Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Hee-Jin Kim | -- | 1106 | 2022-07-13 11:08:09 | | | |
| 2 | Dean Liu | -17 word(s) | 1089 | 2022-07-14 02:54:11 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Yi, K.; Kim, H. Botulinum Neurotoxin Injection Targeting Lateral Canthal Rhytids. Encyclopedia. Available online: https://encyclopedia.pub/entry/25096 (accessed on 08 February 2026).
Yi K, Kim H. Botulinum Neurotoxin Injection Targeting Lateral Canthal Rhytids. Encyclopedia. Available at: https://encyclopedia.pub/entry/25096. Accessed February 08, 2026.
Yi, Kyu-Ho, Hee-Jin Kim. "Botulinum Neurotoxin Injection Targeting Lateral Canthal Rhytids" Encyclopedia, https://encyclopedia.pub/entry/25096 (accessed February 08, 2026).
Yi, K., & Kim, H. (2022, July 13). Botulinum Neurotoxin Injection Targeting Lateral Canthal Rhytids. In Encyclopedia. https://encyclopedia.pub/entry/25096
Yi, Kyu-Ho and Hee-Jin Kim. "Botulinum Neurotoxin Injection Targeting Lateral Canthal Rhytids." Encyclopedia. Web. 13 July, 2022.
Copy Citation
Botulinum neurotoxin injections near the lateral canthal rhytids are commonly used in cosmetic settings; however, there is a lack of thorough anatomical knowledge, and an effective way to treat them with accumulating knowledge is needed.
orbicularis oculi muscle
infraorbital wrinkles
facial wrinkle
injection point
1. Introduction
Botulinum neurotoxin (BoNT) stops neuronic linking by seizing the release of acetylcholine at the neuromuscular junction and hindering contraction of the muscle [1][2]. In cosmetic treatment, BoNT is usually used to reduce periorbital wrinkles by diminishing expression in the orbicularis oculi muscle. The main aesthetic concerns in the periorbital region are lateral canthal rhytids (crow’s feet) (Figure 1).
Figure 1. The wrinkles in the eye region are lateral canthal rhytids in many individuals.
The easing of wrinkles through BoNT is performed in numerous cases, and side effects, such as paralysis of nearby muscles causing diplopia and ptosis, have been reported [3][4]. In treating creases with BoNT in the periorbital region, major complications such as diplopia may be caused by inadvertent palsy of the rectus lateralis, medialis, and inferioris [5][6]. Even if there is a low incidence of adverse effects, clinicians should inject anatomically-based exact sites of the orbicularis oculi muscle, and primary treatment should be initiated with a reduced amount of BoNT.
Factors that should be considered are that a substantial number of units and short-term repetitive injections of BoNT build up antibodies that lead to insufficient treatment [7][8][9][10]. Recent findings on BoNT injection points from anatomical perspectives in certain muscles have been based on external anatomical landmarks (Figure 2) [11][12].
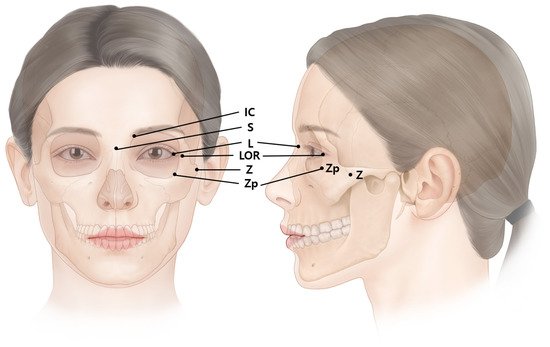
Figure 2. The external anatomical landmark of the eye regions. LOR, lateral orbital rim at the level of lateral canthus; S, sellion; Z, zygion; Zp, zygomatic point located on the outer orbital region; L, lateral canthus; IC, interciliary point located on the frontal notch.
2. Anatomy of the Orbicularis Oculi Muscle
The orbicularis oculi muscle is located around the eyes, and it acts to close the eyelid. The orbicularis oculi muscle can be divided into four parts: orbital portion, palpebral portion, lateral band, and medial band of the orbicularis oculi muscle. The palpebral portion can be subdivided into preseptal and pretarsal portions according to their location (Figure 3).
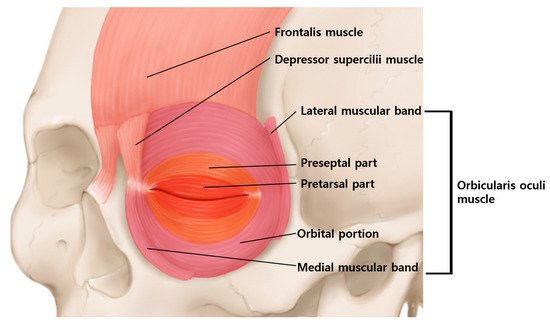
Figure 3. Schematic image of the orbicularis oculi muscle. The orbicularis oculi muscle is divided into the orbital portion and the palpebral portion according to their position. The palpebral portion is subdivided into preseptal and pretarsal portions.
