Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Fatih Yalcin | -- | 1423 | 2022-04-14 03:52:08 | | | |
| 2 | Amina Yu | -51 word(s) | 1372 | 2022-04-14 04:07:02 | | | | |
| 3 | Amina Yu | + 2 word(s) | 1374 | 2022-04-18 07:46:00 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Yalcin, F.; , .; Kurtul, A.; Peker (Ex Yalcin), H. Basal Septal Hypertrophy. Encyclopedia. Available online: https://encyclopedia.pub/entry/21742 (accessed on 02 March 2026).
Yalcin F, , Kurtul A, Peker (Ex Yalcin) H. Basal Septal Hypertrophy. Encyclopedia. Available at: https://encyclopedia.pub/entry/21742. Accessed March 02, 2026.
Yalcin, Fatih, , Alparslan Kurtul, Hulya Peker (Ex Yalcin). "Basal Septal Hypertrophy" Encyclopedia, https://encyclopedia.pub/entry/21742 (accessed March 02, 2026).
Yalcin, F., , ., Kurtul, A., & Peker (Ex Yalcin), H. (2022, April 14). Basal Septal Hypertrophy. In Encyclopedia. https://encyclopedia.pub/entry/21742
Yalcin, Fatih, et al. "Basal Septal Hypertrophy." Encyclopedia. Web. 14 April, 2022.
Copy Citation
Hypertension plays a dominant role in the development of left ventricular (LV) remodeling and heart failure, in addition to being the main risk factor for coronary artery disease.
basal septal hypertrophy
early imaging biomarker
heart failure
hypertension and stressed heart morphology
1. Basal Septal Hypertrophy and Clinic Observations
It is known that left ventricular (LV) segmental remodeling could be the case in early-stage hypertension described as borderline hypertension, and the septal wall is speculated to be the first LV wall to become hypertrophic in clinical practice according to cross-sectional studies [1][2][3]. Increased myocardial dynamics was suggested to be related to focal hypertrophy. In addition to this non-uniform LV geometry with segmental hypertrophy of septal base (basal septal hypertrophy, BSH), myocardial hypercontractility is determined in imaging reports as a usual finding in the early stage of hypertensive heart disease [4][5]. It was confirmed hyperdynamic septal basal tissue quantitatively by the combined analysis of tissue Doppler imaging and dobutamine stress echocardiography in BSH [6]. However, the determination of hypertension under stress in some symptomatic patients with dyspnea and hyperdynamic function is not recalled during examination and technic analysis [7]. Therefore, It was remarked the importance of investigation for hypertension and technic analysis with ultrasound in symptomatic patients with hyperdynamic LV function [8].
2. BSH and Animal Validation
The earlier ones showed a high heart rate–pressure product and high LV outflow tract blood flow as well as basal septal hyperdynamic tissue under stress in BSH patients with hypertension [6][9][10][11]. These clinic observations possibly represented a compensatory hemodynamic adaptation to increased stress stimuli in this group of patients. Beyond these cross-sectional observations, it was decided to determine the progression of LV segmental remodeling prospectively. It was used treadmill exercise for physiologic and transaortic construction for pathologic stress stimuli and third-generation microscopic ultrasonography in small animals for the determination of segmental LV remodeling evolution. It was noted for the first time that BSH is the early imaging biomarker of LV remodeling under both physiologic and pathologic stress [12]. Nevertheless, since it was detected that BSH development as initial LV remodeling prospectively in an animal model in both physiologic stress-mediated remodeling with normal organization of myocytes and pathologic with myocyte hypertrophy and collagen accumulation, a correct diagnosis for the nature of BSH should be documented by blood pressure (BP) monitorization to explore whether or not pressure-overload is the case.
In the animal validation studies, it was also detected a remarkable velocity increment in the early time points after transaortic construction in pathologic stress, which was consistent with the findings in cross-sectional clinic studies [13]. However, there was a sharp transition in the basal septal tissue function after the initiation of the maladaptive phase of LV remodeling under pathologic stress, while LV function was preserved in animals with physiologic stress. Nevertheless, preserved global LV function at the BSH stage with compensatory tissue hyperfunction prior to maladaptation could lead to a diagnostic difficulty in clinical practice if pressure-overload is not completely eliminated. On the other hand, previous ultrasonographic data regarding BSH in the last two decades [6][9][10][11] have recently been confirmed by cardiac magnetic resonance (CMR) studies in healthy individuals with initial septal remodeling.
