Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Sujogya Panda | + 2829 word(s) | 2829 | 2022-02-09 10:36:42 | | | |
| 2 | Rita Xu | Meta information modification | 2829 | 2022-02-17 05:18:35 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Panda, S. Anticancer Activities of Mushrooms. Encyclopedia. Available online: https://encyclopedia.pub/entry/19564 (accessed on 07 February 2026).
Panda S. Anticancer Activities of Mushrooms. Encyclopedia. Available at: https://encyclopedia.pub/entry/19564. Accessed February 07, 2026.
Panda, Sujogya. "Anticancer Activities of Mushrooms" Encyclopedia, https://encyclopedia.pub/entry/19564 (accessed February 07, 2026).
Panda, S. (2022, February 17). Anticancer Activities of Mushrooms. In Encyclopedia. https://encyclopedia.pub/entry/19564
Panda, Sujogya. "Anticancer Activities of Mushrooms." Encyclopedia. Web. 17 February, 2022.
Copy Citation
Approximately 270 species of mushrooms have been reported as potentially useful for human health. However, few mushrooms have been studied for bioactive compounds that can be helpful in treating various diseases. Like other natural regimens, the mushroom treatment appears safe, as could be expected from their long culinary and medicinal use.
anticancer activity
bioactive compounds
clinical trials
in vitro
in vivo
medicinal mushrooms
1. Introduction
Estimates of the number of fungal species on Earth range widely, from around half a million to 10 million. Recent estimates by Hawksworth and Lucking indicate 2.2–3.8 million from which only 120,000 species have been named so far [1]. Thus, only about 8% of the estimated number of species is presently known to mycologists [2]. The estimated number of mushroom species on Earth is 150,000–160,000 [3]; however, so far, only ~14,000 species are identified, of which ~7000 have varying degrees of edibility, with 3000 species mainly edible and falling within 21 genera [4]. Moreover, ~2000 species are estimated to be useful medicinally, while only 270 species are reported to possess therapeutic potential for human health [4]. Therefore, mushrooms have already proved themselves as a potential source of drugs against both communicable and non-communicable diseases based on clinical reports. In addition, they supplement primary food in daily life and contain several unique secondary metabolites, polysaccharides, essential minerals, proteins, and vitamins [5][6]. However, only 10% of existing mushroom species are known to science so far, while <1% is exploited for therapeutic uses. From this perspective, mushrooms appear to be a neglected natural source, whose therapeutic potential deserves to be explored in a scientific manner for the discovery of new drugs.
At present, cancer is a leading cause of death worldwide. Nearly 10 million deaths were recorded globally from different cancers in 2020 [https://www.who.int/news-room/fact-sheets/detail/cancer; assessed on 1 January 2022]. Cancer arises through several external factors or agents, such as physical carcinogens by ultraviolet or ionizing radiation, chemical carcinogens by the consumption of contaminated water, food, transition metals, asbestos, aflatoxin, tobacco smoke, etc., and biological carcinogens, such as certain viruses, bacteria, and parasites. It arises through a transformation of normal cells into tumor cells by a multi-stage process from a pre-cancerous lesion to a malignant tumor. According to WHO reports, in 2020, 2.2 million cases of breast cancer were recorded, leading to 685,000 deaths, 2.21 million cases of lung cancer were recorded, with 1.18 million deaths, 1.93 million cases of colon and rectum cancer were recorded, with 935,000 deaths, and 1.09 million cases of stomach cancer were recorded, with 769,000 deaths. “Despite the growing success of conventional personalized cancer therapies, recurrence and metastases remain common, depending on the type of cancer and the stage of disease” [6]. Although early detection and appropriate diagnosis play a crucial role in cancer management, the development of anticancer treatments through synthetic chemicals, or by exploring unique metabolites extracted from mushrooms or other natural sources, is a promising approach to help clinical oncology in developing new cancer drugs.
Over 60% of anticancer drugs can be traced to a natural products, but none so far originate from a mushroom [7]. This is surprising, since mushrooms have long been claimed to have anticancer effects. Traditionally, mushrooms have been used for treating cancers. “Over the past three decades, scientific and medical research in Japan, China, and Korea and recently in the USA have confirmed the properties and unique compounds extracted of mushrooms for prevention and treatment of cancer and other chronic diseases” [8]. A few of these species include: Agaricus, Albatrellus, Antrodia, Calvatia, Clitocybe, Cordyceps, Flammulina, Fomes, Funlia, Ganoderma, Inocybe, Inonotus, Lactarius, Phellinus, Pleurotus, Russula, Schizophyllum, Suillus, Trametes, and Xerocomus, etc. They show promising anticancer activity and may contain potent anticancer compounds. Dunneram et al. have suggested inclusionding of more mushrooms in their diet as a protective measure against cancer [5]. As such, the market for dietary supplements containing mushrooms is rapidly growing, with a market size of over 18 billion USD. This represents about 10% of the overall market for dietary supplements. Fungal genera, such as Ganoderma, Ophiocordyceps, and Cordyceps, have a prominent share [6].
