
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | GIANMARCO ANNIBALI | -- | 2117 | 2022-04-28 14:59:16 | | | |
| 2 | Peter Tang | Meta information modification | 2117 | 2022-04-29 08:12:45 | | |
Video Upload Options
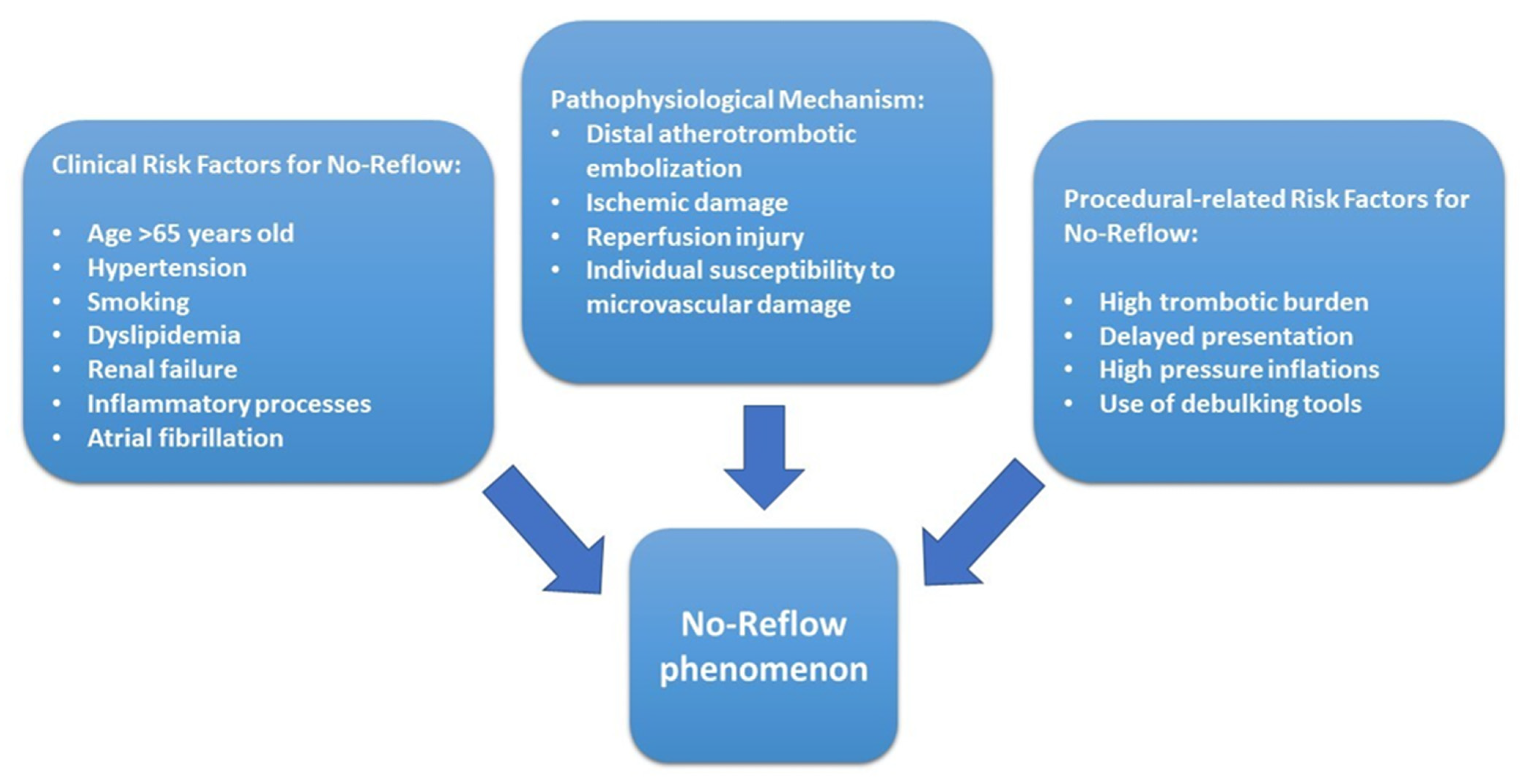
Primary percutaneous angioplasty (pPCI), represents the reperfusion strategy of choice for patients with STEMI according to current international guidelines of the European Society of Cardiology. Coronary no-reflow is characterized by angiographic evidence of slow or no anterograde epicardial flow, resulting in inadequate myocardial perfusion in the absence of evidence of mechanical vessel obstruction. No reflow (NR) is related to a functional and structural alteration of the coronary microcirculation.
