
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Xesús Feás | + 1973 word(s) | 1973 | 2022-02-11 09:08:05 | | | |
| 2 | Vivi Li | -50 word(s) | 1923 | 2022-02-28 02:12:29 | | | | |
| 3 | Vivi Li | -50 word(s) | 1923 | 2022-02-28 02:14:04 | | | | |
| 4 | Vivi Li | Meta information modification | 1923 | 2022-02-28 07:58:12 | | |
Video Upload Options
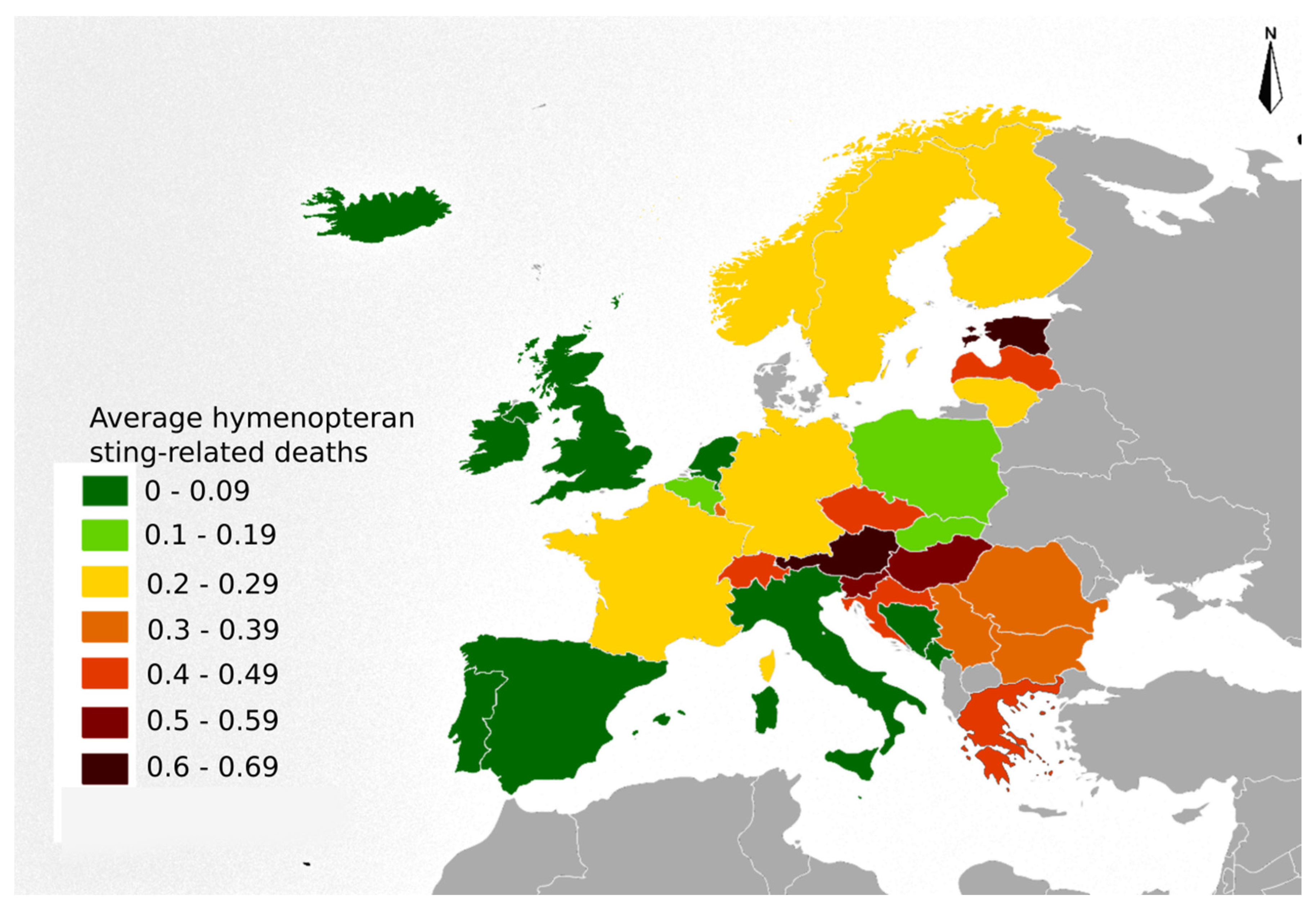
Bees and wasps provide an important service to ecosystems, contributing to the improvement of biodiversity while helping to maintain ecological balance. Although not frequent, hornet, wasp, and bee stings may be life-threatening. With each sting, Hymenopterans inject a small amount of venom that can cause reactions of varying intensity: (i) normal local reactions (NLR), (ii) large local reactions (LLR), (iii) systemic anaphylactic reactions (SAR), (iv) systemic toxic reactions (STR) and (v) unusual reactions (UR). Hymenopteran stings have recently become a worldwide public health concern. However, this health problem can be underestimated despite the number of cases presented. With the expansion of non-native Hymenopteran species across Europe, allergists should be aware that their community’s exposures are continually changing.