Mushroom-derived polysaccharides exhibit potent antitumor activity against several tumor metastasis cells. Moreover, they showed better activity when used in conjunction with chemotherapy. Mechanistically, the antitumor action is facilitated through a thymus-dependent immune mechanism, which necessitates an intact T cell component. Polysaccharides class components mainly trigger cytotoxic macrophages, natural killer cells, dendritic cells, monocytes, neutrophils, and chemical messengers that activate complementary and acute phase responses. In addition, these polysaccharides act as multi-cytokine inducers, capable of stimulating gene expression of many immunomodulating cytokines and their receptors [7][8][9][10]. Terpenes are another class of compounds, well known for their bioactivity, and many mushroom-derived terpenes have shown potential anticancer properties. Terpenes can modulate the immune system by inducing the expression of genes coding for proteins engaged in the immune response. Mushrooms are also a rich source of carbohydrate-binding proteins known as lectins, and exhibit cytotoxicity/anticancer properties with different mechanisms of action. Several lectins are known to have antitumor and antiproliferative properties. Other important metabolites include phenolic compounds, well known as antioxidants with different mechanisms of action. “Overall, mushroom treatment in oncology studies appeared safe and devoid of side effects. Changes in chemical parameters or clinical signs suggest that mushrooms do affect body physiology, but clinical benefits were more on quality of life than on hard endpoints like disease-free survival or mortality” [9].
2. Summary Results of Literature Analysis
Types and stages of cancer, study parameters (such as sample sizes, dose, treatment duration), and outcomes were noted for each trial with a particular mushroom species. The literature search was performed in PubMed, combining the terms “mushroom” and “cancer”, and limiting the results to clinical trials (https://pubmed.ncbi.nlm.nih.gov/?term=mushrooms+and+cancer&filter=pubt.clinicaltrial&filter=pubt.randomizedcontrolledtrial; assessed on 21 September 2021). This yielded clinical trials on the following medicinal mushrooms (MM): Agaricus bisporus (single trials, [10]); A. blazei (three trials, [11][12][13]); A. sylvaticus (two trials; [14][15]); Antrodia cinnamomea (single trial, [16]); Coriolus versicolor (two trials; [17][18]); Ganoderma lucidum (single trial, [19]); Grifola frondosa (three trials; [20][21][22]); Lentinus edodes (four trials; [23][24][25][26]); Phellinus rimosus (single trial; [27]); Poria cocos (single trial; [28]).
In parallel, researchers searched clinical trial databases to record clinical trial information and added some additional trials on Agaricus bisporus (one randomized phase II trial for prostate cancer, NCT04519879; one interventional clinical trial for breast cancer, NCT007090200), Coriolus versicolor (one randomized, parallel, double-blind, placebo-controlled trial for breast cancer, NCT00647075), Grifola frondosa (one randomized, interventional clinical trial for lung neoplasms and breast carcinoma, NCT02603016), and Trametes versicolor (one phase I clinical trial for breast cancer, NCT02568787). Interestingly, four published reports on Agaricus blazei were based on one trial, but presented different results [16][18][29][30].
They found that the majority of clinical studies were carried out with just 3 species: Lentinula edodes (22.2%), Coriolus versicolor, and Ganoderma lucidum (both 13.9%); followed by Agaricus bisporus and Grifola frondosa (both 11.1%) (Figure 1). There were 2 other species of Agaricus which were also well studied, including A. blazei (8.3%) and A. sylvaticus (5.6%). Most clinical studies were conducted in humans, except one in dogs (whose results are not impressive, as Maitake@ treatment could not reduce lymph node size by more than 50%, while two dogs developed adverse effects [21]).
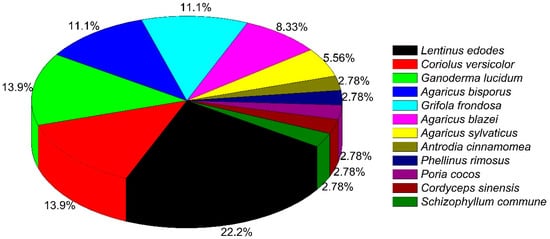
Figure 1. Distribution of mushroom species used in different clinical trials.
