You're using an outdated browser. Please upgrade to a modern browser for the best experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Seiichiro Makihara | + 1223 word(s) | 1223 | 2022-02-16 04:33:19 | | | |
| 2 | Camila Xu | + 17 word(s) | 1240 | 2022-02-22 03:20:07 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Makihara, S. Sinonasal Inverted Papilloma. Encyclopedia. Available online: https://encyclopedia.pub/entry/19696 (accessed on 26 December 2025).
Makihara S. Sinonasal Inverted Papilloma. Encyclopedia. Available at: https://encyclopedia.pub/entry/19696. Accessed December 26, 2025.
Makihara, Seiichiro. "Sinonasal Inverted Papilloma" Encyclopedia, https://encyclopedia.pub/entry/19696 (accessed December 26, 2025).
Makihara, S. (2022, February 21). Sinonasal Inverted Papilloma. In Encyclopedia. https://encyclopedia.pub/entry/19696
Makihara, Seiichiro. "Sinonasal Inverted Papilloma." Encyclopedia. Web. 21 February, 2022.
Copy Citation
Sinonasal inverted papilloma (SNIP) is a benign neoplasm of the nasal cavity and paranasal sinuses and accounts for 0.5–4% of primary nasal tumors.
HPV infection
sinonasal inverted papilloma
diabetes mellitus
1. Introduction
Sinonasal inverted papilloma (SNIP) is a benign neoplasm of the nasal cavity and paranasal sinuses and accounts for 0.5–4% of primary nasal tumors [1]. SNIP has a tendency to recur (12–20%), and malignant transformation has been found in 3–7% of cases [2]. Thus, many ear, nose, and throat surgeons are interested in understanding which factors are related to tumor recurrence.
The etiology of SNIP remains unknown. Certain hypotheses have been proposed, but causality has never been established for the suspected factors of smoking, allergy, and human papillomavirus (HPV) infection [3]. Several staging systems have been indicated to provide a recurrence rate-driven prognosis [4].
For more than 30 years, HPV has been suspected to play a major role in the pathophysiology of SNIP. Several studies have reported higher HPV detection rates in recurrent SNIP cases [5][6][7], but there is contradictory information about whether HPV-associated SNIP has a higher risk of recurrence [8][9].
2. Clinicopathologic Analysis of Sinonasal Inverted Papilloma
The results of this research on the relationship between clinical or demographic data and recurrence of SNIP showed that younger age (<40 years), presence of DM, advanced tumor stage, and HPV DNA were associated with higher recurrence rates. Pähler et al. also reported that patients who presented with recurrent papilloma infection were significantly younger (48.7 years old on average) at the time of initial diagnosis than those (60.2 years old on average) with non-recurrent tumors (p = 0.0194), and multivariate logistic regression revealed that a younger age at initial diagnosis was the strongest risk factor for neoplasm recurrence [10]. In contrast, several reports found no relationship between recurrence and younger age [4][11][12]. Therefore, a detailed investigation with a large sample size is needed.
Patients with impaired immune responses have a greater tendency to develop HPV-associated disorders [13][14][15]. In patients with DM, a common chronic disease in Japan, the proliferation of macrophages and T cells is altered, and the function of B and NK cells is impaired, which results in abnormal innate and adaptive immunity [16]. Several biological mechanisms may possibly increase the incidence of HPV-related anogenital precancer and cancer occurrence in women with diabetes [17]. As one such mechanism, hyperglycemia in diabetes is related to cell-mediated immune deficiencies and an increased vulnerability to viral infections and, which may endanger clearance of HPV infections and thus boost progression to precancer and cancer development [17][18][19]. Moon et al. reported no relationship between recurrence and DM in 132 cases of SNIP [11]. Here is the first to report the relationship between DM and SNIP recurrence, in addition to DM and HPV infections among patients with SNIP, partially because a limited number of studies examined SNIP and HPV infections.
Krouse [20], Han et al. [21], Cannady et al. [22], and others have proposed several classification staging systems for SNIP. The most widely used classification system is that of Krouse, which emphasizes that tumor extension over the medial maxillary sinus or to the frontal or sphenoid sinus is an important prognostic factor [11][23]. Of the recurrences reported by Gras-Cabrerizo et al. [23] according to the Krouse system: 0% occurred in the T1 stage, 16% in the T2 stage, 25% in the T3 stage, and 60% in the T4 stage (p = 0.05). Furthermore, Moon et al. reported that the Krouse stage T4 group had more frequent recurrences than the T1, T2, and T3 groups did [11]. It is found that patients with Krouse stage T3 showed significant associations with recurrence, compared to those with T1 or T2.
