
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Sari Mahasneh | + 1776 word(s) | 1776 | 2022-03-17 08:48:18 | | | |
| 2 | Beatrix Zheng | Meta information modification | 1776 | 2022-03-21 03:49:36 | | | | |
| 3 | Beatrix Zheng | Meta information modification | 1776 | 2022-03-21 03:51:44 | | |
Video Upload Options
Sinusitis is defined as inflammation of the sinus mucosal lining epithelium. The etiology of sinusitis might include the common cold, influenza, measles, tumors, and anatomical problems and, in some cases, can be of odontogenic origin. Sinusitis of odontogenic origin was first reported and documented in 1943 by Bauer, with a reported prevalence of around 10%. More recent studies—using three-dimensional imaging devices such as cone-beam computed tomography (CBCT)—identified sinusitis of odontogenic origin in up to 40% of cases. According to Ferguson, odontogenic sinusitis (OS) can be caused by apical periodontitis, periodontal disease, dental implants impinging on the maxillary sinus, or extrusion of dental materials. Patients were found to have a higher risk for postoperative OS when large amounts of bone grafts were used during sinus lifting procedures.
1. Introduction
2. Current Insights
-
Group 1: root tips in contact with the sinus floor;
-
Group 2: root tips penetrating into the sinus;
-
Group 3: root tips below the sinus floor.
3. Conclusions
References
- Garry, S.; O’Riordan, I.; James, D.; Corbett, M.; Barry, T.; Thornton, M. Odontogenic Sinusitis—Case Series and Review of Literature. J. Laryngol. Otol. 2021, 136, 49–54.
- Guerra-Pereira, I.; Vaz, P.; Faria-Almeida, R.; Braga, A.-C.; Felino, A. CT maxillary sinus evaluation—A retrospective cohort study. Med. Oral Patol. Oral Cir. Bucal 2015, 20, e419.
- Turfe, Z.; Ahmad, A.; Peterson, E.I.; Craig, J.R. Odontogenic sinusitis is a common cause of unilateral sinus disease with maxillary sinus opacification. Int. Forum Allergy Rhinol. 2019, 9, 1515–1520.
- Whyte, A.; Boeddinghaus, R. Imaging of odontogenic sinusitis. Clin. Radiol. 2019, 74, 503–516.
- Troeltzsch, M.; Pache, C.; Troeltzsch, M.; Kaeppler, G.; Ehrenfeld, M.; Otto, S.; Probst, F. Etiology and clinical characteristics of symptomatic unilateral maxillary sinusitis: A review of 174 cases. J. Cranio-Maxillofac. Surg. 2015, 43, 1522–1529.
- Hoskison, E.; Daniel, M.; Rowson, J.; Jones, N. Evidence of an increase in the incidence of odontogenic sinusitis over the last decade in the UK. J. Laryngol. Otol. 2012, 126, 43.
- Phothikhun, S.; Suphanantachat, S.; Chuenchompoonut, V.; Nisapakultorn, K. Cone-beam computed tomographic evidence of the association between periodontal bone loss and mucosal thickening of the maxillary sinus. J. Periodontol. 2012, 83, 557–564.
- Ugincius, P.; Kubilius, R.; Gervickas, A.; Vaitkus, S. Chronic odontogenic maxillary sinusitis. Stomatologija 2006, 8, 44–48.
- Arias-Irimia, O.; Barona-Dorado, C.; Santos-Marino, J.A.; Martínez-Rodríguez, N.; Martínez-González, J.M. Meta-analysis of the etiology of odontogenic maxillary sinusitis. Med. Oral Patol. Oral Cir. Bucal 2010, 15, e70–e73.
- Allevi, F.; Fadda, G.L.; Rosso, C.; Martino, F.; Pipolo, C.; Cavallo, G.; Felisati, G.; Saibene, A.M. Diagnostic criteria for odontogenic sinusitis: A systematic review. Am. J. Rhinol. Allergy 2021, 35, 713–721.
- Park, M.S.; Eo, M.Y.; Myoung, H.; Kim, S.M.; Lee, J.H. Early diagnosis of jaw osteomyelitis by easy digitalized panoramic analysis. Maxillofac. Plast. Reconstr. Surg. 2019, 41, 6.
- Workman, A.D.; Granquist, E.J.; Adappa, N.D. Odontogenic sinusitis: Developments in diagnosis, microbiology, and treatment. Curr. Opin. Otolaryngol. Head Neck Surg. 2018, 26, 27–33.