The distribution of different types of cancer across the reviewed clinical studies is shown in Figure 2. Most studies were treating breast cancer (18.6%), followed by colorectal (14%) and prostate cancer (11.6%) (Figure 2). Other treated cancer conditions included liver, lung (both 6.98%), cervical, and ovarian cancer (both 4.65%) (Figure 2). Few of these studies were placebo-controlled, double-blind randomized trials (RCTs). The administration of mushrooms was largely oral. Several clinical trials studied a combination with chemotherapy to reduce side effects and improve quality of life (QOL), and observe changes in hematologic parameters (HP), overall survival (OS), antitumor activity, or immunomodulation.
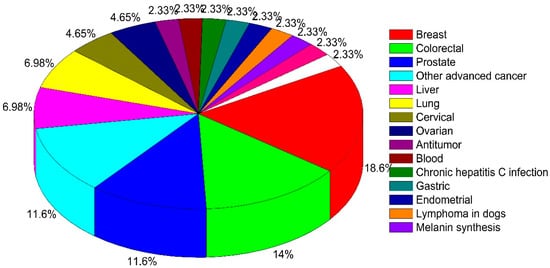
Figure 2. Distribution of various type of cancer among clinical trials.
As only a few mushroom species (11) were evaluated in clinical studies, and the total number of studies was small (only 36), researchers continued their literature search for finding preclinical oncology evidence on mushroom species (database source: https://pubmed.ncbi.nlm.nih.gov/; assessed on 11 October 2021). The anticancer properties from these are summarized for individual species including the type of extracts/fraction/active compounds, type of cancer study, in vitro/in vivo, the dose of treatment, the mechanism involved, etc. Figure 3 and Figure 4 show the distribution of mushrooms with various cancer types for in vitro and in vivo studies, respectively. The most interesting clinical trials with their major outcomes are summarized in Table 1.
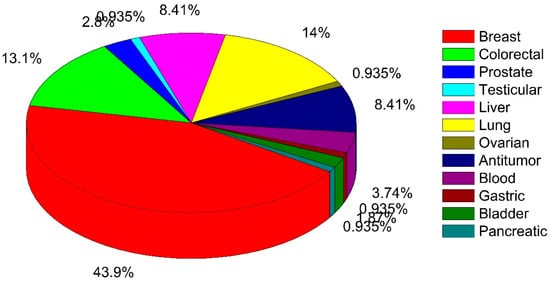
Figure 3. Distribution of various type of cancer among in vitro anticancer studies of mushrooms.
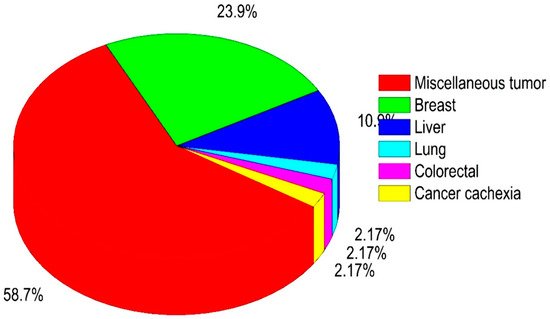
Figure 4. Distribution of in vivo anticancer studies for various type of cancer.
Table 1. Selected clinical studies of mushrooms with anticancer activity.