HPV, an epitheliotropic DNA virus, can infect the epidermis or mucosa in humans. During infection, viral DNA sequences of HPV are incorporated into cellular DNA and play a key role in the promotion of neoplasm growth and malignant transformation of SNIP [24]. The detection method and detection rate of HPV-PCR are important points, and there have been several studies that employ HPV-PCR in FFPE samples [25][26][27]. The internal control gene amplification was performed to assess the validity of the results obtained in this study. β-actin and GAPDH were used as the internal controls [28][29]. β-actin (258 bp) was amplified in 31 of 32 cases, and GAPDH (226 bp) was amplified in all cases (Figure 1). These results suggest that HPV-PCR approach is unlikely to result in false negatives due to DNA fragmentation because of formalin fixation. Consistent with detections from previous reports, those with malignant and benign clinical courses could be separated based on high- and low-risk types of HPV, respectively. HPV-6 and -11 are considered as low-grade risk types, while HPV-16 and -18 are considered as high-grade risk types [30]. The detection rate of HPV was increased in SNIP with carcinoma and high-grade dysplasia, as compared to that in SNIP with mild dysplasia or no dysplasia [31]. Meta-analyses showed a significant relationship between HPV infection and malignant transformation of SNIP [32][33]. Additionally, several studies reported that patients who were SNIP positive for HPV infection showed higher levels of recurrence than those who were SNIP-negative for HPV infection [5][6][7]. In contrast, a research of 57 patients reported HPV DNA in seven SNIP areas, all of which were grades II and I (benign) SNIP cases. All other cases were grade III or grade IV (carcinoma arising from SNIP) and negative for HPV DNA. High-risk HPV subtype DNA was found in five of seven cases, suggesting that infection, especially with high-risk HPV subtypes, was an early and stimulating event in tumorigenesis [34]. Taken together, these studies suggest that HPV plays a key role in not only malignant transformation, but also early pathological development and recurrence [30].
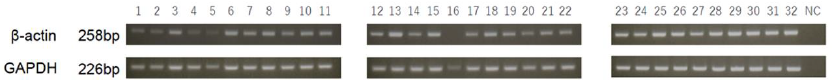 Figure 1. The internal control gene amplification. β-actin (258 bp) was amplified in 31 of 32 cases, and GAPDH (226 bp) was amplified in all cases. NC, negative control.
Figure 1. The internal control gene amplification. β-actin (258 bp) was amplified in 31 of 32 cases, and GAPDH (226 bp) was amplified in all cases. NC, negative control.Smoking is considered the most momentous risk factor for the development and recurrence of tumors occurring in the head, neck, and uterine cervix regions [30][35]. As one of the environmental risk factors, smoking has been associated with recurrence of SNIP. In a research of 132 patients, SNIP had recurrence in 21 of 132 (15.9%) patients. While 11 of the 39 smokers (28.2%) had recurrence of the disease, only 10 of the 93 nonsmokers (10.7%) had recurrence, which showed a significantly higher rate of recurrence among smokers (p = 0.012) [11]. No significant difference between nonsmokers and smokers in the incidence of SNIP recurrence here.
It is indicated that an endoscopic approach was an approving treatment option for SNIP and confirmed a global recommendation that it is the world standard in the treatment of such nose lesions, discovering a lower recurrence rate than that in external approaches. However, the recurrence rate did not show a significant difference between the endoscopic and combined approach groups [36]. Even when an external approach is necessary, the combination of an endoscopic approach is important for suppressing recurrence, as was observed here.
Despite being performed in a single institution, there were still limitations. First, the low positivity rate of HPV DNA made it difficult to evaluate the influence of HPV infection on the SNIP recurrence. Only 5 of 32 patients (15.6%) were positive for HPV DNA in the present study. Three recent PCR-based studies detected HPV in 11 of 90 patients (12.2%) [31], 2 of 19 patients (10.5%) [37], and 8 of 54 patients (14.8%) [4]. The low prevalence of HPV reflects the possibility that HPV infection is not the main causal factor for the pathogenesis of SNIP. Second, there were few patients with the T1 stage according to the Krouse system, and no patient with T4 stage. Furthermore, the number of young patients recruited here was small. A multicenter research with a large sample size is needed to establish the relationship between SNIP recurrence and HPV infection and identify additional risk factors associated with recurrence.
References
- Mirza, S.; Bradley, P.J.; Acharya, A.; Stacey, M.; Jones, N.S. Sinonasal inverted papillomas: Recurrence, and synchronous and metachronous malignancy. J. Laryngol. Otol. 2007, 121, 857–864.
- Adriaensen, G.F.; Lim, K.H.; Georgalas, C.; Reinartz, S.M.; Fokkens, W.J. Challenges in the Management of Inverted Papilloma: A Review of 72 Revision Cases. Laryngoscope 2016, 126, 322–328.
