Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Pingnan Sun | -- | 1624 | 2022-06-23 11:19:47 | | | |
| 2 | Jessie Wu | Meta information modification | 1624 | 2022-06-24 02:16:05 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Zaib, T.; Rashid, H.; Khan, H.; Zhou, X.; Sun, P. Recent Advances in Syndactyly. Encyclopedia. Available online: https://encyclopedia.pub/entry/24373 (accessed on 07 February 2026).
Zaib T, Rashid H, Khan H, Zhou X, Sun P. Recent Advances in Syndactyly. Encyclopedia. Available at: https://encyclopedia.pub/entry/24373. Accessed February 07, 2026.
Zaib, Tahir, Hibba Rashid, Hanif Khan, Xiaoling Zhou, Pingnan Sun. "Recent Advances in Syndactyly" Encyclopedia, https://encyclopedia.pub/entry/24373 (accessed February 07, 2026).
Zaib, T., Rashid, H., Khan, H., Zhou, X., & Sun, P. (2022, June 23). Recent Advances in Syndactyly. In Encyclopedia. https://encyclopedia.pub/entry/24373
Zaib, Tahir, et al. "Recent Advances in Syndactyly." Encyclopedia. Web. 23 June, 2022.
Copy Citation
Syndactyly (SD) is a congenital digital malformation characterized by webbing of the fingers and toes. Syndactyly is derived from the Greek word “syn”, meaning together, and “dactylos”, meaning digits. It is one of the most common hereditary limb disorders, with a prevalence of 3–10 in every 10,000 births, although higher estimates in the range of 10–40/10,000 have been reported.
syndactyly
HOXD13
surgery
1. Classification of Syndactyly
The classification of non-syndromic SD can be performed in different ways, based on the various phenotypes. It can be simple or complex, complete or incomplete, and osseous (bone-involved) or cutaneous (only skin-involved). The classification system of Temtamy and McKusick for non-syndromic syndactyly is largely based on the phenotypic appearance (nature or site of affected limbs), along with segregation of the disorder in affected families [1]. The classification system of Temtamy and McKusick provided the basis for the latest modern classification system, which additionally considers advancements made clinically, as well as in basic molecular studies. In 2012, a nine-type classification system was put forward by Malik et al. that was mainly an extended version of the Temtamy and McKusick classification system [2]. The autosomal dominant mode of inheritance is evident in most of the types [3]. Research summarize the classification of non-syndromic syndactyly in Table 1.
Table 1. List of genes and loci responsible for different types of non-syndromic syndactyly.
| Clinical Phenotype | Original Name | Major Symptoms | Locus/Gene | Mutation Type | Inheritance | References |
|---|---|---|---|---|---|---|
| Syndactyly I-a | Zygodactyly | Cutaneous webbing of 2nd and 3rd toes without the hand involvement | Chr.3p21.31 | - | AD* | [4][5][6] |
| Syndactyly I-b | Lueken type | Bilateral bony or cutaneous webbing of 3rd/4th fingers and 2nd/3rd toes | HOXD13 | Duplication, missense, and deletion | AD | [4][7] |
| Syndactyly I-c | Montagu type | Bilateral bony or cutaneous webbing of 3rd/4th fingers, with normal feet | HOXD13 | Duplication, missense, and deletion | AD | [4][8] |
| Syndactyly I-d | Castilla type | Bilateral cutaneous webbing of the 4th and 5th toes | - | - | AD | [2][4][9] |
| Syndactyly II-a | Vordingborg type | Distinct combinations of syndactyly and polydactyly | HOXD13 | Duplication, missense, frameshift, splicing and deletion | AD | [10][11][12] |
| Syndactyly II-b | Metacarpal and metatarsal synostoses | FBLN1 | Missense | AD | [10][13] | |
| Syndactyly II-c | Cutaneous webbing, abnormal metacarpals | Chr.14q11.2-12 | - | AD | [14] | |
| Syndactyly III | Johnston-Kirby type | Bilateral complete syndactyly of the 4th and 5th fingers | Chr.7q36.3 | - | AD | [5][15][16] |
| Syndactyly IV | Haas-type polysyndactyly | Complete cutaneous syndactyly of all fingers | LMBR1 | Large duplications and missense | AD | [17][18][19][20] |
| Syndactyly V | Dowd type | Synostotic fusion of metacarpals | HOXD13 | Duplication, missense, and deletion | AD | [21][22][23] |
| Syndactyly VI | Mitten type | Fusion of 2nd–5th fingers of the right hand | - | - | AD | [1] |
| Syndactyly VII-a | Cenani-Lenz syndactyly (CLS) | Bony fusion of all digits | LRP4 | Missense | AR* | [24][25] |
| Syndactyly VII-b | 15q13.3, GREM1-FMN1 | - | - | [26] | ||
| Syndactyly VIII | Orel-Holmes type | Fusion of metacarpals 4/5 | FGF16 | Nonsense | XR* | [15] |
| Syndactyly IX | Mesoaxial synostotic syndactyly (MSSD) | Phalangeal reduction | BHLHA9 | Missense, frameshift, and deletion | AR | [27][28][29] |
AD* = autosomal dominant, AR* = autosomal recessive, XR* = X-linked recessive.