| Scientific Name | Type of Study | Major Outcomes | Reference |
|---|---|---|---|
| Agaricus bisporus | Phase I trial, n = 32 | Appeared to reduce prostate cancer by decreasing immunosuppressive factors. | [10] * |
| Agaricus blazei | Randomized, placebo-controlled, double-blind clinical trial (RCT), n = 40 | AndoSanTM as adjuvant therapy to high dose of melphalan improved a few immune-modulating effects. In addition, increase in serum levels (IL-1, IL-5, and IL- 7) and expression of antibodies and killer immunoglobulin receptor (KIR) genes were observed. | [12] * |
| Agaricus blazei | RCT, n = 100 | Between treated and non-treated groups, there was no significant difference w.r.t. lymphokine-activated killer and monocyte activities among cervical, ovarian, and endometrial cancer patients undergoing chemotherapy. Additionally, several side effects were improved by verum only when treated with mushroom extract | [13] * |
| Agaricus sylvaticus | RCT, n = 56 | Significant reduction in fasting plasma glucose, total cholesterol, creatinine, aspartate aminotransferase, alanine aminotransferase, IgA, IgM, and systolic and diastolic blood pressure. | [31] |
| Agaricus sylvaticus | RCT, n = 46 | Improved nutritional status with reduced adverse effects (nausea, vomiting, and anorexia), in patients with breast cancer, stage II and III. | [15] |
| Cordyceps sinensis | Clinical study, n = 36 | Jinshuibao capsule (containing constituents similar to Cordyceps sinensis) restored cellular immunological function, improved quality of life (QOL), but had no substantial effect on humoral immune function. | [32] |
| Ganoderma lucidum | Pilot clinical trial, n = 48 | Treated breast cancer patients showed significant enhancements in physical well-being and fatigue with a reduced amount of anxiety and depression. | [19] |
| Ganoderma lucidum | Open label, n = 36 | Ganopoly®® significant increase in mean plasma concentrations of IL-2, IL-6, and IFN-γ, whereas the levels of IL-1 and TNF-α were significantly decreased. The mean absolute number of CD56+ cells was significantly increased, whereas the numbers of CD3+-, CD4+-, and CD8+-expressing cells were just marginally increased compared with baseline levels, with the CD4:CD8 T cell ratios unchanged. PHA responses were enhanced in most patients; and mean NK activity was increased compared with baselines. | [33] |
| Ganoderma lucidum | RCT, n = 68 | A significant increase in Karnofsky scores compared with placebo among the advanced-stage lung cancer patients. Less disease progression. In addition, several cancer-related symptoms and immune parameters were significantly improved in verum. | [34] |
| Ganoderma lucidum | Controlled clinical Trial, n = 198 | Decrease in both number and size of colorectal adenomas for the verum group. | [29] |
| Grifola frondosa | Phase I/II, dose escalation trial, n = 34 | Maitake extracts affects both immunological stimulatory and inhibitory parameters in peripheral blood with treated post-menopausal breast cancer patients. | [20] * |
| Lentinula edodes | Phase II clinical trial, n = 74 | Mushroom extract failed to reduce by >50% prostate- specific antigen in early stage prostrate cancer patients. | [24] * |
| Lentinus edodes | Clinical trial, n = 62 | Administration of L. edodes extract in prostate cancer patients failed to stabilize or halt progression of disease. | [25] * |
| Schizophyllum commune | Clinical trial, n = 220 | Tumor-reducing effect in cervical cancer patients with stage II or III. Time to recurrence was longer in in stage II but not stage III cancer, compared with control group; 48-month survival time of patients with stage II but not stage III cancer in the SPG group was significantly longer than in the control group. | [30] |
| Trametes versicolor | Controlled trial, n = 60 | Significantly improved symptoms of Qi and Yin deficiency in gastric cancer patients after chemotherapy. | [35] |
RCT—randomized clinical trial; *—papers also retrieved from SciFinder.
For in vitro studies with cell lines, most used breast cancer cell lines (43.9%), followed by lung (14%) and colorectal (13.1%), as well as (8.41%) liver cancer cell lines (Figure 3). For in vivo studies, most papers pertained to antitumor effects in mice (58.7%), which may be due to the common availability of tumor mouse models (Figure 4). Moreover, among the cancer types once more breast cancer is most studied (23.9%) followed by liver cancer (10.9%) (Figure 4). To facilitate interpretation, they summarized all mushrooms species per type of cancer in Table 2, listing in vitro vs. in vivo as well as clinical trials.
Table 2. Summary list of mushroom species studied for anticancer properties.