1. Introduction
2. Pathophysiological Mechanisms
3. Diagnosis of No-Reflow
|
Diagnostic Methods |
Study Design |
Results |
Limitations |
|---|---|---|---|
|
Coronary Angiography (MBG) [42] |
777 prospectively enrolled patients who underwent pPCI during a 6-year period. |
MBG can be used to describe the effectiveness of myocardial reperfusion and is an independent predictor of long-term mortality. |
Interobserver and intraobserver variabilities associated with subjective angiographic assessments. |
|
Coronary Flow Reserve (CFR) [43] |
89 prospectively enrolled patients who underwent pPCI during a 4-year period and subsequent physiologic study. |
A CFR value ≥ 2.0 is considered normal. Complimentary assessment of microcirculation by the IMR and CFR may be useful to evaluate myocardial viability and predict the long-term prognosis of STEMI patients. |
Possible significant variability of tracings between different beats. Does not distinguish between epicardial and microvascular components of coronary resistances. Requires maximal hyperemia using adenosine. |
|
Microvascular resistance index (IMR) [44] |
288 prospectively enrolled patients with STEMI during a 11-year period. |
An IMR > 40 is a multivariable associate of left ventricular and clinical outcomes after STEMI, regardless of infarct size. IMR has superior clinical value for risk stratification. |
Manual injection of saline may be a source of variability. It requires achievement of maximal hyperemia and the use of adenosine. |
|
Electrocardiogram (ECG) [36] |
180 prospectively enrolled patients with a first acute STEMI. |
Residual ST-segment elevation and the number of Q waves on the ECG shortly after pPCI have complementary predictive value on myocardial function, infarct size and extent, and MVO. |
Discordance between resolution of ST-segment elevation and the angiographic indices of NR. |
|
Myocardial Contrast Echocardiography (MCE) [40] |
110 prospectively enrolled patients who underwent pPCI in a multicenter study. |
Among patients with TIMI 3 flow, MVO extension, as detected and quantified by MCE, is the most powerful independent predictor of LV remodeling after STEMI compared with persistent ST-segment elevation and degree of MBG. |
Operator-dependent and limited by the possible poor acoustic window. |
|
Cardiac Magnetic Resonance (CMR) [6] |
Pooled analysis using individual patient data from seven randomized primary PCI trials |
The presence and extent of MVO measured by CMR after primary PCI in STEMI are strongly associated with mortality and hospitalization for HF within 1 year. |
Usually performed 2 to 7 days after pPCI. Not widely available locally. Not performable in all patients. |
|
Positron Emission Tomography (PET) [37] |
Seven porcine model with left anterior descending coronary artery occlusion/reperfusion underwent PET-CT within 3 days of infarction. |
Increased regional FDG uptake in the area of acute infarction is a frequent occurrence and indicates tissue inflammation that is commonly associated with MVO. |
Expensive and difficult to obtain locally. |
pPCI, Primary Percutaneous Coronary Intervention; MBG, Myocardial Blush Grade; STEMI, ST-Elevation Myocardial Infarction; NR, No-Reflow; CMR, Cardiac Magnetic Resonance; MCE, Myocardial Contrast Echocardiography; TIMI, Thrombolysis in Myocardial Infarction; MVO, Microvascular Obstruction; LV, Left Ventricular; HF, Heart Failure; PET, Positron Emission Tomography; PET-CT, Positron Emission Tomography/Computed Tomography; and FDG, 2-Deoxy-2-[18F]Fluoro-d-Glucose.
4. Management of No-Reflow
References
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur. Heart J. 2018, 39, 119–177.
- TIMI Study Group. The Thrombolysis in Myocardial Infarction (TIMI) trial. Phase I findings. N. Engl. J. Med. 1985, 312, 932–936.
- Niccoli, G.; Kharbanda, R.K.; Crea, F.; Banning, A.P. No-reflow: Again prevention is better than treatment. Eur. Heart J. 2010, 31, 2449–2455.
- Tasar, O.; Karabay, A.K.; Oduncu, V.; Kirma, C. Predictors and outcomes of no-reflow phenomenon in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Coron. Artery Dis. 2019, 30, 270–276.
- Niccoli, G.; Burzotta, F.; Galiuto, L.; Crea, F. Myocardial no-reflow in humans. J. Am. Coll. Cardiol. 2009, 54, 281–292.
- De Waha, S.; Patel, M.R.; Granger, C.B.; Ohman, E.M.; Maehara, A.; Eitel, I.; Ben-Yehuda, O.; Jenkins, P.; Thiele, H.; Stone, G.W. Relationship between microvascular obstruction and adverse events following primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: An individual patient data pooled analysis from seven randomized trials. Eur. Heart J. 2017, 38, 3502–3510.