2. Diagnosis and Surgical Treatment of Syndactyly
SD is basically a limb malformation that belongs to congenital anomalies affecting bone or skeletal structure or function. It is caused when the digits of the fetus in the womb do not separate successfully, resulting in a webbed hand or feet. As an apparent deformity of the hands and feet, the characteristic is so obvious that it attracts instant attention or concern soon after birth, especially when it occurs in the hands. SD can be managed using different diagnostic tools, plus a genetic background of the patient’s family history and clinical data regarding deformities in affected family members. Genetic screening of the affected person and affected family members can easily reveal information about the genetic background, which can make it easy for a clinician to diagnose the deformity. Furthermore, other tools, such as X-rays and ultrasound, can also make the deformity clearer to the clinician and, therefore, more easily diagnosed. In the presence of all this information, a clinician will be able to diagnose the problem immediately and perform treatment effectively and efficiently [30][31]. Furthermore, after successfully diagnosing the deformity, genetic analysis of the patient and his family members will be helpful in establishing a clearer genotype–phenotype correlation. Researchers have proposed a genetic analysis procedure in the form of a schematic diagram to obtain clearer genotype–phenotype correlation in future (Figure 1).
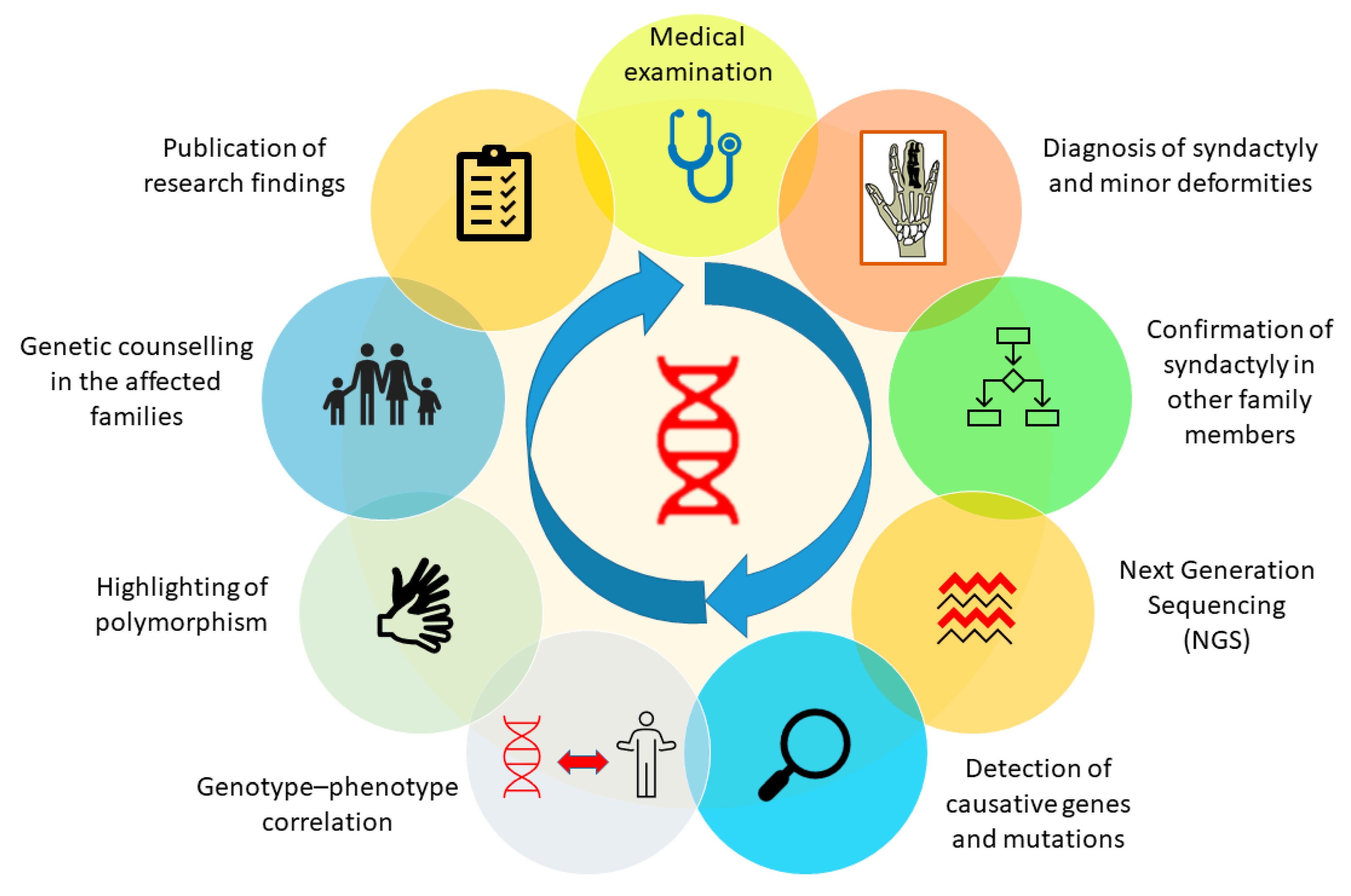
Figure 1. Genetic analysis procedure to attain a clearer genotype-phenotype correlation in all types of syndactyly.