| Cancer Type | In Vitro Study | In Vivo Study | Clinical Trial |
|---|---|---|---|
| Miscellaneous tumors | Agaricus bisporus, Agaricus blazei, Antrodia camphorata, Grifola frondosa, Phellinus linteus, Phellinus rimosus, Ramaria flava | Agaricus blazei, Agaricus sylvaticus, Antrodia camphorata, Amauroderma rude, Cordyceps sinensis, Flammulina velutipes, Ganoderma lucidum, Grifola frondosa, Lentinus edodes, Lepista inversa, Pleurotus nebrodensis, Tricholoma mongolicum | Phellinus rimosus |
| Bladder | Phellinus linteus, Poria cocos | - | - |
| Blood | Agaricus blazei, Cordyceps sinensis, Grifola frondosa, Pleurotus ostreatus | - | Grifola frondosa |
| Breast | Agaricus bisporus, Agaricus blazei, Amauroderma rude, Antrodia cinnamomea, Antrodia camphorata, Antrodia salmonea, Amauroderma rude, Cordyceps sinensis, Coriolus versicolor, Cortinarius xiphidipus, Fuscoporia torulosa, Ganoderma lucidum, Grifola frondosa, Inonotus obliquus, Laetiporus sulphureus, Lentinus crinitus, Lentinus polychrous, Lignosus rhinocerotis, Lignosus tigris, Marasmius oreades, Phellinus linteus, Phellinus rimosus, Pholiota adiposa, Pholiota nameko, Pleurotus abalones, Pleurotus djamor, Pleurotus highking, Pleurotus nebrodensis, Pleurotus ostreatus, Poria cocos, Tricholoma mongolicum, Xylaria schweinitzii | Agaricus bisporus, Agaricus blazei, Amauroderma rude, Antrodia salmonea, Ganoderma lucidum, Lignosus tigris, Phellinus rimosus, Poria cocos, Schizophyllum commune | Agaricus bisporus, Agaricus sylvaticus, Coriolus versicolor, Ganoderma lucidum, Grifola frondosa |
| Cancer cachexia | - | Antrodia cinnamomea | |
| Cervical | - | - | Agaricus blazei, Schizophyllum commune |
| Chronic hepatitis C infection | - | - | Agaricus blazei |
| Colorectal | Agaricus bisporus, Agaricus blazei, Antrodia salmonea, Cerrena unicolor, Ganoderma lucidum, Grifola frondosa, Inonotus obliquus, Lentinan, Marasmius oreades, Phellinus linteus, Pleurotus sajor-caju, Pleurotus ostreatus, Pycnoporus sanguineus, Sarcodon aspratus, Taiwanofungus salmoneus | Agaricus blazei | Agaricus sylvaticus, Ganoderma lucidum, Lentinan |
| Endometrial | - | - | Agaricus blazei |
| Gastric | Agaricus blazei | - | Trametes versicolor, Lentinan |
| Liver | Agaricus blazei, Auricularia auricula-judae, Cordyceps sinensis, Coriolus versicolo, Lentinan, Russula alatoreticula, Thelephora aurantiotincta, Tricholoma mongolicum, Xylaria schweinitzii | Agaricus blazei, Auricularia auricula-judae, Ganoderma lucidum, Phellinus linteus, Schizophyllum commune | Coriolus versicolo, Lentinan |
| Lung | Agaricus blazei, Antrodia cinnamomea, Cordyceps sinensis, Flammulina velutipes, Ganoderma lucidum, Grifola frondosa, Inonotus obliquus, Lentinula edodes, Phellinus linteus, Lentinus squarrosulus, Pleurotus nebrodensis, Pleurotus nebrodensis | Poria cocos | Ganoderma lucidum, Grifola frondosa |
| Lymphoma in dogs | - | - | Grifola frondosa |
| Myeloma | - | - | Agaricus blazei |
| Nasopharyngeal | - | - | Ganoderma lucidum |
| Ovarian | Antrodia salmonea | - | Agaricus blazei, Agaricus bisporus, Volvariella volvacea |
| Pancreatic | Agaricus blazei | - | - |
| Prostate | Fuscoporia torulosa, Ganoderma lucidum, Lentinula edodes, Phellinus linteus | - | Agaricus bisporus, Lentinula edodes |
| Testicular | Cordyceps sinensis | - | - |
| Other advanced cancers | - | - | Antrodia cinnamomea, Cordyceps sinensis, Ganoderma lucidum, Lentinula edodes |
“-”—no data available.
For more detailed interpretation, a summary table was prepared listing the name of the mushroom species aimed at different types of cancer. After analyzing the types of studies, each category, such as in vitro, in vivo, in silico, isolation of active constituents, and clinical study, was rated with scores—ideal (excellent, >5 studies-***), (good, 3–5 studies-**), (poor, 1–2 studies-*), or no study (-)—and the overall strength of recommendation score was given based on the available literature (Table 3).