The orbital portion is in the outer region and the muscle originates from both the supraorbital and infraorbital margins. The muscle then encircles and inserts into the lateral canthal tendon, medial canthal tendon, partially to the frontalis muscle, procerus muscle, corrugator supercilii muscles and skin.
In a study by Kim et al., the mean distance from the lateral canthus to the lateral edge of the orbicularis oculi muscle was 31 mm. The medial band of the orbicularis oculi muscle was observed in 64% of the population, whereas the lateral band was observed in 54% (Figure 4) [13].
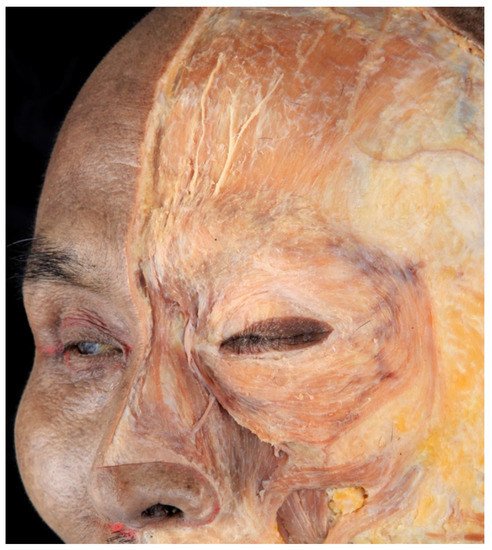
Figure 4. Dissected image of orbicularis orculi muscle. The muscle is composed of lateral and medial muscular band, preseptal and pretarsal part, and orbital portion.
According to Park et al., the lateral muscular band originating from the superficial temporal fascia lateral to the orbicularis oculi muscle was observed in half of the population [14]. The termination of the band was at the zygomatic arch region in 27.9%, at the cheek region 8%, and around mouth corner was 8.2%. This suggests that the lateral band may play a significant role in facial animation or cheek dimple formation and should be considered when treating lateral canthal rhytids.
The orbital portion of the orbicularis oculi muscle firmly closes the eyelids and pulls down the eyebrows. When a person smiles, this portion contracts and lateral canthal rhytids occur around the lateral corners of the eyes.
The palpebral portion consists of the preseptal and pretarsal parts. The preseptal part is located superficially to the orbital septum, whereas the pretarsal part is from the tarsal plate. The palpebral portion of the muscle acts voluntarily and involuntarily, shutting the eyelids when blinking. The palpebral portion produces vertical wrinkles in the medial canthus. The complicated muscle fibers of the orbicularis oculi muscle generate wrinkles in different directions, depending on the location.
According to ultrasonographic findings, the lateral part of the orbicularis oculi muscle is the thickest and appears hypoechoic. The hypoechoic orbicularis oculi muscle continues superiorly with the hyperechoic temporoparietal fascia (Figure 5).
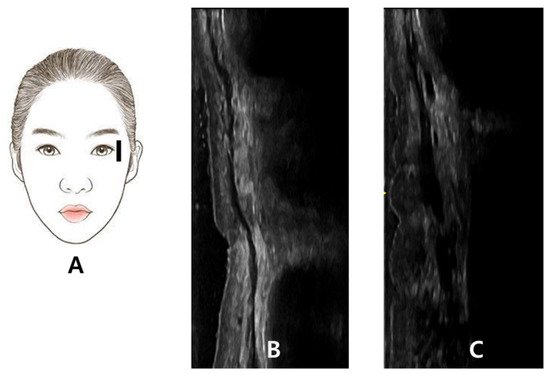
Figure 5. The probe of the ultrasonography has been placed longitudinally at lateral orbital rim at the level of lateral canthus (A). The thin hypoechoic orbicularis oculi muscle observed in ultrasonography during resting state (B). The thick hypoechoic orbicularis oculi muscle is observed in contracted state when asked to smile (C).
3. Injection Points for Lateral Canthal Rhytids
The anatomical landmark for lateral canthal rhytids is the lateral orbital rim at the level of the lateral canthus (Figure 6). From a point 20 mm apart in three directions, superior 30 degree, lateral and inferior 30 degree injection points are proposed.

Figure 6. The injection points for lateral canthal rhytids (Crow’s feet). The light blue dot represents dose of 2 U, while green dot represents dose of 1 U. The degree of the superior and inferior injection is by 30 degrees. The total is 5 U, which is a satisfactory dose for each side. LOR, lateral orbital rim at the level of lateral canthus.
Considering the extension of the orbicularis oculi muscle from the lateral canthus to the lateral edge of the orbicularis oculi muscle is around 3 cm [13] and the fact that BoNT spreads over 1 cm from the injection point, injection into a minimum of three points with 1–2 U of BoNT each, totaling 5 U, is recommended. Borodic et al. demonstrated that BoNT diffuses up to 4.5 cm at a point of injection in case of 10 U into the rabbit longissimus dorsi muscle and the 1 U injection diffusion gradient of 1.5 cm to 3 cm [15].
