoS management of Healthcare Data in a Software-Defined Fog environment. In Proceedings of the ICC 2021—IEEE International Conference on Communications, Montreal, QC, Canada, 14–23 June 2021; pp. 1–6.
- Wang, Q.; Alcaraz-Calero, J.; Ricart-Sanchez, R.; Weiss, M.B.; Gavras, A.; Nikaein, N.; Vasilakos, X.; Giacomo, B.; Pietro, G.; Roddy, M.; et al. Enable Advanced QoS-Aware Network Slicing in 5G Networks for Slice-Based Media Use Cases. IEEE Trans. Broadcast. 2019, 65, 444–453.
- Al-Tarawneh, L.A. Medical Grade QoS Improvement Using IEEE802.11e WLAN Protocol. In Proceedings of the Smart Technologies and Innovation for a Sustainable Future, Dubai, United Arab Emirates, 15–16 November 2017; Al-Masri, A., Curran, K., Eds.; Springer International Publishing: Cham, Swizerland, 2019; pp. 229–235.
- Khalil, A.; Mbarek, N.; Togni, O. IoT Service QoS Guarantee Using QBAIoT Wireless Access Method. In Proceedings of the Mobile, Secure, and Programmable Networking, Mohammedia, Morocco, 23–24 April 2019; Renault, É., Boumerdassi, S., Bouzefrane, S., Eds.; Springer International Publishing: Cham, Swizerland, 2019; pp. 157–173.
- Goyal, R.; Patel, R.; Bhaduria, H.; Prasad, D. An Energy Efficient QoS Supported Optimized Transmission Rate Technique in WBANs. Wirel. Pers. Commun. 2020, 117, 235–260.
- Ibrahim, A.A.; Bayat, O.; Ucan, O.N.; Salisu, S. Weighted Energy and QoS based Multi-hop Transmission Routing Algorithm for WBAN. In Proceedings of the 6th International Engineering Conference “Sustainable Technology and Development” (IEC), Erbil, Iraq, 26–27 February 2020; IEEE: Piscataway, NJ, USA, 2020; pp. 191–195.
- Gautam, A.; Mahajan, R.; Zafar, S. QoS Optimization in Internet of Medical Things for Sustainable Management. In Cognitive Internet of Medical Things for Smart Healthcare: Services and Applications; Hassanien, A.E., Khamparia, A., Gupta, D., Shankar, K., Slowik, A., Eds.; Springer International Publishing: Cham, Swizerland, 2021; pp. 163–179.
- Adhikary, S.; Ghosh, B.; Choudhury, S. QoS Enhancement in WBAN with Twin Coordinators. In Advanced Computing and Systems for Security: Volume Eleven; Chaki, R., Cortesi, A., Saeed, K., Chaki, N., Eds.; Springer: Singapore, 2021; pp. 85–97.
- Tseng, H.W.; Wang, Y.B.; Yang, Y. An Adaptive Channel Hopping and Dynamic Superframe Selection Scheme With QoS Considerations for Emergency Traffic Transmission in IEEE 802.15.6-Based Wireless Body Area Networks. IEEE Sens. J. 2020, 20, 3914–3929.
- Zuhra, F.T.; Baka, K.B.A.; Ahmed, A.; Khan, U.A.; Bhangwar, A.R. MIQoS-RP: Multi-Constraint Intra-BAN, QoS-Aware Routing Protocol for Wireless Body Sensor Networks. IEEE Access 2020, 8, 99880–99888.
- Waheed, T.; Rehman, A.U.; Karim, F.; Ghani, S. QoS Enhancement of AODV Routing for MBANs. Wirel. Pers. Commun. 2020, 116, 1379–1406.
- Sodhro, A.H.; Luo, Z.; Sangaiah, A.K.; Baik, S.W. Mobile edge computing based QoS optimization in medical healthcare applications. Int. J. Inf. Manag. 2019, 45, 308–318.
- Bai, T.; Lin, J.; Li, G.; Wang, H.; Ran, P.; Li, Z.; Pang, Y.; Wu, W.; Jeon, G. An optimized protocol for QoS and energy efficiency on wireless body area networks. Peer Peer Netw. Appl. 2019, 12, 326–336.
- Gong, S.; Zhu, X.; Zhang, R.; Zhao, H.; Guo, C. An Intelligent Resource Management Solution for Hospital Information System Based on Cloud Computing Platform. IEEE Trans. Reliab. 2022, 1–14.
- Dammak, B.; Turki, M.; Cheikhrouhou, S.; Baklouti, M.; Mars, R.; Dhahbi, A. LoRaChainCare: An IoT Architecture Integrating Blockchain and LoRa Network for Personal Health Care Data Monitoring. Sensors 2022, 22, 1497.
More
Information
Subjects:
Computer Science, Interdisciplinary Applications; Computer Science, Information Systems; Health Care Sciences & Services
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
2.0K
Revisions:
2 times
(View History)
Update Date:
20 Jul 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