Table 3. Scores for each species of mushrooms regarding its anticancer properties.
| Name of the Mushroom | Type of Cancer | Type of Studies (References) | Overall Strength of Recommendation | ||||
|---|---|---|---|---|---|---|---|
| In Vitro | In Vivo | In Silico | Clinical Study | Active Constituents | |||
| Agaricus bisporus | Breast, colon, prostate cancer | *** | ** | *** | ** | ** | ** |
| Agaricus blazei | Several types of cancer: myeloma, leukemia, chronic hepatitis C infection, breast, cervical, ovarian, lung, pancreatic, and endometrial | *** | *** | - | *** | *** | *** |
| Agaricus sylvaticus | Colorectal and breast cancer | *** | ** | - | *** | * | ** |
| Amauroderma rude | Breast cancer | *** | * | - | - | ** | * |
| Antrodia cinnamomea | Breast and lung cancer | *** | *** | - | * | ** | ** |
| Antrodia camphorata | Miscellaneous tumor | ** | * | - | - | * | * |
| Antrodia salmonea | Breast, colon, and ovarian cancer | *** | ** | - | - | * | * |
| Auricularia auricula-judae | Hepatoma | * | - | * | - | * | * |
| Cerrena unicolor | Colon cancer, miscellaneous tumors | *** | * | - | - | - | * |
| Cordyceps sinensis | Lung and testicular cancer | *** | * | ** | * | ** | ** |
| Coriolus versicolor | Breast, gastric, and liver cancer | *** | *** | *** | *** | ** | *** |
| Cortinarius xiphidipus | Several types | * | - | - | - | - | - |
| Flammulina velutipes | Lung cancer and miscellaneous tumor | ** | - | * | - | *** | * |
| Fuscoporia torulosa | Brest and prostate cancer | * | - | - | - | - | - |
| Ganoderma lucidum | Breast, lung, colorectal, and Nasopharyngeal cancer |
*** | *** | *** | *** | *** | *** |
| Grifola frondosa | Blood, breast, and lung cancer | *** | ** | * | *** | *** | *** |
| Inonotus obliquus | Breast cancer | *** | ** | * | - | *** | ** |
| Lentinus edodes | Breast, lung, colorectal, gastric, and liver cancer | *** | ** | ** | *** | *** | *** |
| Lentinus squarrosulus | Lung cancer | * | - | - | - | - | - |
| Lepista inversa | Several cancer cell lines | * | - | - | - | - | - |
| Lignosus rhinocerotis | Breast cancer | ** | * | * | - | ** | * |
| Lignosus tigris | Breast cancer | ** | * | - | - | * | * |
| Marasmius oreades | Colon and breast cancer | ** | * | - | - | * | * |
| Phellinus linteus | Colon, liver, lungs, and prostate cancer | *** | ** | * | - | *** | ** |
| Phellinus rimosus | Colon and liver cancer | *** | * | - | - | ** | * |
| Pholiota nameko | Breast cancer | ** | * | - | - | * | * |
| Pleurotus abalones | Breast cancer | ** | * | - | - | * | * |
| Pleurotus highking | Breast cancer | ** | * | - | - | * | * |
| Pleurotus nebrodensis | Liver, lungs, and breast cancer | *** | * | - | - | ** | * |
| Pleorotus ostreatus | Blood, lungs, and breast cancer | *** | ** | * | - | * | * |
| Poria cocos | Breast and pancreatic cancer | *** | ** | ** | * | *** | ** |
| Pycnoporus sanguineus | Colon cancer | * | - | - | - | - | - |
| Ramaria flava | Liver cancer | ** | - | - | - | - | - |
| Russula alatoreticula | Liver cancer | * | - | - | - | - | - |
| Schizophyllum commune | Breast, liver, and cervical cancer | *** | * | - | * | ** | ** |
| Thelephora aurantiotincta | Liver cancer | * | - | - | - | - | - |
| Taiwanofungus salmoneus | Colon and liver cancer | *** | * | - | - | ** | * |
| Tricholoma mongolicum | Breast and liver cancer | *** | - | - | - | * | * |
| Xylaria schweinitzii | Breast, liver, and lung cancer | * | - | - | - | * | - |
***—excellent, >5 studies; **—good, 3–5 studies; *—poor, 1–2 studies; “-”—no study.
References
- Hawksworth, D.L.; Lücking, R. Fungal diversity revisited: 2.2 to 3.8 million species. Microbiol. Spectr. 2017, 5, 5.
- Wasser, S.P. Medicinal mushroom science: Current perspectives, advances, evidences, and challenges. Biomed. J. 2014, 37, 345–356.
- Chang, S.T.; Wasser, S.P. The cultivation and environmental impact of mushrooms. In Oxford Research Encyclopedias Environmental Science; Oxford University Press: Oxford, UK, 2017.
- Sharma, S.K.; Gautam, N. Chemical, bioactive, and antioxidant potential of twenty wild culinary mushroom species. BioMed Res. Int. 2015, 2015, 346508.