The most important aim and objective of surgical treatment for SD is to minimize possible complications, reinstate the space between the digits, and detach the limbs by using minimal medical techniques and avoiding problems that are likely to happen, such as recurrence and post-surgery complications, until a useful hand is obtained [32]. Skin implantation, open treatment, and the zigzag method of surgery techniques are usually conducted in corrective SD patient surgeries. Surgical outcomes in SD are more positive in simple-type SD compared to complex-type SD. In the United States, a recent study reported that the occurrence of SD is roughly 7 for every 10,000 babies born and that almost every affected child receives surgery before reaching two years of age. The study also pointed out that there may be some genuine problems in getting immediate health care, which includes accessibility to specialized surgeons for correcting limb deformity, failure to get to well-equipped hospitals, especially for people living in remote areas, and poor financial status [33].
The most significant and simple way to eliminate the deformity is early treatment of new-borns by surgery. For new-borns with simple SD, the best age to receive surgery ranges from 6 to 18 months old, whereas in case of complex syndactyly, surgery should be performed prior to 6 months of age [32]. It is very difficult to predict the effectiveness of the surgery because of the tremendous variety and phenotypic range of SD types. The simpler the SD, the higher the chance of achieving useful and fully recovered hand movement [34]. In case of simple SD, corrective and operational outcomes are typically excellent, with fewer chances of recurrence or the possibility of re-arising hand-related problems, whereas in case of complex SD, the chances of post-surgery complications are higher and involve difficulty in normal hand movement and nail deformities [18][34][35]. Complex-SD patients who have received surgery always require revisiting the clinician or surgeon to diagnose post-operative complications.
