Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Bogdan Florin Iliescu | -- | 1872 | 2022-05-27 07:49:24 | | | |
| 2 | Conner Chen | Meta information modification | 1872 | 2022-05-27 07:54:21 | | | | |
| 3 | Conner Chen | Meta information modification | 1872 | 2022-05-30 08:50:08 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Iliescu, B.; Costachescu, B.; , . Analysis of the Classification Systems for Thoracolumbar Fractures. Encyclopedia. Available online: https://encyclopedia.pub/entry/23470 (accessed on 08 February 2026).
Iliescu B, Costachescu B, . Analysis of the Classification Systems for Thoracolumbar Fractures. Encyclopedia. Available at: https://encyclopedia.pub/entry/23470. Accessed February 08, 2026.
Iliescu, Bogdan, Bogdan Costachescu, . "Analysis of the Classification Systems for Thoracolumbar Fractures" Encyclopedia, https://encyclopedia.pub/entry/23470 (accessed February 08, 2026).
Iliescu, B., Costachescu, B., & , . (2022, May 27). Analysis of the Classification Systems for Thoracolumbar Fractures. In Encyclopedia. https://encyclopedia.pub/entry/23470
Iliescu, Bogdan, et al. "Analysis of the Classification Systems for Thoracolumbar Fractures." Encyclopedia. Web. 27 May, 2022.
Copy Citation
Spinal fractures represent a category of traumatic lesions with a significant impact both medical and social aspects of life. Within this category, thoracolumbar fractures (TLF) form a particular subcategory due to their location with specific biomechanics—the transition from thoracic physiologic kyphosis (fixed) to lumbar lordosis (mobile). Lesions at this level may have severe consequences such as complete/partial motor deficit, local pain or kyphosis.
thoracolumbar
fractures
classification
1. Introduction
Spinal fractures represent a category of traumatic lesions with a significant impact both medical and social aspects of life. Within this category, thoracolumbar fractures (TLF) form a particular subcategory due to their location with specific biomechanics—the transition from thoracic physiologic kyphosis (fixed) to lumbar lordosis (mobile) [1]. Lesions at this level may have severe consequences such as complete/partial motor deficit, local pain or kyphosis [2].
The incidence of thoracolumbar traumatic lesions is variable dependent on the region and country and the number of cases ranges between 6.4 and 11.7/million/year in the United States [3] and 2.4/million/year in China [4], with a global incidence of 3/million/year, including osteoporotic fractures [5]. Within spinal fractures, thoracolumbar localization is present in more than half of the cases (58%) [6]. The most common localization is L1, followed by T12 and L2 [7]. Neurologic deficit (AIS A–AIS D) affects between 25–45% of the cases and 54% [6][7]. More importantly, the treatment of these fractures is still the subject of much controversy. There are three issues that have not yet found a definitive solution which are as follows: 1—a reliable classification/scale, 2—the best surgical approach [8].
In 2002, Mirza et al. defined the ideal criteria that have to be fulfilled in the classification of traumatic spinal lesions [9]. According to them, the terminology has to be clear, comprehensive, concise and descriptive, so as to clearly define each category; the lesion has to be described in terms of pathogeny and biomechanics (mechanism), to precisely indicate the severity and to guide the treatment; lesion characteristics have to defined both in terms of clinical and radiologic elements; the neurology has to be defined in terms of etiology, severity and manifestations; lesion morphology scaling has to take into account the severity of bony and ligamentous lesions, prognostic predictors, including natural history, treatment type and results, deformity risk and additional neurological deficits, to provide useful elements for future research.
Historically, multiple classifications and scales have been devised in order to optimally define the lesions as well as the treatment options. These systems evolved over time, considering not only the morphology of the lesion and mechanisms but also stability, neurology and PLC integrity.
