1000/1000
Hot
Most Recent

| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Mathias Bonmarin | + 1201 word(s) | 1201 | 2022-02-10 09:25:10 | | | |
| 2 | Catherine Yang | Meta information modification | 1201 | 2022-03-09 08:33:34 | | |
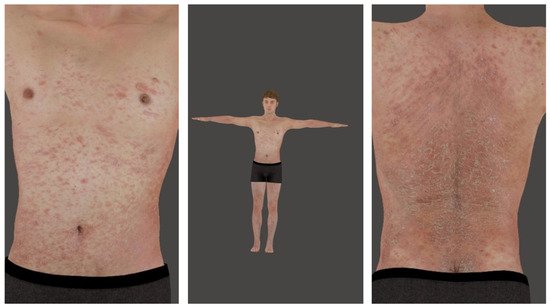
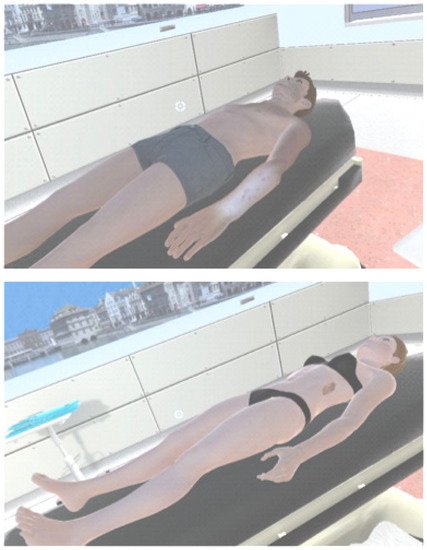
Augmented reality (AR) is a component of virtual reality (VR) or virtual environments (VE) where the user is completely immersed into a synthetic environment. While in VR, the user does not see the real world. Instead, AR allows us to superimpose virtual objects onto real ones. The number of AR/VR applications has undeniably exploded over the last decades. While both techniques have been extensively used in various medical fields, such as in plastic surgery, little investigation has been performed so far in dermatology.