1. Introduction
2. Hymenopteran Sting-Related Deaths
| Country 1 | Size | Sum | Minimum | Maximum | Range | Mode | Mean | Median | Standard Deviation | Variance |
|---|---|---|---|---|---|---|---|---|---|---|
| AT | 15 | 73 | 0 | 12 | 12 | 5 | 4.87 | 5 | 3.27 | 10.7 |
| BE | 18 | 27 | 0 | 5 | 5 | 1 | 1.5 | 1 | 1.42 | 2.03 |
| BG | 9 | 26 | 1 | 6 | 5 | 2 | 2.89 | 2 | 1.62 | 2.61 |
| HR | 19 | 35 | 0 | 6 | 6 | 1 | 1.84 | 1 | 1.71 | 2.92 |
| CZ | 23 | 111 | 0 | 14 | 14 | 4 | 4.83 | 4 | 3.04 | 9.24 |
| EE | 17 | 14 | 0 | 3 | 3 | 0 | 0.82 | 1 | 1.01 | 1.03 |
| FI | 20 | 25 | 0 | 4 | 4 | 0 | 1.25 | 1 | 1.25 | 1.57 |
| FR | 15 | 211 | 9 | 23 | 14 | 14 | 14.07 | 14 | 4.15 | 17.21 |
| DE | 18 | 327 | 6 | 32 | 26 | 18 | 18.17 | 18 | 6.97 | 48.62 |
| EL | 2 | 9 | 4 | 5 | 1 | 4 & 5 | 4.5 | 4.5 | 0.71 | 0.5 |
| HU | 21 | 112 | 0 | 13 | 13 | 4 | 5.33 | 4 | 3.54 | 12.53 |
| IE | 8 | 2 | 0 | 1 | 1 | 0 | 0.25 | 0 | 0.46 | 0.21 |
| IT | 13 | 69 | 1 | 12 | 11 | 5 & 3 | 5.31 | 5 | 3.4 | 11.56 |
| LV | 9 | 9 | 0 | 2 | 2 | 2 | 1 | 1 | 1 | 1 |
| LT | 7 | 7 | 0 | 4 | 4 | 1 & 0 | 1 | 1 | 1.41 | 2 |
| LU | 7 | 1 | 0 | 1 | 1 | 0 | 0.14 | 0 | 0.38 | 0.14 |
| NL | 21 | 20 | 0 | 5 | 5 | 0 | 0.95 | 1 | 1.2 | 1.45 |
| NO | 20 | 19 | 0 | 3 | 3 | 1 | 0.95 | 1 | 0.76 | 0.58 |
| PL | 17 | 125 | 3 | 12 | 9 | 7 & 8 & 9 | 7.35 | 8 | 2.67 | 7.12 |
| PT | 13 | 9 | 0 | 4 | 4 | 0 | 0.69 | 0 | 1.32 | 1.73 |
| RO | 18 | 149 | 2 | 16 | 14 | 10 | 8.28 | 9 | 3.44 | 11.86 |
| RS | 18 | 53 | 1 | 6 | 5 | 3 | 2.94 | 3 | 1.43 | 2.06 |
| SK | 21 | 17 | 0 | 2 | 2 | 0 | 0.81 | 1 | 0.81 | 0.66 |
| SI | 19 | 21 | 0 | 4 | 4 | 0 | 1.11 | 1 | 1.37 | 1.88 |
| ES | 17 | 60 | 1 | 8 | 7 | 4 & 3 | 3.53 | 3 | 1.81 | 3.26 |
| SE | 20 | 44 | 0 | 6 | 6 | 1 | 2.2 | 2 | 1.61 | 2.59 |
| CH | 21 | 65 | 1 | 8 | 7 | 4 | 3.1 | 3 | 1.61 | 2.59 |
| UK | 15 | 51 | 1 | 7 | 6 | 2 | 3.4 | 4 | 1.84 | 3.4 |
3. Specific Locations where Hymenopteran Sting-Related Deaths Occurred
4. Age Distribution of Hymenopteran Sting-Related Deaths
5. Hymenopteran Sting-Related Deaths by Gender
6. Hymenopteran Sting-Related Deaths Features by Region: Eastern, Northern, Southern and Western Europe
| Items | Items | Eastern Europe 1 1994–2016 |
Northern Europe 2 1996–2016 |
Southern Europe 3 1995–2015 |
Western Europe 4 1995–2016 |
Europe 1994–2016 |
|---|---|---|---|---|---|---|
| Deaths | Total | 540 | 171 | 256 | 724 | 1691 |
| Men | 425 (78.7%) |
127 (74.3%) |
223 (87.1%) |
545 (75.3%) |
1320 (78.1%) |
|
| Woman | 115 (21.3%) |
44 (25.7%) |
33 (12.9%) |
179 (24.7%) |