Surgeons specializing in pediatrics often admit children with rare limb deformities. Closely associated deformities and syndromes should be always taken into consideration, because if not diagnosed accurately, surgery in that case can lead the patient into a worsen situation [36]. The main principle of the surgical treatment of SD and other associated limb deformities is to gain functional and useful limbs with less chance of recurrence. Skin grafts are the operational procedures most commonly used for corrective purposes in limbs affected with SD [37], although open-treatment methods for SD avoid leftover postoperative marks on the skin and are comparatively useful, with the best end results [38]. Several modern surgical techniques have been successfully practiced in the clinics with the aim of achieving useful limbs with no post-operative scars, smooth mobility of the digits, and fewer chances of recurrence. The free skin graft (full-thickness) surgical technique produces the best results when practiced in combination with the Z-method of incision, which can successfully diminish the scars usually obtained at the end of surgery and, as a result, can attain fully functional and useful limbs [39]. Recently, a technique called the improved flap technique was successfully implemented and involves the use of skin grafts with full thickness and different types of flaps to provide sufficient soft tissue cover. The results involved no post-operative complications, provided full recovery of the affected hand, and no discomfort to the child who received surgery [40]. Furthermore, the use of a dermal fat graft surgical technique specifically intended for treating the complex type of SD has recently been introduced [41]. In recent years, the use of abdominal flaps for complex SD release has also proved to be successful [42]. The part of the donor skin used for the corrective surgery of simple or complicated SD must have the features of both dorsal and palm skin as it can leave post-operative skin flaws in the digits, which can eventually affect mobility. Recently, it has been demonstrated that for the surgical purposes of SD, a gradation skin graft is far better cosmetically, compared to skin grafts from the sub-malleolar part, as it has been used traditionally; however, proper alignment with other parts is critical [43].
In case of the treatment of webbed toes in SD, it is slightly more complicated to perform surgery in children because of its high recurrence rate and post-surgery complications, especially in those children who are older than 24 months (the younger the age of the child at the time of surgery, lower the risk of recurrence) [44]. Recently, it has been demonstrated that the most effective surgical procedure suitable for both simple and complex SD involves the interdigitating of rectangular flaps because of its simple design, flexibility in alteration during surgery, and inclusive flap tips [45]. Another study suggested that the dorsal hexagon flap can be a useful substitute technique in treating syndactyly [46]. Furthermore, for skin grafting in which the donor site of the patient also gets disturbed, dorsal rectangular flaps can be very useful, with appealing results for the patient [47]. Based on the condition of the deformity, an individualized treatment plan should be made that can better restore the shape and function of the thumb, especially in SD5 [48]. Moreover, the use of methotrexate can reduce keloid formation just after the dissection of the webbed digits [49].
Post-operative check-ups of the patients should be frequently arranged prior to complete recovery to avoid any difficulties due to surgery [32]. Overall, treatment and surgery for SD are carried out by surgeons of other specialties, which shows that SD treatment is a harmless and effective process with few postoperative complications, but it does need to be followed up by clinicians to ensure fully recovered limbs [50].
References
- Temtamy, S.A.; McKusick, V.A. The genetics of hand malformations. Birth Defects Orig. Artic. Ser. 1978, 14, 1–619.
- Malik, S. Syndactyly: Phenotypes, genetics and current classification. Eur. J. Hum. Genet. 2012, 20, 817–824.
- Sobreira, N.L.; Cernach, M.C.; Brunoni, D.; Perez, A.B. Complex toe syndactyly with characteristic facial phenotype: A new syndrome? Am. J. Med. Genet. A 2008, 146A, 1725–1728.
- Malik, S.; Schott, J.; Ali, S.W.; Oeffner, F.; Amin-ud-Din, M.; Ahmad, W.; Grzeschik, K.H.; Koch, M.C. Evidence for clinical and genetic heterogeneity of syndactyly type I: The phenotype of second and third toe syndactyly maps to chromosome 3p21.31. Eur. J. Hum. Genet. 2005, 13, 1268–1274.
- Al-Qattan, M.M.; Shamseldin, H.E.; Al Mazyad, M.; Al Deghaither, S.; Alkuraya, F.S. Genetic heterogeneity in type III familial cutaneous syndactyly and linkage to chromosome 7q36. Am. J. Med. Genet. A 2013, 161A, 1579–1584.