- Tataryn, R.; Lewis, M.; Horalek, A.; Thompson, C.; Cha, B.; Pokorny, A. Maxillary Sinusitis of Endodontic Origin: AAE Position Statement. 2018. Available online: https://www.aae.org/specialty/wp-content/uploads/sites/2/2018/04/AAE_PositionStatement_MaxillarySinusitis.pdf (accessed on 15 February 2022).
- Wang, R.-G.; Jiang, S.; Gu, R. The cartilaginous nasal capsule and embryonic development of human paranasal sinuses. J. Otolaryngol. 1994, 23, 239–243.
- Emirzeoglu, M.; Sahin, B.; Bilgic, S.; Celebi, M.; Uzun, A. Volumetric evaluation of the paranasal sinuses in normal subjects using computer tomography images: A stereological study. Auris Nasus Larynx 2007, 34, 191–195.
- Pirner, S.; Tingelhoff, K.; Wagner, I.; Westphal, R.; Rilk, M.; Wahl, F.; Bootz, F.; Eichhorn, K.W. CT-based manual segmentation and evaluation of paranasal sinuses. Eur. Arch. Oto-Rhino-Laryngol. 2009, 266, 507–518.
- Kucybała, I.; Janik, K.A.; Ciuk, S.; Storman, D.; Urbanik, A. Nasal Septal Deviation and Concha Bullosa—Do They Have an Impact on Maxillary Sinus Volumes and Prevalence of Maxillary Sinusitis? Pol. J. Radiol. 2017, 82, 126–133.
- Lana, J.P.; Carneiro, P.M.; Machado Vde, C.; de Souza, P.E.; Manzi, F.R.; Horta, M.C. Anatomic variations and lesions of the maxillary sinus detected in cone beam computed tomography for dental implants. Clin. Oral Implant. Res. 2012, 23, 1398–1403.
- Raghav, M.; Karjodkar, F.R.; Sontakke, S.; Sansare, K. Prevalence of incidental maxillary sinus pathologies in dental patients on cone-beam computed tomographic images. Contemp. Clin. Dent. 2014, 5, 361–365.
- Hsiao, Y.J.; Yang, J.; Resnik, R.R.; Suzuki, J.B. Prevalence of Maxillary Sinus Pathology Based on Cone-Beam Computed Tomography Evaluation of Multiethnicity Dental School Population. Implant. Dent. 2019, 28, 356–366.
- Hiari, M.; Hiari, M.A. Incidental paranasal sinus inflammatory changes in a Jordanian population. East. Mediterr. Health J. 1998, 4, 308–311.
- Eberhardt, J.A.; Torabinejad, M.; Christiansen, E.L. A computed tomographic study of the distances between the maxillary sinus floor and the apices of the maxillary posterior teeth. Oral Surg. Oral Med. Oral Pathol. 1992, 73, 345–347.
- Waite, D.E. Maxillary sinus. Dent. Clin. N. Am. 1971, 15, 349–368.
- Wallace, J.A. Transantral endodontic surgery. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1996, 82, 80–83.
- Kilic, C.; Kamburoglu, K.; Yuksel, S.P.; Ozen, T. An assessment of the relationship between the maxillary sinus floor and the maxillary posterior teeth root tips using dental cone-beam computerized tomography. Eur. J. Dent. 2010, 4, 462–467.
- Mills, R.P.; Kartush, J.M. Orbital wall thickness and the spread of infection from the paranasal sinuses. Clin. Otolaryngol. Allied Sci. 1985, 10, 209–216.