Next, 2 U were injected at each superior and lateral injection points; and 1 U was injected at the inferior injection point. Inferior point is proposed with lesser dose because, the diffusion of BoNT would affect zygomaticus major and minor giving asymmetrical facial expression. The total was 5 U on each side. The injection points were located around the border of the orbicularis oculi muscle. This is to avoid the venous damage of the sentinel and inferior palpebral veins that runs near the orbital rim. In addition, serious side effects such as diplopia can be prevented by injection away from the orbital rim. Although the injection is conducted in the margin of the orbicularis oculi muscle, BoNT diffuses to 1.5-3 cm which is sufficient to be effective in lateral canthal rhytids [16].
References
- Dessy, L.A.; Mazzocchi, M.; Rubino, C.; Mazzarello, V.; Spissu, N.; Scuderi, N. An objective assessment of botulinum toxin A effect on superficial skin texture. Ann. Plast. Surg. 2007, 58, 469–473.
- Childers, M.K. Targeting the neuromuscular junction in skeletal muscles. Am. J. Phys. Med. Rehabil. 2004, 83, S38–S44.
- Wutthiphan, S.; Kowal, L.; O’Day, J.; Jones, S.; Price, J. Diplopia following subcutaneous injections of botulinum A toxin for facial spasms. J. Pediatr. Ophthalmol. Strabismus 1997, 34, 229–234.
- Lee, J.J.; Jeon, H.S.; Choi, H.Y. Three Cases of Esotropia after Cosmetic Botulinum Toxin A Use in the Eyelid. J. Korean Ophthalmol. Soc. 2015, 56, 799–802.
- Chen, C.S.; Miller, N.R. Botulinum toxin injection causing lateral rectus palsy. Br. J. Ophthalmol. 2007, 91, 843.
- Aristodemou, P.; Watt, L.; Baldwin, C.; Hugkulstone, C. Diplopia associated with the cosmetic use of botulinum toxin a for facial rejuvenation. Ophthalmic Plast. Reconstr. Surg. 2006, 22, 134–136.
- Hsu, T.S.; Dover, J.S.; Arndt, K.A. Effect of volume and concentration on the diffusion of botulinum exotoxin A. Arch. Dermatol. 2004, 140, 1351–1354.
- Kinnett, D. Botulinum toxin A injections in children: Technique and dosing issues. Am. J. Phys. Med. Rehabil. 2004, 83, S59–S64.
- Lepage, D.; Parratte, B.; Tatu, L.; Vuiller, F.; Monnier, G. Extra- and intramuscular nerve supply of the muscles of the anterior antebrachial compartment: Applications for selective neurotomy and for botulinum toxin injection. Surg. Radiol. Anat. 2005, 27, 420–430.
- Pingel, J.; Nielsen, M.S.; Lauridsen, T.; Rix, K.; Bech, M.; Alkjaer, T.; Andersen, I.T.; Nielsen, J.B.; Feidenhansl, R. Injection of high dose botulinum-toxin A leads to impaired skeletal muscle function and damage of the fibrilar and non-fibrilar structures. Sci. Rep. 2017, 7, 14746.
- Yi, K.-H.; Lee, J.-H.; Hu, H.-W.; Kim, H.-J. Novel Anatomical Guidelines on Botulinum Neurotoxin Injection for Wrinkles in the Nose Region. Toxins 2022, 14, 342.
- Yi, K.H.; Lee, J.H.; Hu, H.W.; Kim, H.J. Anatomical Proposal for Botulinum Neurotoxin Injection for Glabellar Frown Lines. Toxins 2022, 14, 268.
- Kim, H.; Seo, K.K.; Lee, H.; Kim, J. Clinical anatomy of the face for filler and botulinum toxin injection. Turk Derm. Derg. 2016, 10, 135.
- Park, J.T.; Youn, K.H.; Hur, M.S.; Hu, K.S.; Kim, H.J.; Kim, H.J. Malaris muscle, the lateral muscular band of orbicularis oculi muscle. J. Craniofac. Surg. 2011, 22, 659–662.
- Borodic, G.E.; Ferrante, R.; Pearce, L.B.; Smith, K. Histologic assessment of dose-related diffusion and muscle fiber response after therapeutic botulinum A toxin injections. Mov. Disord. 1994, 9, 31–39.
- Ramirez-Castaneda, J.; Jankovic, J.; Comella, C.; Dashtipour, K.; Fernandez, H.H.; Mari, Z. Diffusion, spread, and migration of botulinum toxin. Mov. Disord. 2013, 28, 1775–1783.
More
Information
Subjects:
Dermatology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.2K
Revisions:
2 times
(View History)
Update Date:
14 Jul 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