- Caiazzo, G.; Musci, R.L.; Frediani, L.; Umińska, J.; Wanha, W.; Filipiak, K.J.; Kubica, J.; Navarese, E.P. State of the Art: No-Reflow Phenomenon. Cardiol. Clin. 2020, 38, 563–573.
- Kaur, G.; Baghdasaryan, P.; Natarajan, B.; Sethi, P.; Mukherjee, A.; Varadarajan, P.; Pai, R.G. Pathophysiology, Diagnosis, and Management of Coronary No-Reflow Phenomenon. Int. J. Angiol. 2021, 30, 15–21.
- Montone, R.A.; Camilli, M.; Del Buono, M.G.; Meucci, M.C.; Gurgoglione, F.; Russo, M.; Crea, F.; Niccoli, G. “No-reflow”: Update su diagnosi, fisiopatologia e strategie terapeutiche. G. Ital. Cardiol. 2020, 21, 4S–14S.
- Porto, I.; Biasucci, L.M.; De Maria, G.L.; Leone, A.M.; Niccoli, G.; Burzotta, F.; Trani, C.; Tritarelli, A.; Vergallo, R.; Liuzzo, G.; et al. Intracoronary microparticles and microvascular obstruction in patients with ST elevation myocardial infarction undergoing primary percutaneous intervention. Eur. Heart J. 2012, 33, 2928–2938.
- Heusch, G.; Kleinbongard, P.; Böse, D.; Levkau, B.; Haude, M.; Schulz, R.; Erbel, R. Coronary microembolization: From bedside to bench and back to bedside. Circulation 2009, 120, 1822–1836.
- Weis, S.M.; Cheresh, D.A. Pathophysiological consequences of VEGF-induced vascular permeability. Nature 2005, 437, 497–504.
- Bouleti, C.; Mewton, N.; Germain, S. The no-reflow phenomenon: State of the art. Arch. Cardiovasc. Dis. 2015, 108, 661–674.
- Ambrosio, G.; Tritto, I. Reperfusion injury: Experimental evidence and clinical implications. Am. Heart J. 1999, 138, S69–S75.
- Fröhlich, G.M.; Meier, P.; White, S.K.; Yellon, D.M.; Hausenloy, D.J. Myocardial reperfusion injury: Looking beyond primary PCI. Eur. Heart J. 2013, 34, 1714–1722.
- Riksen, N.P.; Franke, B.; van den Broek, P.; Smits, P.; Rongen, G.A. The 1976C>T polymorphism in the adenosine A2A receptor gene does not affect the vasodilator response to adenosine in humans in vivo. Pharmacogenet. Genom. 2007, 17, 551–554.
- Kloner, R.A.; King, K.S.; Harrington, M.G. No-reflow phenomenon in the heart and brain. Am. J. Physiol. Heart Circ. Physiol. 2018, 315, H550–H562.
- Gibson, C.M.; Cannon, C.P.; Daley, W.L.; Dodge, J.T.; Alexander, B.; Marble, S.J.; McCabe, C.H.; Raymond, L.; Fortin, T.; Poole, W.K.; et al. TIMI frame count: A quantitative method of assessing coronary artery flow. Circulation 1996, 93, 879–888.
- Van ’t Hof, A.W.; Liem, A.; Suryapranata, H.; Hoorntje, J.C.; de Boer, M.J.; Zijlstra, F. Angiographic assessment of myocardial reperfusion in patients treated with primary angioplasty for acute myocardial infarction: Myocardial blush grade. Zwolle Myocardial Infarction Study Group. Circulation 1998, 97, 2302–2306.
- Bulluck, H.; Foin, N.; Tan, J.W.; Low, A.F.; Sezer, M.; Hausenloy, D.J. Invasive Assessment of the Coronary Microcirculation in Reperfused ST-Segment-Elevation Myocardial Infarction Patients: Where Do We Stand? Circ. Cardiovasc. Interv. 2017, 10, e004373.
- Knaapen, P.; Camici, P.G.; Marques, K.M.; Nijveldt, R.; Bax, J.J.; Westerhof, N.; Götte, M.J.W.; Jerosch-Herold, M.; Schelbert, H.R.; Lammertsma, A.A.; et al. Coronary microvascular resistance: Methods for its quantification in humans. Basic Res. Cardiol. 2009, 104, 485–498.