In 2010, van Middendorp et.al. describe the ideal characteristics of a classification system for spinal traumatic lesions [10]. Ideal properties of spinal injury classification categories are, according to them, as follows: (1) clear definitions without ambiguity or freedom of interpretation; (2) all-inclusive and mutually exclusive; (3) clearly distinguishable representative graphic illustrations; (4) straightforward and practicable for daily use; (5) limited number of categories; (6) characterized by increasing grades of severity; (7) each (sub)category alphanumerically coded; (8) injury characteristics easily discernable on diagnostic images [10].
2. Bohler Classification
The first classification of thoracolumbar traumatic lesions belongs to Bohler in 1930 [11]. In his classification he introduced lesion mechanism and morphology, describing 5 categories: compression fracture, flexion distraction injury (compression injury to the vertebral body and distraction injury to the posterior element), extension injury, shear fracture, and rotational injuries. He made no attempt to define spinal instability based on lesion morphology [12].
Sethi et.al., 2009, when looking at the existent classifications analyses, studied the Boehler classification and concluded that it is simple, easily usable, yet very descriptive, outdated, unvalidated, and cannot be predictive of outcome [13]. The same paper also evaluates other less used classifications, such as the Watson–Jones classification and the Nicoll, McAffee, Ferguson and Allen classifications [14][15][16][17]. Although these are considered simple and easy to use in practice, they are as a general rule not validated, they do not predict the outcome and as a result are not commonly used.
3. The Load Sharing Classification (LSC) of Spine Fractures
A classification based on a quantitative point system, The Load Sharing Classification (LSC) of Spine Fractures was published by McCormack and Gaines in 1994 [18]. This classification appeared as a result of the increasingly extensive use of pedicular screws, a technique described and used by Roy Camille, initially in spine fractures, then in other types of spinal pathologies [19][20][21][22][23]. The authors documented in certain cases the failure of short segment pedicular screws SSPS instrumentation systems—of one level above, or one level below—used for the treatment of three-columns fractures and fractures–dislocations in the thoracic and thoracolumbar areas, leading to kyphosis. This classification evaluates, based on a quantitative point system, the following elements: (1) the degree of kyphosis correction on lateral view, (2) degree of vertebral body comminution, (3) the apposition of the fracture fragment. Each element can be evaluated with 1 to 3 points, leading to an overall score of 3 to 9. As the score increases, the anterior support is more severely affected. SPSS is indicated for a score of 6 or lower. For a score greater or equal to 7, without dislocation (severe burst fractures) short-segment anterior corpectomy, strut-graft fusion and instrumentation is indicated. If dislocation is also present then, for the same score of 7 or greater, SPSS followed by an anterior approach (circumferential, 360 degrees) is indicated. Alternatively, LSPS (8 screws) can be used with the downside of supplemental mobility impairment. The authors underline from the beginning a couple of disadvantages of their classification such as a lack of evaluation of the mechanism of injury, ligament integrity, which in turn makes this score unusable for surgical decision making (the evaluation of the ligamentous system is essential in therapeutical decision). In conclusion, this classification is useful in making the choice between SSPS or LSPS, as well as the anterior approach (Figure 1).
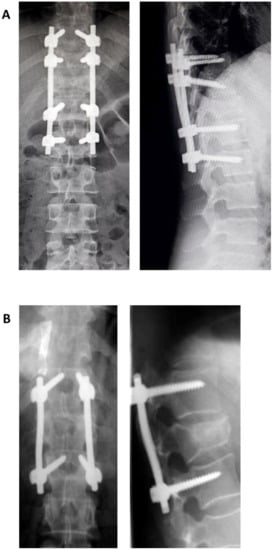
Figure 1. Postoperative X-ray showing a long segment pedicular screws (A) and short segment pedicular screws (B).