Blood pressure (BP) monitorization under stress is insufficient in patients with LV septal hypertrophy during clinical practice. In fact, no attempt was made for BP recording during exercise even in the comprehensively planned cardiac magnetic resonance (CMR) in which physiologic exercise in a healthy population was speculated to be the reason for septal hypertrophy [14]. It was emphasized the importance of BP monitoring in imaging studies on initial septal remodeling, since physiologic septal remodeling cannot be proven without the complete elimination of hemodynamic overload due to increased BP at stress [15]. Furthermore, it has recently considered reportingandon hemodynamic overload using BP recording during exercise in healthy people or even endurance athletes with septal hypertrophy determined using CMR [16] and the importance of BSH as the early imaging biomarker in the prevention of global remodeling by an effective medical management [17].
Striking Difference between Animal and Human BSH Data
BSH plays a role as a common denominator for variety of stress stimuli beyond basic hemodynamic stress-mediated LV remodeling. Due to this complex nature of BSH, it was previously described this morphological finding as the ‘stressed heart morphology’ (SHM), which was documented as an imaging figure in both acute and chronic stress-mediated heart conditions such as acute stress cardiomyopathy [18] and hypertension [17]. Despite the fact that hemodynamic overload seems to be a unique pathophysiologic mechanism for LV global remodeling, the LV base represents an extremely sensitive feature under different types of stress stimuli, since it is associated with predominant sympathetic innervation.
In fact, while a smooth curvature is the case in some patients (Figure 1), another group of hypertensive patients could have extremely predominant BSH without any remodeled segments over the rest of the LV (Figure 2). It has recently been described that the mechanical component of BSH in aortic stenosis (Figure 3) in addition to the other etiologies including emotional in acute stress cardiomyopathy and functional due to an increased afterload in hypertensive patients [19]. All these different mechanisms of stress induction in humans may explain a more complex nature for the development of this morphology. SHM could represent an individually variable heterogenous distribution of myocardial remodeling in humans and this heterogeneity supports the potential influence of additional mental or emotional stress-mediated contributors in humans.
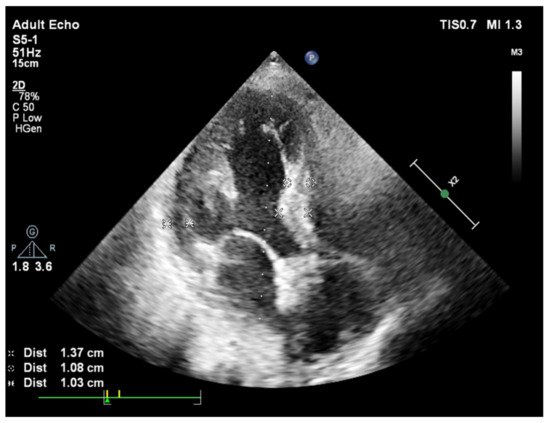
Figure 1. A slight curve of septal base from apical 4 chamber view during end-diastole in a patient with systemic hypertension and basal septal hypertrophy.
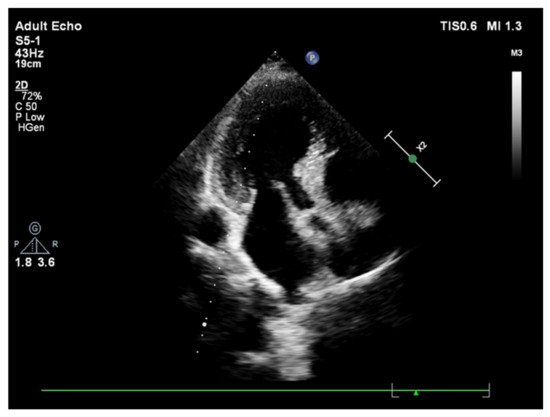
Figure 2. A sharp curvature of more remarkable basal septal hypertrophy from apical 4 chamber view during end-diastole in another hypertensive patient.