- Andersen, H.J.; Hansen, A.K. Tibial hypo-/aplasia with preaxial syn- and polydactyly. Arch. Orthop. Trauma Surg. 1990, 109, 231–233.
- Bosse, K.; Betz, R.C.; Lee, Y.A.; Wienker, T.F.; Reis, A.; Kleen, H.; Propping, P.; Cichon, S.; Nothen, M.M. Localization of a gene for syndactyly type 1 to chromosome 2q34-q36. Am. J. Hum. Genet. 2000, 67, 492–497.
- Dai, L.; Liu, D.; Song, M.; Xu, X.; Xiong, G.; Yang, K.; Zhang, K.; Meng, H.; Guo, H.; Bai, Y. Mutations in the homeodomain of HOXD13 cause syndactyly type 1-c in two Chinese families. PLoS ONE 2014, 9, e96192.
- Akarsu, A.N.; Stoilov, I.; Yilmaz, E.; Sayli, B.S.; Sarfarazi, M. Genomic structure of HOXD13 gene: A nine polyalanine duplication causes synpolydactyly in two unrelated families. Hum. Mol. Genet. 1996, 5, 945–952.
- Malik, S.; Grzeschik, K.H. Synpolydactyly: Clinical and molecular advances. Clin. Genet. 2008, 73, 113–120.
- Sarfarazi, M.; Akarsu, A.N.; Sayli, B.S. Localization of the syndactyly type II (synpolydactyly) locus to 2q31 region and identification of tight linkage to HOXD8 intragenic marker. Hum. Mol. Genet. 1995, 4, 1453–1458.
- Muragaki, Y.; Mundlos, S.; Upton, J.; Olsen, B.R. Altered growth and branching patterns in synpolydactyly caused by mutations in HOXD13. Science 1996, 272, 548–551.
- Debeer, P.; Schoenmakers, E.F.; Thoelen, R.; Holvoet, M.; Kuittinen, T.; Fabry, G.; Fryns, J.P.; Goodman, F.R.; Van de Ven, W.J. Physical map of a 1.5 mb region on 12p11.2 harbouring a synpolydactyly associated chromosomal breakpoint. Eur. J. Hum. Genet. 2000, 8, 561–570.
- Malik, S.; Abbasi, A.A.; Ansar, M.; Ahmad, W.; Koch, M.C.; Grzeschik, K.H. Genetic heterogeneity of synpolydactyly: A novel locus SPD3 maps to chromosome 14q11.2-q12. Clin. Genet. 2006, 69, 518–524.
- Lonardo, F.; Della Monica, M.; Riccardi, G.; Riccio, I.; Riccio, V.; Scarano, G. A family with X-linked recessive fusion of metacarpals IV and V. Am. J. Med. Genet. A 2004, 124A, 407–410.
- Gladwin, A.; Donnai, D.; Metcalfe, K.; Schrander-Stumpel, C.; Brueton, L.; Verloes, A.; Aylsworth, A.; Toriello, H.; Winter, R.; Dixon, M. Localization of a gene for oculodentodigital syndrome to human chromosome 6q22-q24. Hum. Mol. Genet. 1997, 6, 123–127.
- Wieczorek, D.; Pawlik, B.; Li, Y.; Akarsu, N.A.; Caliebe, A.; May, K.J.; Schweiger, B.; Vargas, F.R.; Balci, S.; Gillessen-Kaesbach, G.; et al. A specific mutation in the distant sonic hedgehog (SHH) cis-regulator (ZRS) causes Werner mesomelic syndrome (WMS) while complete ZRS duplications underlie Haas type polysyndactyly and preaxial polydactyly (PPD) with or without triphalangeal thumb. Hum. Mutat. 2010, 31, 81–89.
- Samson, P.; Salazard, B. Syndactyly. Chir. Main 2008, 27 (Suppl. 1), S100–S114.
- Dai, L.; Guo, H.; Meng, H.; Zhang, K.; Hu, H.; Yao, H.; Bai, Y. Confirmation of genetic homogeneity of syndactyly type IV and triphalangeal thumb-polysyndactyly syndrome in a Chinese family and review of the literature. Eur. J. Pediatr. 2013, 172, 1467–1473.