- Lisan, Q.; Laccourreye, O.; Bonfils, P. Sinonasal inverted papilloma: From diagnosis to treatment. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2016, 133, 337–341.
- Roh, H.J.; Mun, S.J.; Cho, K.S.; Hong, S.L. Smoking, not human papilloma virus infection, is a risk factor for recurrence of sinonasal inverted papilloma. Am. J. Rhinol. Allergy 2016, 30, 79–82.
- Hwang, C.S.; Yang, H.S.; Hong, M.K. Detection of human papillomavirus (HPV) in sinonasal inverted papillomas using polymerase chain reaction (PCR). Am. J. Rhinol. 1998, 12, 363–366.
- Beck, J.C.; McClatchey, K.D.; Lesperance, M.M.; Esclamado, R.M.; Carey, T.E.; Bradford, C.R. Human papillomavirus types important in progression of inverted papilloma. Otolaryngol. Head Neck Surg. 1995, 113, 558–563.
- Beck, J.C.; McClatchey, K.D.; Lesperance, M.M.; Esclamado, R.M.; Carey, T.E.; Bradford, C.R. Presence of human papillomavirus predicts recurrence of inverted papilloma. Otolaryngol. Head Neck Surg. 1995, 113, 49–55.
- Kraft, M.; Simmen, D.; Casas, R.; Pfaltz, M. Significance of human papillomavirus in sinonasal papillomas. J. Laryngol. Otol. 2001, 115, 709–714.
- Jenko, K.; Kocjan, B.; Zidar, N.; Poljak, M.; Strojan, P.; Zargi, M.; Blatnik, O.; Gale, N. In inverted papillomas HPV more likely represents incidental colonization than an etiological factor. Virchows Arch. 2011, 459, 529–538.
- Pähler Vor der Holte, A.; Fangk, I.; Glombitza, S.; Wilkens, L.; Welkoborsky, H.J. Prognostic factors and risk factors for development and recurrence of sinonasal papillomas: Potential role of different HPV subtypes. Eur. Arch. Otorhinolaryngol. 2020, 277, 767–775.
- Moon, I.J.; Lee, D.Y.; Suh, M.W.; Han, D.H.; Kim, S.T.; Min, Y.G.; Lee, C.H.; Rhee, C.S. Cigarette smoking increases risk of recurrence for sinonasal inverted papilloma. Am. J. Rhinol. Allergy 2010, 24, 325–329.
- Lisan, Q.; Laccourreye, O.; Bonfils, P. Sinonasal Inverted Papilloma: Risk Factors for Local Recurrence After Surgical Resection. Ann. Otol. Rhinol. Laryngol. 2017, 126, 498–504.
- Geerlings, S.E.; Hoepelman, A.I. Immune dysfunction in patients with diabetes mellitus (DM). FEMS Immunol. Med. Microbiol. 1999, 26, 259–265.
- Heard, I.; Palefsky, J.M.; Kazatchkine, M.D. The impact of HIV antiviral therapy on human papillomavirus (HPV) infections and HPV-related diseases. Antivir. Ther. 2004, 9, 13–22.
- Yong, M.; Parkinson, K.; Goenka, N.; O’Mahony, C. Diabetes and genital warts: An unhappy coalition. Int. J. STD AIDS 2010, 21, 457–459.
- Zhou, T.; Hu, Z.; Yang, S.; Sun, L.; Yu, Z.; Wang, G. Role of Adaptive and Innate Immunity in Type 2 Diabetes Mellitus. J. Diabetes Res. 2018, 2018, 7457269.
- Reinholdt, K.; Thomsen, L.T.; Munk, C.; Dehlendorff, C.; Aalborg, G.L.; Carstensen, B.; Jørgensen, M.E.; Kjaer, S.K. Incidence of human papillomavirus-related anogenital precancer and cancer in women with diabetes: A nationwide registry-based cohort study. Int. J. Cancer 2021, 148, 2090–2101.
- Mor, A.; Dekkers, O.M.; Nielsen, J.S.; Beck-Nielsen, H.; Sørensen, H.T.; Thomsen, R.W. Impact of Glycemic Control on Risk of Infections in Patients with Type 2 Diabetes: A Population-Based Cohort Study. Am. J. Epidemiol. 2017, 186, 227–236.
- Abu-Ashour, W.; Twells, L.; Valcour, J.; Randell, A.; Donnan, J.; Howse, P.; Gamble, J.M. The association between diabetes mellitus and incident infections: A systematic review and meta-analysis of observational studies. BMJ Open Diabetes Res. Care 2017, 5, e000336.
- Krouse, J.H. Development of a staging system for inverted papilloma. Laryngoscope 2000, 110, 965–968.
- Han, J.K.; Smith, T.L.; Loehrl, T.; Toohill, R.J.; Smith, M.M. An evolution in the management of sinonasal inverting papilloma. Laryngoscope 2001, 111, 1395–1400.