- Fearon, W.F.; Low, A.F.; Yong, A.S.; McGeoch, R.; Berry, C.; Shah, M.G.; Ho, M.Y.; Kim, H.-S.; Loh, J.P.; Oldroyd, K.G. Prognostic value of the Index of Microcirculatory Resistance measured after primary percutaneous coronary intervention. Circulation 2013, 127, 2436–2441.
- Fahrni, G.; Wolfrum, M.; De Maria, G.L.; Cuculi, F.; Dawkins, S.; Alkhalil, M.; Patel, N.; Forfar, J.C.; Prendergast, B.D.; Choudhury, R.P.; et al. Index of Microcirculatory Resistance at the Time of Primary Percutaneous Coronary Intervention Predicts Early Cardiac Complications: Insights From the OxAMI (Oxford Study in Acute Myocardial Infarction) Cohort. J. Am. Heart Assoc. 2017, 6, e005409.
- Fearon, W.F.; Balsam, L.B.; Farouque, H.M.O.; Caffarelli, A.D.; Robbins, R.C.; Fitzgerald, P.J.; Yock, P.G.; Yeung, A.C. Novel index for invasively assessing the coronary microcirculation. Circulation 2003, 107, 3129–3132.
- De Maria, G.L.; Scarsini, R.; Shanmuganathan, M.; Kotronias, R.A.; Terentes-Printzios, D.; Borlotti, A.; Langrish, J.P.; Lucking, A.J.; Choudhury, R.P.; Kharbanda, R.; et al. Angiography-derived index of microcirculatory resistance as a novel, pressure-wire-free tool to assess coronary microcirculation in ST elevation myocardial infarction. Int. J. Cardiovasc. Imaging 2020, 36, 1395–1406.
- Ciofani, J.L.; Allahwala, U.K.; Scarsini, R.; Ekmejian, A.; Banning, A.P.; Bhindi, R.; De Maria, G.L. No-reflow phenomenon in ST-segment elevation myocardial infarction: Still the Achilles’ heel of the interventionalist. Future Cardiol. 2021, 17, 383–397.
- Gragnano, F. Microvascular Obstruction Treatment Efficacy Measured Using Dynamic Microvascular Resistance (dMVR): First-in-Man Study Diagnosis Sequence Patient Cohort, EuroPCR e-Course, Paris 2020. Available online: https://media.pcronline.com/diapos/PCReCourse2020/226-20200627_0900_Hotline_and_Innovation_Channel_Gragnano_Felice_0000_ (accessed on 25 June 2020).
- Lima, J.A.; Judd, R.M.; Bazille, A.; Schulman, S.P.; Atalar, E.; Zerhouni, E.A. Regional heterogeneity of human myocardial infarcts demonstrated by contrast-enhanced MRI. Potential mechanisms. Circulation 1995, 92, 1117–1125.
- Wu, K.C.; Kim, R.J.; Bluemke, D.A.; Rochitte, C.E.; Zerhouni, E.A.; Becker, L.C.; Lima, J.A. Quantification and time course of microvascular obstruction by contrast-enhanced echocardiography and magnetic resonance imaging following acute myocardial infarction and reperfusion. J. Am. Coll. Cardiol. 1998, 32, 1756–1764.
- Ganame, J.; Messalli, G.; Dymarkowski, S.; Rademakers, F.E.; Desmet, W.; Van de Werf, F.; Bogaert, J. Impact of myocardial haemorrhage on left ventricular function and remodelling in patients with reperfused acute myocardial infarction. Eur. Heart J. 2009, 30, 1440–1449.
- Zia, M.I.; Ghugre, N.R.; Connelly, K.A.; Strauss, B.H.; Sparkes, J.D.; Dick, A.J.; Wright, G.A. Characterizing myocardial edema and hemorrhage using quantitative T2 and T2* mapping at multiple time intervals post ST-segment elevation myocardial infarction. Circ. Cardiovasc. Imaging 2012, 5, 566–572.
- García-Dorado, D.; Oliveras, J.; Gili, J.; Sanz, E.; Pérez-Villa, F.; Barrabés, J.; Carreras, M.J.; Solares, J.; Soler-Soler, J. Analysis of myocardial oedema by magnetic resonance imaging early after coronary artery occlusion with or without reperfusion. Cardiovasc. Res. 1993, 27, 1462–1469.
- Croisille, P.; Revel, D.; Saeed, M. Contrast agents and cardiac MR imaging of myocardial ischemia: From bench to bedside. Eur. Radiol. 2006, 16, 1951–1963.