- Lohan, S.; Spielmann, M.; Doelken, S.C.; Flottmann, R.; Muhammad, F.; Baig, S.M.; Wajid, M.; Hulsemann, W.; Habenicht, R.; Kjaer, K.W.; et al. Microduplications encompassing the Sonic hedgehog limb enhancer ZRS are associated with Haas-type polysyndactyly and Laurin-Sandrow syndrome. Clin. Genet. 2014, 86, 318–325.
- Hay, S. Incidence of selected congenital malformations in Iowa. Am. J. Epidemiol. 1971, 94, 572–584.
- Robinow, M.; Johnson, G.F.; Broock, G.J. Syndactyly type V. Am. J. Med. Genet. 1982, 11, 475–482.
- Zhao, X.; Sun, M.; Zhao, J.; Leyva, J.A.; Zhu, H.; Yang, W.; Zeng, X.; Ao, Y.; Liu, Q.; Liu, G.; et al. Mutations in HOXD13 underlie syndactyly type V and a novel brachydactyly-syndactyly syndrome. Am. J. Hum. Genet. 2007, 80, 361–371.
- Khan, T.N.; Klar, J.; Ali, Z.; Khan, F.; Baig, S.M.; Dahl, N. Cenani-Lenz syndrome restricted to limb and kidney anomalies associated with a novel LRP4 missense mutation. Eur. J. Med. Genet. 2013, 56, 371–374.
- Li, Y.; Pawlik, B.; Elcioglu, N.; Aglan, M.; Kayserili, H.; Yigit, G.; Percin, F.; Goodman, F.; Nurnberg, G.; Cenani, A.; et al. LRP4 mutations alter Wnt/beta-catenin signaling and cause limb and kidney malformations in Cenani-Lenz syndrome. Am. J. Hum. Genet. 2010, 86, 696–706.
- Dimitrov, B.I.; Voet, T.; De Smet, L.; Vermeesch, J.R.; Devriendt, K.; Fryns, J.P.; Debeer, P. Genomic rearrangements of the GREM1-FMN1 locus cause oligosyndactyly, radio-ulnar synostosis, hearing loss, renal defects syndrome and Cenani--Lenz-like non-syndromic oligosyndactyly. J. Med. Genet. 2010, 47, 569–574.
- Percin, E.F.; Percin, S.; Egilmez, H.; Sezgin, I.; Ozbas, F.; Akarsu, A.N. Mesoaxial complete syndactyly and synostosis with hypoplastic thumbs: An unusual combination or homozygous expression of syndactyly type I? J. Med. Genet. 1998, 35, 868–874.
- Malik, S.; Percin, F.E.; Ahmad, W.; Percin, S.; Akarsu, N.A.; Koch, M.C.; Grzeschik, K.H. Autosomal recessive mesoaxial synostotic syndactyly with phalangeal reduction maps to chromosome 17p13.3. Am. J. Med. Genet. A 2005, 134, 404–408.
- Khan, A.; Wang, R.; Han, S.; Ahmad, W.; Zhang, X. A novel homozygous missense mutation in BHLHA9 causes mesoaxial synostotic syndactyly with phalangeal reduction in a Pakistani family. Hum. Genome Var. 2017, 4, 17054.
- Jin, H.; Lin, P.F.; Wang, Q.M.; Mao, F.; Cai, Y.; Gong, Y.Q. Synpolydactyly in a Chinese kindred: Mutation detection, prenatal ultrasonographic and molecular diagnosis. Zhonghua Yi Xue Yi Chuan Xue Za Zhi 2011, 28, 601–605.
- Bates, S.J.; Hansen, S.L.; Jones, N.F. Reconstruction of congenital differences of the hand. Plast. Reconstr. Surg. 2009, 124, 128e–143e.
- Dao, K.D.; Shin, A.Y.; Billings, A.; Oberg, K.C.; Wood, V.E. Surgical treatment of congenital syndactyly of the hand. J. Am. Acad. Orthop. Surg. 2004, 12, 39–48.
- Swarup, I.; Zhang, Y.; Do, H.; Daluiski, A. Epidemiology of syndactyly in New York State. World J. Orthop. 2019, 10, 387–393.