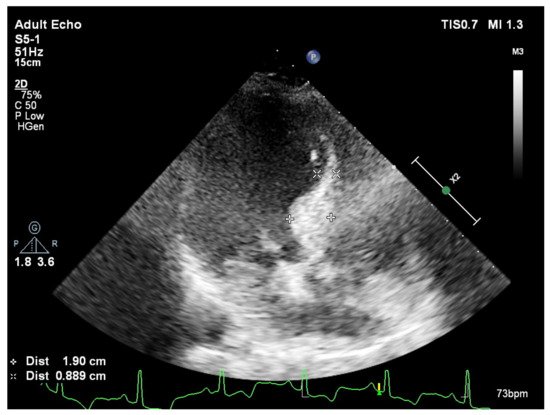
Figure 3. Predominantly placed hypertrophy over septal base from apical 4 chamber view during end-diastole in a patient with aortic stenosis and basal septal hypertrophy.
Sympathetic overdrive more dominantly involves the LV base compared to the midapical myocardial segments. However, despite the fact that it is a potentially possible etiologic mechanism, there has not been any chronic mental or emotional disorder documented or described except acute stress cardiomyopathy in the development of SHM. Heterogeneity involved in remodeling in humans produces a dilemma not only in a certain diagnosis of pure hemodynamic overload-mediated BSH in hypertensive patients, but in the certain determination of BSH prevalence in the population.
On the other hand, years later, It has benn determined that LV segmental remodeling in an animal model that is associated with a very regular distribution (Figure 4a,b) under stress-mediated hemodynamic overload differently from an individually variable heterogeneity and focally predominant BSH in human data. Third-generation microscopic ultrasonography provided a unique opportunity to document the regional evolution of LV remodeling prospectively. Microimaging also confirmed previous cross-sectional clinic studies in hypertension that support BSH as the first remodeled region that was validated as the early imaging biomarker in animal validation studies [12][13]. Recently, it was suggested that scientists should be cautious in the quantification of this morphologic finding, because it is possible to detect an extremely large spectrum of BSH heterogeneity in clinical practice [20][21].
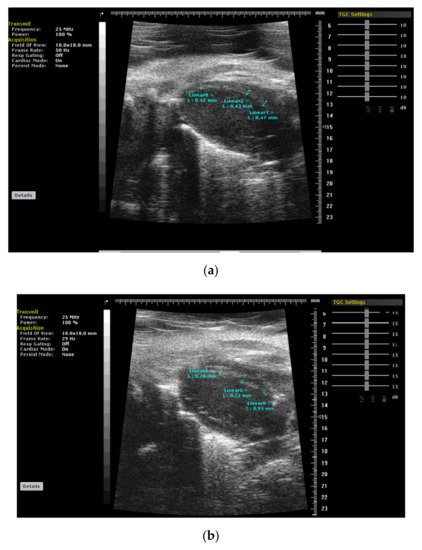
Figure 4. (a,b): Cardiac images of a mice using 3rd generation microscopic ultrasound show normal cardiac geometry and a regularly remodeled septal wall with thickerseptal base at 4 weeks after stress induction due to pressure-overload (TAC: transverse aortic construction), respectively.
3. Heart Failure with Preserved Ejection Fraction
HF with preserved ejection fraction (HFPEF) is a relatively new clinical entity and the number of HFPEF patients is increasing worldwide. As the majority of the HFPEF patients have systemic hypertension, HFPEF is usually accepted as a hypertension-mediated phenomenon. The preserved global systolic function has been documented by freehand three-dimensional echocardiography at rest in HFPEFpatients [22]. However, despite a normal global EF, contractile abnormalities are more common in HFPEF, unlike patients with hypertensive global LV remodeling [23]. It was pointed out the importance of the evaluation of contractile reserve by combined diagnostic techniques with stress induction, which may be beneficial for the monitorization of disease progression from an early to an advanced stage and a more effective treatment of hypertensive heart disease [24]. In fact, fibrotic tissue accumulation progressively decreases diastolic filling and results in impaired LV contractility in HFPEF [25]. As both conditions have preserved global EF at rest, it is crucial to separate hypertensive LV remodeling from the HFPEF. It was pointed out that myocardial fibrosis detected using CMR could be beneficial in the detection of patients with HFPEF [26].