Sethi et.al. advance the opinion that the Load Sharing Classification method of McCormack is simple, predicts the outcome of short instrumentation, but is not validated, and does not evaluate neurology and stability [13]. Radcliff et.al. conclude that the Load Sharing Score (LSS) cannot be used alone for surgical decision making for thoracolumbar fractures in the absence of a significant correlation between the neurological status and ligament integrity [14]. This caveat can lead to an incorrect choice of treatment, a low interobserver reliability for the proposed surgical treatment threshold score of 6, which may hinder communication and the continuity of care among providers, and surgical decision making at a score greater than 6 it is not reproducible, sensitive and specific.
Even more, both surgical techniques as well as instrumentation systems have evolved significantly in recent decades and, as a result, the LSS should be used carefully [15]. Stam et.al. in their systematic literature review published in 2020 conclude that, although an LSS equal or greater than 7 requires the reconstruction of anterior spinal support with or without SSPS, SSPS alone is sufficient and safe in these cases [16]. As a result, LSS loses its predictive value when faced with sagittal and posterior instrumentation failure.
In spite of all the above-mentioned disadvantages, LSS is valuable with regard to the issue of anterior vertebral support, taking into account the comminution and fragments apposition. These elements represent red flags for possible lesion progression towards chronic pain and segmental kyphosis, especially in cases treated conservatively.
4. Introduction of Columnar Concepts
A critical landmark in the evolution of thoracolumbar lesions classification was the introduction of the columnar concept. It was introduced in 1963 by Holdsworth as the “Two Column Concept” [17]. The author defined two parts for the spinal column, namely the anterior column consisting of the vertebral body, intervertebral disk and anterior and posterior ligaments, and the posterior column consisting of the pedicles, joint process, transverse apophysis, yellow ligament, spinous process and supra and interspinous ligaments. Column stability depends on the posterior column. This is the first instance that the role of PLC in column stability is noticed. Traumatic lesions are therefore split in stable—wedge compression fracture, burst fracture and unstable dislocations, i.e., extension fractures and dislocations rotational fracture-dislocation. The latter are produced through the following mechanisms: flexion, flexion-rotation, extension, extension-compression and translation. It is a classification that takes into account traumatic mechanisms and lesion morphology.
In 1983, Denis described the three columns system, which divides the Holdsworth anterior column in two, resulting a middle column which consists of the posterior half of the vertebral body, intervertebral disk and PCL (Figure 2). The middle column allows for a good differentiation between compression fractures that affect only the anterior column and burst fractures that involve both anterior and middle columns. Denis classifies thoracolumbar lesions as minor lesions—lesions of the transverse apophysis, spinous process, and isthmus (pars interarticularis) and major lesions—compression fracture, burst fracture, flexion-distraction injury (seat-belt injury), and fracture-dislocation [24]. Lesions are considered unstable if at least two columns are involved (e.g., a compression fracture with comminution is stable; a burst fracture with comminution produced by axial loading and compression of the vertebral body is unstable; the seat belt fracture that is the result of flexion and involves all three columns is unstable; a luxating fracture that involves all three columns and is a result of complex mechanisms of compression and rotation, is unstable). This classification has a series of disadvantages [25]. It does not evaluate the status of PCL that can lead over time at progressive instability, classifies all comminutive fractures as unstable (two columns involved), overlooks the neurology and provides no treatment guidelines.
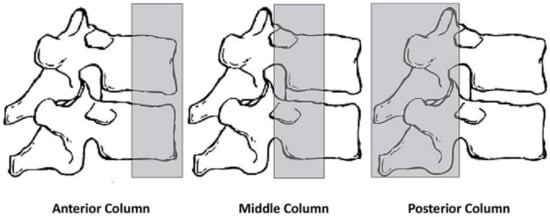
Figure 2. Schematic representation of Denis’ three column concept.