- Cannady, S.B.; Batra, P.S.; Sautter, N.B.; Roh, H.J.; Citardi, M.J. New staging system for sinonasal inverted papilloma in the endoscopic era. Laryngoscope 2007, 117, 1283–1287.
- Gras-Cabrerizo, J.R.; Montserrat-Gili, J.R.; Massegur-Solench, H.; León-Vintró, X.; De Juan, J.; Fabra-Llopis, J.M. Management of sinonasal inverted papillomas and comparison of classification staging systems. Am. J. Rhinol. Allergy 2010, 24, 66–69.
- Lin, H.; Lin, D.; Xiong, X.S. Roles of human papillomavirus infection and stathmin in the pathogenesis of sinonasal inverted papilloma. Head Neck 2016, 38, 220–224.
- Alvarez-Aldana, A.; Martínez, J.W.; Sepúlveda-Arias, J.C. Comparison of five protocols to extract DNA from paraffin-embedded tissues for the detection of human papillomavirus. Pathol. Res. Pract. 2015, 211, 150–155.
- Kocjan, B.J.; Hošnjak, L.; Poljak, M. Detection of alpha human papillomaviruses in archival formalin-fixed, paraffin-embedded (FFPE) tissue specimens. J. Clin. Virol. 2016, 76, S88–S97.
- Božić, L.; Jovanović, T.; Šmitran, A.; Janković, M.; Knežević, A. Comparison of HPV detection rate in formalin-fixed paraffin-embedded tissues of head and neck carcinoma using two DNA extraction kits and three amplification methods. Eur. J. Oral. Sci. 2020, 128, 501–507.
- Sengüven, B.; Baris, E.; Oygur, T.; Berktas, M. Comparison of methods for the extraction of DNA from formalin-fixed, paraffin-embedded archival tissues. Int. J. Med. Sci. 2014, 11, 494–499.
- Panchal, N.K.; Bhale, A.; Chowdary, R.; Verma, V.K.; Beevi, S.S. PCR Amplifiable DNA from Breast Disease FFPE Section for Mutational Analysis. J. Biomol. Tech. 2020, 31, 1–6.
- Wang, M.J.; Noel, J.E. Etiology of sinonasal inverted papilloma: A narrative review. World J. Otorhinolaryngol. Head Neck Surg. 2017, 3, 54–58.
- Scheel, A.; Lin, G.C.; McHugh, J.B.; Komarck, C.M.; Walline, H.M.; Prince, M.E.; Zacharek, M.A.; Carey, T.E. Human papillomavirus infection and biomarkers in sinonasal inverted papillomas: Clinical significance and molecular mechanisms. Int. Forum Allergy Rhinol. 2015, 5, 701–707.
- Stepp, W.H.; Farzal, Z.; Kimple, A.J.; Ebert, C.S., Jr.; Senior, B.A.; Zanation, A.M.; Thorp, B.D. HPV in the malignant transformation of sinonasal inverted papillomas: A meta-analysis. Int. Forum Allergy Rhinal. 2021, 11, 1461–1471.
- McCormick, J.P.; Suh, J.D.; Lee, J.T.; Wells, C.; Wang, M.B. Role of High-Risk HPV Detected by PCR in Malignant Sinonasal Inverted Papilloma: A Meta-Analysis. Laryngoscope 2021.
- Kim, J.Y.; Yoon, J.K.; Citardi, M.J.; Batra, P.S.; Roh, H.J. The prevalence of human papilloma virus infection in sinonasal inverted papilloma specimens classified by histological grade. Am. J. Rhinol. 2007, 21, 664–669.
- Nishino, K.; Sekine, M.; Kodama, S.; Sudo, N.; Aoki, Y.; Seki, N.; Tanaka, K. Cigarette smoking and glutathione S-transferase M1 polymorphism associated with risk for uterine cervical cancer. J. Obstet. Gynaecol. Res. 2008, 34, 994–1001.
- Goudakos, J.K.; Blioskas, S.; Nikolaou, A.; Vlachtsis, K.; Karkos, P.; Markou, K.D. Endoscopic Resection of Sinonasal Inverted Papilloma: Systematic Review and Meta-Analysis. Am. J. Rhinol. Allergy 2018, 32, 167–174.
- Stoddard, D.G., Jr.; Keeney, M.G.; Gao, G.; Smith, D.I.; García, J.J.; O’Brien, E.K. Transcriptional activity of HPV in inverted papilloma demonstrated by in situ hybridization for E6/E7 mRNA. Otolaryngol. Head Neck Surg. 2015, 152, 752–758.
More
Information
Subjects:
Otorhinolaryngology
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
723
Revisions:
2 times
(View History)
Update Date:
22 Feb 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