References
- Maron, B.J.; Edwards, J.E.; Epstein, S.E. Disproportionate ventricular septal thickening in patients with systemic hypertension. Chest 1978, 73, 466–470.
- Safar, M.E.; Benessiano, J.R.; Hornych, A.L. Asymmetrical septal hypertrophy and borderline hypertension. Int. J. Cardiol. 1982, 2, 103–108.
- Verdecchia, P.; Porcellati, C.; Zampi, I.; Schillaci, G.; Gatteschi, C.; Battistelli, M.; Bartoccini, C.; Borgioni, C.; Ciucci, A. Asymmetric left ventricular remodelling due to isolated septal thickening in patients with systemic hypertension and normal left ventricular masses. Am. J. Cardiol. 1994, 73, 247–252.
- Lutas, E.M.; Devereux, R.B.; Reis, G.; Alderman, M.H.; Pickering, T.G.; Borer, J.S.; Laragh, J.H. Increased cardiac performance in mild essential hypertension. Left ventricular mechanics. Hypertension 1985, 7, 979–988.
- De Simone, G.; Di Lorenzo, L.; Costantino, G.; Moccia, D.; Buonissimo, S.; de Divitiis, O. Supernormal contractility in primary hypertension without left ventricular hypertrophy. Hypertension 1988, 11, 457–463.
- Yalçin, F.; Yigit, F.; Erol, T.; Baltali, M.; Korkmaz, M.E.; Müderrisoglu, H. Effect of dobutamine stress on basal septal tissue dynamics in hypertensive patients with basal septal hypertrophy. J. Hum. Hypertens. 2006, 20, 628–630.
- Gorantla, R.S.; Ahmed, S.; Voruganti, D.; Menzies, D.J. Hyperdynamic left ventricle on radionuclide myocardial perfusion imaging (RNMPI): A marker of diastolic dysfunction in patients presenting with dyspnea on exertion. Int. J. Cardiol. Heart Vasc. 2015, 9, 43–47.
- Yalçin, F.; Schindler, T.; Abraham, T.P. Hypertension should be ruled out in hyperdynamic left ventricle in radionuclide myocardial perfusion imaging, diastolic dysfunction, dyspnea on exertion. Int. J. Cardiol. Heart Vasc. 2015, 7, 149–150.
- Yalçin, F.; Muderrisoglu, H.; Korkmaz, M.E.; Ozin, B.; Baltali, M.; Yigit, F. The effect of dobutamine stress on left ventricular outflow tract gradients in hypertensive patients with basal septal hypertrophy. Angiology 2004, 55, 295–301.
- Yalçin, F.; Yalçin, H.; SeyfeliEAkgul, F. Stress-induced hypercontractility in patients with hypertension: An interesting imaging finding. Int. J. Cardiol. 2010, 143, E1–E3.
- Yalçin, F.; Yalçin, H.; Abraham, T.P. Stress-induced regional features of left ventricle is related to pathogenesis of clinical conditions with both acute and chronic stress. Int. J. Cardiol. 2010, 145, 367–368.
- Yalçin, F.; Kucukler, N.; Cingolani, O.; Mbiyangandu, B.; Sorensen, L.; Pinherio, A.; Abraham, M.R.; Abraham, T.P. Evolution of ventricular hypertrophy and myocardial mechanics in physiologic and pathologic hypertrophy. J. Appl. Physiol. 2019, 126, 354–362.
- Yalçin, F.; Kucukler, N.; Cingolani, O.; Mbiyangandu, B.; Sorensen, L.; Pinherio, A.; Abraham, M.R.; Abraham, T.P. Intracavitary gradient in mice with early regional remodeling at the compensatory hyperactive stage prior to left ventricular tissue dysfunction. J. Am. Coll. Cardiol. 2020, 75, 1585.