- Wasser, S.P. Medicinal Mushrooms in Human Clinical Studies. Part I. Anticancer, Oncoimmunological, and Immunomodulatory Activities: A Review. Int. J. Med. Mushrooms 2017, 19, 279–317.
- Jeitler, M.; Michalsen, A.; Frings, D.; Hübner, M.; Fischer, M.; Koppold-Liebscher, D.A.; Murthy, V.; Kessler, C.S. Significance of Medicinal Mushrooms in Integrative Oncology: A Narrative Review. Front. Pharmacol. 2020, 11, 580656.
- Demain, A.L.; Vaishnav, P. Natural products for cancer chemotherapy. Microb. Biotechnol. 2011, 4, 687–699.
- Figueiredo, L.; Régis, W.C.B. Medicinal mushrooms in adjuvant cancer therapies: An approach to anticancer effects and presumed mechanisms of action. Nutrire 2017, 42, 28.
- Panda, S.K.; Luyten, W. Medicinal mushrooms: Clinical perspective and challenges. Drug Discov. Today 2021, 27, 636–651.
- Twardowski, P.; Kanaya, N.; Frankel, P.; Synold, T.; Ruel, C.; Pal, S.K.; Junqueira, M.; Prajapati, M.; Moore, T.; Tryon, P.; et al. A phase I trial of mushroom powder in patients with biochemically recurrent prostate cancer: Roles of cytokines and myeloid-derived suppressor cells for Agaricus bisporus-induced prostate-specific antigen responses. Cancer 2015, 121, 2942–2950.
- Grinde, B.; Hetland, G.; Johnson, E. Effects on gene expression and viral load of a medicinal extract from Agaricus blazei in patients with chronic hepatitis C infection. Int. Immunopharmacol. 2006, 6, 1311–1314.
- Tangen, J.-M.; Tierens, A.; Caers, J.; Binsfeld, M.; Olstad, O.K.; Trøseid, A.-M.S.; Wang, J.; Tjønnfjord, G.E.; Hetland, G. Clinical Study immunomodulatory effects of the Agaricus blazei Murrill-based mushroom extract AndoSan in patients with multiple myeloma undergoing high dose chemotherapy and autologous stem cell transplantation: A randomized, double blinded clinical study. BioMed Res. Int. 2015, 2015, 718539.
- Ahn, W.S.; Kim, D.J.; Chae, G.T.; Lee, J.M.; Bae, S.M.; Sin, J.I.; Kim, Y.W.; Namkoong, S.E.; Lee, I.P. Natural killer cell activity and quality of life were improved by consumption of a mushroom extract, Agaricus blazei Murill Kyowa, in gynecological cancer patients undergoing chemotherapy. Int. J. Gynecol. Cancer 2004, 14, 589–594.
- Fortes, R.C.; Recôva, V.L.; Melo, A.L.; Novaes, M.R.C.G. Effects of dietary supplementation with medicinal fungus in fasting glycemia levels of patients with colorectal cancer: A randomized, double-blind, placebo-controlled clinical study. Nutr. Hosp. 2008, 23, 591–598.
- Valadares, F.; Novaes, M.R.C.G.; Cañete, R. Effect of Agaricus sylvaticus supplementation on nutritional status and adverse events of chemotherapy of breast cancer: A randomized, placebo-controlled, double-blind clinical trial. Indian J. Pharmacol. 2013, 45, 217–222.
- Tsai, M.Y.; Hung, Y.C.; Chen, Y.H.; Chen, Y.H.; Huang, Y.C.; Kao, C.W.; Su, Y.L.; Chiu, H.H.E.; Rau, K.M. A preliminary randomised controlled study of short-term Antrodia cinnamomea treatment combined with chemotherapy for patients with advanced cancer. BMC Complement. Altern. Med. 2016, 16, 322.
- Chay, W.Y.; Tham, C.K.; Toh, H.C.; Lim, H.Y.; Tan, C.K.; Lim, C.; Wang, W.W.; Choo, S.P. Coriolus versicolor (Yunzhi) use as therapy in advanced hepatocellular carcinoma patients with poor liver function or who are unfit for standard therapy. J. Altern. Complement. Med. 2017, 23, 648–652.
- Torkelson, C.J.; Sweet, E.; Martzen, M.R.; Sasagawa, M.; Wenner, C.A.; Gay, J.; Putiri, A.; Standish, L.J. Phase 1 clinical trial of Trametes versicolor in women with breast cancer. ISRN Oncol. 2012, 2012, 251632.