371 (21.9%) |
|
| Ratio | X23GR | 3.7 | 2.9 | 6.8 | 3 | 3.6 |
| X23GD | 310 | 83 | 190 | 366 | 949 | |
| Age | ≤14 years | 3 (0.6%) |
- | 2 (0.8%) |
3 (0.4%) |
8 (0.5%) |
| 15–24 years | 10 (1.9%) |
1 (0.6%) |
3 (1.2%) |
7 (1%) |
21 (1.2%) |
|
| 25–64 years | 418 (77.4%) |
101 (59.1%) |
169 (66%) |
440 (60.8%) |
1128 (66.7%) |
|
| ≥65 years | 109 (20.2%) |
55 (32.2%) |
82 (32%) |
274 (37.8%) |
520 (30.8%) |
|
| Place | Not reported | 33 (6.1%) |
52 (30.4%) |
73 (28.5%) |
1 (0.1%) |
159 (9.4%) |
| X23 code extension to four-digit reported 5 | 507 (93.9%) |
119 (69.6%) |
183 (71.5%) |
723 (99.9%) |
1532 (90.6%) |
|
| X23.0 (home) | 241 (44.6%) |
35 (20.5%) |
19 (7.4%) |
202 (27.9%) |
497 (29.4%) |
|
| X23.1 (residential institution) | 5 (0.9%) |
1 (0.6%) |
- | 2 (0.3%) |
8 (0.5%) |
|
| X23.2 (school, other institution and public administrative area) | 5 (0.9%) |
- | 1 (0.4%) |
1 (0.1%) |
7 (0.4%) |
|
| X23.3 (sports and athletics area) | 1 (0.2%) |
- | - | - | 1 (0.1%) |
|
| X23.4 (street and highway) | 17 (3.1%) |
1 (0.6%) |
6 (2.3%) |
30 (4.1%) |
54 (3.2%) |
|
| X23.5 (trade and service area) | - | - | - | - | - | |
| X23.6 (industrial and construction area) | 1 (0.2%) |
- | - | - | 1 (0.1%) |
|
| X23.7 (farm) | 18 (3.3%) |
1 (0.6%) |
6 (2.3%) |
1 (0.1%) |
26 (1.5%) |
|
| X23.8 (other specified place) | 48 (8.9%) |
9 (5.3%) |
21 (8.2%) |
112 (15.5%) |
190 (11.2%) |
|
| X23.9 (unspecified place) | 171 (31.7%) |
72 (42.1%) |
130 (50.8%) |
375 (51.8%) |
748 (44.2%) |
7. Hymenopteran Sting-Related Deaths, X23 Mortality Rates (X23MR)
References
- Cianferoni, A. Non-IgE-mediated anaphylaxis. J. Allergy Clin. Immunol. 2021, 147, 1123–1131.
- Worm, M.; Eckermann, O.; Dölle, S.; Aberer, W.; Beyer, K.; Hawranek, T.; Hompes, S.; Koehli, A.; Mahler, V.; Nemat, K.; et al. Triggers and treatment of anaphylaxis: An analysis of 4000 cases from Germany, Austria and Switzerland. Dtsch. Arztebl. Int. 2014, 111, 367–375.
- Demain, J.G.; Minaei, A.A.; Tracy, J.M. Anaphylaxis and insect allergy. Curr. Opin. Allergy Clin. Immunol. 2010, 10, 318–322.
- Yoon, K.A.; Kim, K.; Kim, W.-J.; Bang, W.Y.; Ahn, N.-H.; Bae, C.-H.; Yeo, J.-H.; Lee, S.H. Characterization of venom components and their phylogenetic properties in some Aculeate bumblebees and wasps. Toxins 2020, 12, 47.
- Pucca, M.B.; Cerni, F.A.; Oliveira, I.S.; Jenkins, T.P.; Argemí, L.; Sørensen, C.V.; Ahmadi, S.; Barbosa, J.E.; Laustsen, A.H. Bee updated: Current knowledge on bee venom and bee envenoming therapy. Front. Immunol. 2019, 10, 2090.