5. Magerl Classification
Magerl et.al. described, in 1994, a new comprehensive classification for thoracolumbar fractures, the AO (Arbeitsgemeinschaft für Osteosynthesefragen) Classification or Magerl Classification, drawing on a study of 1445 fractures over a period of 10 years [26]. This is again a bi-columnar classification and is based on the radiographic morphology of the lesions (Rx and CT) as well as mechanism (compression, distraction, and axial torque). This classification uses a numeric system (3-3-3) and distinguishes three types of lesions referred to as A, B, and C. These are further divided, based on morphological criteria, into three groups which, in turn, have each a series of three sub-groups, adding supplementary specifications. Lesion severity and subsequently, the instability grow from A to C and from 1 to 3. Type A are compression fractures of the vertebral body without PLL involvement, which are stable or partially unstable. Type B are anterior and posterior element injuries with distraction. Comprising, as a rule, disk and ligamentous lesions, they have a surgical indication due to their poor healing potential. Type C anterior and posterior element injuries with rotation are unstable and require surgical treatment.
Sethi et al. consider the Magerl Classification method to be comprehensive. It is based on morphologic aspects, defining severity and instability, but is too complex, has moderate reliability and does not take into account the neurological deficit [13]. Furthermore, although it discusses instability, its definition is not clear, and almost all lesions have a degree of instability. Indeed, as a classification with 53 subtypes that is extremely detailed, with elements that are at times difficult to differentiate, makes its use in daily clinical practice quite difficult.
The reproducibility and reliability of Magerl Classification are not very high. If the lesions type and subtypes are considered, the interobserver agreement is fair (k = 0.32), also the intraobserver is also fair (k = 0.38) [27].
References
- Om, C. Epidemiology of acute thoracolumbar fractures of youngadults in Hong Kong. Hong Kong J. Orthop. Surg. 2001, 5, 40–46.
- Sharif, S.; Shaikh, Y.; Yaman, O.; Zileli, M. Surgical Techniques for Thoracolumbar Spine Fractures: WFNS Spine Committee Recommendations. Neurospine 2021, 18, 667–680.
- Hu, R.; Mustard, C.A.; Burns, C. Epidemiology of incident spinal fracture in a complete population. Spine 1996, 21, 492–499.
- Li, B.; Sun, C.; Zhao, C.; Yao, X.; Zhang, Y.; Duan, H.; Hao, J.; Guo, X.; Fan, B.; Ning, G.; et al. Epidemiological profile of thoracolumbar fracture (TLF) over a period of 10 years in Tianjin, China. J. Spinal Cord. Med. 2019, 42, 178–183.
- Zileli, M.; Sharif, S.; Fornari, M. Incidence and Epidemiology of Thoracolumbar Spine Fractures: WFNS Spine Committee Recommendations. Neurospine 2021, 18, 704–712.
- Leucht, P.; Fischer, K.; Muhr, G.; Mueller, E.J. Epidemiology of traumatic spine fractures. Injury 2009, 40, 166–172.
- Wang, H.; Zhang, Y.; Xiang, Q.; Wang, X.; Li, C.; Xiong, H.; Zhou, Y. Epidemiology of traumatic spinal fractures: Experience from medical university-affiliated hospitals in Chongqing, China, 2001–2010. J. Neurosurg. Spine 2012, 17, 459–468.
- Ramírez-Villaescusa, J.; Hidalgo, J.L.; Ruiz-Picazo, D.; Martin-Benlloch, A.; Torres-Lozano, P.; Portero-Martinez, E. The impact of urgent intervention on the neurologic recovery in patients with thoracolumbar fractures. J. Spine Surg. 2018, 4, 388–396.
- Mirza, S.K.; Mirza, A.J.; Chapman, J.R.; Anderson, P.A. Classifications of thoracic and lumbar fractures: Rationale and supporting data. J. Am. Acad. Orthop. Surg. 2002, 10, 364–377.
- Van Middendorp, J.J.; Audigé, L.; Hanson, B.; Chapman, J.R.; Hosman, A.J. What should an ideal spinal injury classification system consist of? A methodological review and conceptual proposal for future classifications. Eur. Spine J. 2010, 19, 1238–1249.