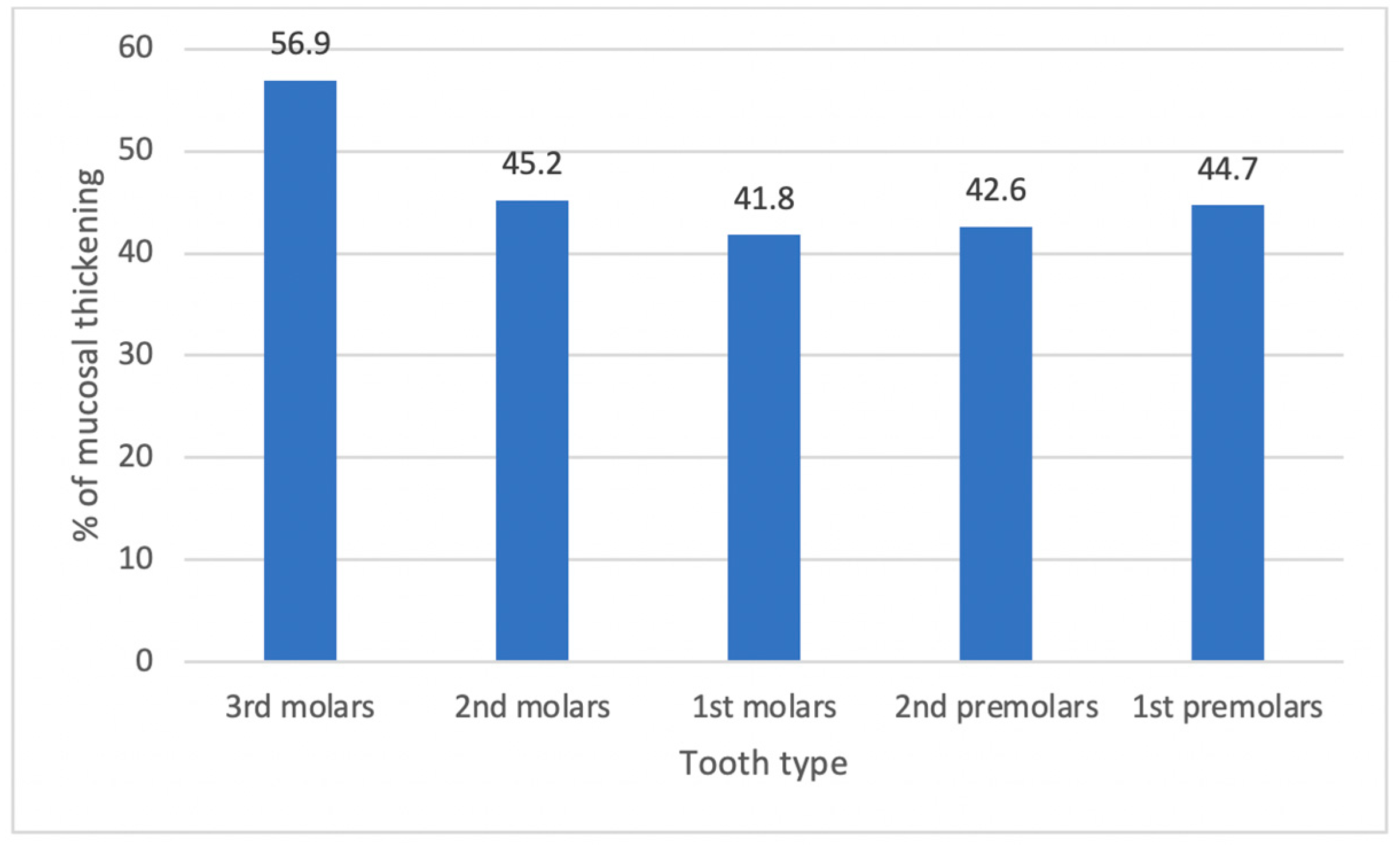
- Aksoy, U.; Orhan, K. Association between odontogenic conditions and maxillary sinus mucosal thickening: A retrospective CBCT study. Clin. Oral Investig. 2019, 23, 123–131.
- van der Borden, W.G.; Wang, X.; Wu, M.-K.; Shemesh, H. Area and 3-dimensional volumetric changes of periapical lesions after root canal treatments. J. Endod. 2013, 39, 1245–1249.
- Lu, Y.; Liu, Z.; Zhang, L.; Zhou, X.; Zheng, Q.; Duan, X.; Zheng, G.; Wang, H.; Huang, D. Associations between maxillary sinus mucosal thickening and apical periodontitis using cone-beam computed tomography scanning: A retrospective study. J. Endod. 2012, 38, 1069–1074.
- Melén, I.; Lindahl, L.; Andréasson, L.; Rundcrantz, H. Chronic maxillary sinusitis: Definition, diagnosis and relation to dental infections and nasal polyposis. Acta Oto-Laryngol. 1986, 101, 320–327.
- Selden, H.S. The endo-antral syndrome. J. Endod. 1977, 3, 462–464.
- Selden, H.S. The endo-antral syndrome: An endodontic complication. J. Am. Dent. Assoc. 1989, 119, 397–398, 401–402.
- Selden, H.S. Endo-Antral syndrome and various endodontic complications. J. Endod. 1999, 25, 389–393.