- Bulluck, H.; Dharmakumar, R.; Arai, A.E.; Berry, C.; Hausenloy, D.J. Cardiovascular Magnetic Resonance in Acute ST-Segment-Elevation Myocardial Infarction: Recent Advances, Controversies, and Future Directions. Circulation 2018, 137, 1949–1964.
- Tjandrawidjaja, M.C.; Fu, Y.; Westerhout, C.M.; White, H.D.; Todaro, T.G.; Van de Werf, F.; Mahaffey, K.W.; Wagner, G.S.; Granger, C.B.; Armstrong, P.W.; et al. Resolution of ST-segment depression: A new prognostic marker in ST-segment elevation myocardial infarction. Eur. Heart J. 2010, 31, 573–581.
- Nijveldt, R.; van der Vleuten, P.A.; Hirsch, A.; Beek, A.M.; Tio, R.A.; Tijssen, J.G.P.; Piek, J.J.; van Rossum, A.C.; Zijlstra, F. Early electrocardiographic findings and MR imaging-verified microvascular injury and myocardial infarct size. JACC Cardiovasc. Imaging 2009, 2, 1187–1194.
- Lautamäki, R.; Schuleri, K.H.; Sasano, T.; Javadi, M.S.; Youssef, A.; Merrill, J.; Nekolla, S.G.; Abraham, M.R.; Lardo, A.C.; Bengel, F.M. Integration of infarct size, tissue perfusion, and metabolism by hybrid cardiac positron emission tomography/computed tomography: Evaluation in a porcine model of myocardial infarction. Circ. Cardiovasc. Imaging 2009, 2, 299–305.
- Porter, T.R.; Li, S.; Oster, R.; Deligonul, U. The clinical implications of no reflow demonstrated with intravenous perfluorocarbon containing microbubbles following restoration of Thrombolysis in Myocardial Infarction (TIMI) 3 flow in patients with acute myocardial infarction. Am. J. Cardiol. 1998, 82, 1173–1177.
- Kaul, S. Myocardial contrast echocardiography: A 25-year retrospective. Circulation 2008, 118, 291–308.
- Galiuto, L.; Garramone, B.; Scarà, A.; Rebuzzi, A.G.; Crea, F.; La Torre, G.; Funaro, S.; Madonna, M.; Fedele, F.; Agati, L.; et al. The extent of microvascular damage during myocardial contrast echocardiography is superior to other known indexes of post-infarct reperfusion in predicting left ventricular remodeling: Results of the multicenter AMICI study. J. Am. Coll. Cardiol. 2008, 51, 552–559.
- Niccoli, G.; Scalone, G.; Lerman, A.; Crea, F. Coronary microvascular obstruction in acute myocardial infarction. Eur. Heart J. 2016, 37, 1024–1033.
- Van’t Hof, A.W.J.; Ten Berg, J.; Heestermans, T.; Dill, T.; Funck, R.C.; van Werkum, W.; Dambrink, J.-H.E.; Suryapranata, H.; van Houwelingen, G.; Ottervanger, J.P.; et al. Prehospital initiation of tirofiban in patients with ST-elevation myocardial infarction undergoing primary angioplasty (On-TIME 2): A multicentre, double-blind, randomised controlled trial. Lancet Lond. Engl. 2008, 372, 537–546.
- Park, S.-D.; Baek, Y.-S.; Lee, M.-J.; Kwon, S.W.; Shin, S.-H.; Woo, S.-I.; Kim, D.-H.; Kwan, J.; Park, K.-S. Comprehensive assessment of microcirculation after primary percutaneous intervention in ST-segment elevation myocardial infarction: Insight from thermodilution-derived index of microcirculatory resistance and coronary flow reserve. Coron. Artery Dis. 2016, 27, 34–39.
- Carrick, D.; Haig, C.; Ahmed, N.; Carberry, J.; Yue May, V.T.; McEntegart, M.; Petrie, M.C.; Eteiba, H.; Lindsay, M.; Hood, S.; et al. Comparative Prognostic Utility of Indexes of Microvascular Function Alone or in Combination in Patients With an Acute ST-Segment-Elevation Myocardial Infarction. Circulation 2016, 134, 1833–1847.
- Faruk Akturk, I.; Arif Yalcin, A.; Biyik, I.; Sarikamis, C.; Turhan Caglar, N.; Erturk, M.; Celik, O.; Uzun, F.; Murat Caglar, I.; Oner, E. Effects of verapamil and adenosine in an adjunct to tirofiban on resolution and prognosis of noreflow phenomenon in patients with acute myocardial infarction. Minerva Cardioangiol. 2014, 62, 389–397.