- Pak, S.C. An introduction to the toxins special issue on “bee and wasp venoms: Biological characteristics and therapeutic application”. Toxins 2016, 8, 315.
- Feindor, M.; Heath, M.D.; Hewings, S.J.; Carreno Velazquez, T.L.; Blank, S.; Grosch, J.; Jakob, T.; Schmid-Grendelmeier, P.; Klimek, L.; Golden, D.B.K.; et al. Venom immunotherapy: From proteins to product to patient protection. Toxins 2021, 13, 616.
- Perez-Riverol, A.; Justo-Jacomini, D.L.; Zollner, R.D.L.; Brochetto-Braga, M.R. Facing hymenoptera venom allergy: From natural to recombinant allergens. Toxins 2015, 7, 2551–2570.
- Pascoal, A.; Estevinho, M.M.; Choupina, A.B.; Sousa-Pimenta, M.; Estevinho, L.M. An overview of the bioactive compounds, therapeutic properties and toxic effects of apitoxin. Food Chem. Toxicol. 2019, 134, 110864.
- Abd El-Wahed, A.; Yosri, N.; Sakr, H.H.; Du, M.; Algethami, A.F.M.; Zhao, C.; Abdelazeem, A.H.; Tahir, H.E.; Masry, S.H.D.; Abdel-Daim, M.M.; et al. Wasp venom biochemical components and their potential in biological applications and nanotechnological interventions. Toxins 2021, 13, 206.
- Elieh Ali Komi, D.; Shafaghat, F.; Zwiener, R.D. Immunology of bee venom. Clin. Rev. Allergy Immunol. 2018, 54, 386–396.
- Sahiner, U.M.; Durham, S.R. Hymenoptera venom allergy: How does venom immunotherapy prevent anaphylaxis from bee and wasp stings? Front. Immunol. 2019, 10, 1959.
- Mingomataj, E.Ç.; Bakiri, A.H.; Ibranji, A.; Sturm, G.J. Unusual reactions to hymenoptera stings: What should we keep in mind? Clin. Rev. Allergy Immunol. 2014, 47, 91–99.
- Nittner-Marszalska, M.; Cichocka-Jarosz, E. Insect sting allergy in adults: Key messages for clinicians. Pol. Arch. Med. Wewn. 2015, 125, 929–937.
- Forrester, J.A.; Weiser, T.G.; Forrester, J.D. An update on fatalities due to venomous and nonvenomous animals in the United States (2008–2015). Wilderness Environ. Med. 2018, 29, 36–44.
- Ferreira, R.S., Jr.; Almeida, R.A.; Barraviera, S.R.; Barraviera, B. Historical perspective and human consequences of Africanized bee stings in the Americas. J. Toxicol. Environ. Health B Crit. Rev. 2012, 15, 97–108.
- Herrera, C.; Leza, M.; Martínez-López, E. Diversity of compounds in Vespa spp. venom and the epidemiology of its sting: A global appraisal. Arch. Toxicol. 2020, 94, 3609–3627.
- Tanno, L.K.; Calderon, M.A.; Smith, H.E.; Sanchez-Borges, M.; Sheikh, A.; Demoly, P.; Joint Allergy Academies. Dissemination of definitions and concepts of allergic and hypersensitivity conditions. World Allergy Organ. J. 2016, 9, 24.
- Linard, A.T.S.; Barros, R.M.; Sousa, J.A.; Leite, R.S. Epidemiology of bee stings in Campina Grande, Paraíba state, Northeastern Brazil. J. Venom. Anim. Toxins Incl. Trop. Dis. 2014, 20, 13.
- Golden, D.B.; Demain, J.; Freeman, T.; Graft, D.; Tankersley, M.; Tracy, J.; Blessing-Moore, J.; Bernstein, D.; Dinakar, C.; Greenhawt, M.; et al. Stinging insect hypersensitivity: A practice parameter update 2016. Ann. Allergy Asthma Immunol. 2017, 118, 28–54.
- Bilò, M.B.; Bonifazi, F. The natural history and epidemiology of insect venom allergy: Clinical implications. Clin. Exp. Allergy 2009, 39, 1467–1476.
- Biló, B.M.; Rueff, F.; Mosbech, H.; Bonifazi, F.; Oude-Elberink, J.N.; EAACI Interest Group on Insect Venom Hypersensitivity. Diagnosis of hymenoptera venom allergy. Allergy 2005, 60, 1339–1349.
- International Statistical Classification of Diseases and Related Health Problems (Icd-10) Version: 2019. Available online: https://icd.who.int/browse10/2019/en (accessed on 11 May 2021).