- Boehler, L. Die Techniek der Knochenbruchbehandlung Im Grieden und Im Kriege; Verlag von Wilheim Maudrich: Vienna, Austria, 1930.
- Bohler, L. The Treatment of Fractures, 5th ed.; Grune & Stratton: New York, NY, USA, 1956; pp. 300–329.
- Sethi, M.K.; Schoenfeld, A.J.; Bono, C.M.; Harris, M.B. The evolution of thoracolumbar injury classification systems. Spine J. 2009, 9, 780–788.
- Radcliff, K.; Kepler, C.K.; Rubin, T.A.; Maaieh, M.; Hilibrand, A.S.; Harrop, J.; Rihn, J.A.; Albert, T.J.; Vaccaro, A.R. Does the Load-Sharing Classification Predict Ligamentous Injury, Neurological Injury, and the Need for Surgery in Patients with Thoracolumbar Burst Fractures? J. Neurosurg. Spine 2012, 16, 534–538.
- Wang, H.; Jiang, J. How to use the load-sharing classification of spine fractures? Eur. Spine J. 2014, 24, 406–407.
- Stam, W.T.; Deunk, J.; Elzinga, M.J.; Bloemers, F.W.; Giannakopoulos, G.F. The Predictive Value of the Load Sharing Classification Concerning Sagittal Collapse and Posterior Instrumentation Failure: A Systematic Literature Review. Glob. Spine J. 2020, 10, 486–492.
- Holdsworth, F.W. Fractures, dislocations, and fractures-dislocations of the spine. J. Bone Joint Surg. 1963, 45B, 6–20.
- McCormack, T.; Karaikovic, E.; Gaines, R.W. The Load Sharing Classification of Spine Fractures. Spine 1994, 19, 1741–1744.
- Roy-Camille, R.; Demeulenaere, C. Osteosynthese du rachis dorsal, lombaire et lombosacree par plaque metalliques vissees dans les pedicles vertebraux et les apophyses articulaires. Presse Med. 1970, 78, 1447–1448.
- Roy-Camille, R.; Saillant, G.; Berteaux, D.; Salgodo, V. Osteosynthesis of thoracolumbar spine fractures with metal plates screwed through the vertebral pedicles. Reconstr. Surg. Traumatol. 1976, 15, 2.
- Roy-Camille, R.; Saillant, G.; Bisserie, M. Surgical treatment of spinal metastatic tumors by posterior plating and laminectomy. In Proceedings of the 51st Annual Meeting of the American Academy of Orthopaedic Surgeons, Atlanta, GA, USA, 9 February 1984.
- Roy-Camille, R.; Saillant, G.; Lapresle, P.; Mazel, C. A secret in spine surgery: The pedicle. In Proceedings of the 51st Annual Meeting of the American Academy of Orthopaedic Surgeons, Atlanta, GA, USA, 9 February 1984.
- Roy-Camille, R.; Saillant, G.; Mazel, C. Internal fixation of the lumbar spine with pedicle screw plating. Clin. Orthop. Rel. Res. 1986, 203, 7–17.
- Denis, F. The three column spine and its significance in the classification of acute thoracolumbar spine injuries. Spine 1983, 8, 817–831.
- Prajapati, H.P.; Kumar, R. Thoracolumbar fracture classification: Evolution, merits, demerits, updates, and concept of stability. Br. J. Neurosurg. 2021, 35, 92–97.
- Magerl, F.; Aebi, M.; Gertzbein, S.D.; Harms, J.; Nazarian, S. A comprehensive classification of thoracic and lumbar injuries. Eur. Spine J. 1994, 3, 184–201.
- Lopes, F.; Ferreira, A.; Santos, R.; Maçaneiro, C.H. Intraobserver and interobserver reproducibility of the old and new classifications of toracolombar fractures. Rev. Bras. Ortop. 2018, 53, 521–526.
More
Information
Subjects:
Orthopedics
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
700
Revisions:
3 times
(View History)
Update Date:
30 May 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