- Lee, P.T.; Dweck, M.R.; Prasher, S.; Shah, A.; Humphries, S.E.; Pennell, D.J.; Montgomery, H.E.; Payne, J.R. Left ventricular wall thickness and the presence of asymmetric hypertrophy in healthy young army recruits: Data from the LARGE heart study. Circ. Cardiovasc. Imaging 2013, 6, 262–267.
- Yalçin, F.; Abraham, T.P.; Gottdiener, J.S. Letter by Yalcin et al. regarding article “Left ventricular wall thickness and the presence of asymmetric hypertrophy in healthy young army recruits: Data from the LARGE heart study”. Circ. Cardiovasc. Imaging 2013, 6, e28.
- Małek, Ł.A.; Czajkowska, A.; Mróz, A.; Witek, K.; Barczuk-Falecka, M.; Nowicki, D.; Postuła, M.; Werys, K. Left ventricular hypertrophy in middle-aged endurance athletes: Is it blood pressure related? Blood Press. Monit. 2019, 24, 110–113.
- Yalçin, F.; Yalçin, H.; Abraham, T.P. Exercise hypertension should be recalled in basal septal hypertrophy as the early imaging biomarker in patients with stressed heart morphology. Blood Press. Monit. 2020, 25, 118–119.
- Yalçin, F.; Muderrisoglu, H. Takotsubo cardiomyopathy may be associated with cardiac geometric features as observed in hypertensive heart disease. Int. J. Cardiol. 2009, 135, 251–252.
- Yalçin, F.; Abraham, M.R.; Abraham, T.P. Myocardial aspects in aortic stenosis and functional increased afterload conditions in patients with stressed heart morphology. Ann. Thorac. Cardiovasc. Surg. 2021, 27, 332–334.
- Marciniak, M.; Gilbert, A.; Loncaric, F.; Fernandes, J.F.; Bijnens, B.; Sitges, M.; King, A.; Crispi, F.; Lamata, P. Septal curvature as a robust and reproducible marker for basal septal hypertrophy. J. Hypertens. 2021, 39, 1421–1428.
- Yalçin, F.; Yalçin, H.; Abraham, M.R.; Abraham, T.P. Basal septal hypertrophy: Extremely sensitive region to variety of stress stimuli and stressed heart morphology. J. Hypertens. 2021, in press.
- Maurer, M.S.; King, D.L.; El-Khoury Rumbarger, L.; Packer, M.; Burkhoff, D. Left heart failure with a normal ejection fraction: Identification of different pathophysiologic mechanisms. J. Card. Fail. 2005, 11, 177–187.
- Tan, Y.T.; Wenzelburger, F.; Lee, E.; Heatlie, G.; Leyva, F.; Patel, K.; Frenneaux, M.; Sanderson, J. The pathophysiology of heart failure with normal ejection fraction: Exercise echocardiography reveals complex abnormalities of both systolic and diastolic ventricular function involving torsion, untwist, and longitudinal motion. J. Am. Coll. Cardiol. 2009, 54, 36–46.
- Yalçin, F.; Yalçin, H.; Küçükler, N.; Abraham, T.P. Quantitative left ventricular contractility analysis under stress: A new practical approach in follow-up of hypertensive patients. J. Hum. Hypertens. 2011, 25, 578–584.
- Diez, J.; Frohlich, E.D. A translational approach to hypertensive heart disease. Hypertension 2010, 55, 1–8.
- Rudolph, A.; Abdel-Aty, H.; Bohl, S.; Boyé, P.; Zagrosek, A.; Dietz, R.; Schulz-Menger, J. Noninvasive detection of fibrosis applying contrast-enhanced cardiac magnetic resonance in different forms of left ventricular hypertrophy relation to remodeling. J. Am. Coll. Cardiol. 2009, 53, 284–291.
More
Information
Subjects:
Cardiac & Cardiovascular Systems
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
2.5K
Revisions:
3 times
(View History)
Update Date:
18 Apr 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