- Kvernmo, H.D.; Haugstvedt, J.R. Treatment of congenital syndactyly of the fingers. Tidsskr. Den Nor. Legeforening 2013, 133, 1591–1595.
- Goldfarb, C.A.; Steffen, J.A.; Stutz, C.M. Complex syndactyly: Aesthetic and objective outcomes. J. Hand Surg. Am. 2012, 37, 2068–2073.
- Little, K.J.; Cornwall, R. Congenital Anomalies of the Hand--Principles of Management. Orthop. Clin. N. Am. 2016, 47, 153–168.
- Mandarano-Filho, L.G.; Bezuti, M.T.; Akita, R.; Mazzer, N.; Barbieri, C.H. Congenital syndactyly: Case by case analysis of 47 patients. Acta Ortopédica Bras. 2013, 21, 333–335.
- Hikosaka, M.; Ogata, H.; Nakajima, T.; Kobayashi, H.; Hattori, N.; Onishi, F.; Tamada, I. Advantages of open treatment for syndactyly of the foot: Defining its indications. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2009, 43, 148–152.
- Gawlikowska-Sroka, A. Polydactyly and syndactyly as the most common congenital disorders of the limbs. Ann. Acad. Med. Stetin. 2008, 54, 130–133.
- Geoghegan, L.; Knowles, B.G.; Nikkhah, D. Syndactyly. J. Surg. Case Rep. 2020, 2020, rjaa517.
- Senda, E.; Ueda, K.; Hirota, Y.; Mitsuno, D.; Nuri, T. Using Dermal Fat Graft to Release Complex Syndactyly: A New Method. Plast. Reconstr. Surg. Glob. Open 2020, 8, e3068.
- Pei, J.; Zhang, J.; Song, B. The use of abdominal flaps for complex syndactyly release: A case series. J. Hand Surg. 2021, 46, 552–554.
- Sasaki, K.; Sasaki, M.; Oshima, J.; Aihara, Y.; Sekido, M. Aesthetic reconstruction for syndactyly using the “gradation skin graft” from the plantar instep area. J. Plast. Reconstr. Aesthet. Surg. 2021, 74, 3371–3376.
- Langlais, T.; Rougereau, G.; Marty-Diloy, T.; Bachy, M.; Barret, H.; Vialle, R.; Fitoussi, F. Surgical treatment in child’s congenital toe syndactyly: Risk factor of recurrence, complication and poor clinical outcomes. Foot Ankle Surg. 2022, 28, 107–113.
- Yoon, A.P.; Jones, N.F. Interdigitating Rectangular Flaps and Dorsal Pentagonal Island Flap for Syndactyly Release. J. Hand Surg. Am. 2019, 44, 288–295.
- Wang, S.; Zheng, S.; Li, N.; Feng, Z.; Liu, Q. Dorsal Hexagon Local Flap Without Skin Graft for Web Reconstruction of Congenital Syndactyly. J. Hand Surg. Am. 2020, 45, 63.e61–63.e69.
- Yuan, F.; Zhong, L.; Chung, K.C. Aesthetic Comparison of Two Different Types of Web-Space Reconstruction for Finger Syndactyly. Plast. Reconstr. Surg. 2018, 142, 963–971.
- Tang, H.; Sun, G.; Qi, J.; Nie, K.; Jin, W.; Li, S.; Wei, Z.; Wang, D. Surgical Treatment of Congenital Type V Thumb Syndactyly. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2016, 30, 1127–1129.
- Kong, B.Y.; Baek, G.H.; Gong, H.S. Treatment of keloid formation following syndactyly division: Surgical technique. Hand Surg. 2012, 17, 433–437.
- Chouairi, F.; Mercier, M.R.; Persing, J.S.; Gabrick, K.S.; Clune, J.; Alperovich, M. National Patterns in Surgical Management of Syndactyly: A Review of 956 Cases. Hand 2020, 15, 666–673.
More
Information
Subjects:
Genetics & Heredity
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
883
Revisions:
2 times
(View History)
Update Date:
24 Jun 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