- Zhao, H.; Zhang, Q.; Zhao, L.; Huang, X.; Wang, J.; Kang, X. Spore powder of Ganoderma lucidum improves cancer-related fatigue in breast cancer patients undergoing endocrine therapy: A pilot clinical trial. Evid.-Based Complement. Altern. Med. 2012, 2012, 809614.
- Deng, G.; Lin, H.; Seidman, A.; Fornier, M.; D’Andrea, G.; Wesa, K.; Yeung, S.; Cunningham-Rundles, S.; Vickers, A.J.; Cassileth, B. A phase I/II trial of a polysaccharide extract from Grifola frondosa (Maitake mushroom) in breast cancer patients: Immunological effects. J. Cancer Res. Clin. Oncol. 2009, 135, 1215–1221.
- Griessmayr, P.C.; Gauthier, M.; Barber, L.G.; Cotter, S.M. Mushroom-derived Maitake PETfraction as single agent for the treatment of lymphoma in dogs. J. Vet. Intern. Med. 2007, 21, 1409–1412.
- Wesa, K.M.; Cunningham-Rundles, S.; Klimek, V.M.; Vertosick, E.; Coleton, M.I.; Yeung, K.S.; Lin, H.; Nimer, S.; Cassileth, B.R. Maitake mushroom extract in myelodysplastic syndromes (MDS): A phase II study. Cancer Immunol. Immunother. 2014, 64, 237–247.
- Ito, T.; Urushima, H.; Sakaue, M.; Yukawa, S.; Honda, H.; Hirai, K.; Igura, T.; Hayashi, N.; Maeda, K.; Kitagawa, T.; et al. Reduction of adverse effects by a mushroom product, active hexose correlated compound (AHCC) in patients with advanced cancer during chemotherapy-the significance of the levels of HHV-6 DNA in saliva as a surrogate biomarker during chemotherapy. Nutr. Cancer 2014, 66, 377–382.
- Sumiyoshi, Y.; Hashine, K.; Kakehi, Y.; Yoshimura, K.; Satou, T.; Kuruma, H.; Namiki, S.; Shinohara, N. Dietary administration of mushroom mycelium extracts in patients with early stage prostate cancers managed expectantly: A phase II study. Jpn. J. Clin. Oncol. 2010, 40, 967–972.
- DeVere White, R.W.; Hackman, R.M.; Soares, S.E.; Beckett, L.A.; Sun, B. Effects of a mushroom mycelium extract on the treatment of prostate cancer. Urology 2002, 60, 640–644.
- Yamaguchi, Y.; Miyahara, E.; Hihara, J. Efficacy and safety of orally administered Lentinula edodes mycelia extract for patients undergoing cancer chemotherapy: A pilot study. Am. J. Chin. Med. 2011, 39, 451–459.
- Meera, C.R.; Janardhanan, K.K. Antitumor activity of a polysaccharide-protein complex isolated from a wood-rotting polypore macro fungus Phellinus rimosus (Berk) pilat. J. Environ. Pathol. Toxicol. Oncol. 2012, 31, 223–232.
- Lee, H.; Cha, H.J. Poria cocos Wolf extracts represses pigmentation in vitro and in vivo. Cell. Mol. Biol. 2018, 64, 80–84.
- Oka, S.; Tanaka, S.; Yoshida, S.; Hiyama, T.; Ueno, Y.; Ito, M.; Kitadai, Y.; Yoshihara, M.; Chayama, K. A water-soluble extract from culture medium of Ganoderma lucidum mycelia suppresses the development of colorectal adenomas. Hiroshima J. Med. Sci. 2010, 59, 1–6.
- Okamura, K.; Suzuki, M.; Yajima, A.; Chihara, T.; Fujiwara, A.; Fukuda, T.; Goto, S.; Ichinohe, K.; Jimi, S.; Kasamatsu, T.; et al. Clinical evaluation of Schizophyllan combined with irradiation in patients with cervical cancer: A randomized controlled study. Cancer 1986, 58, 865–872.
- Fortes, R.C.; Novaes, M.R.C.G. The effects of Agaricus sylvaticus fungi dietary supplementation on the metabolism and blood pressure of patients with colorectal cancer during post surgical phase. Nutr. Hosp. 2011, 26, 176–186.
- Zhou, D.; Lin, L. Effect of Jinshuibao capsule on the immunological function of 36 patients with advanced cancer. Zhongguo Zhongxiyi jiehe Zazhi = Chin. J. Integr. Tradit. West. Med. 1995, 15, 476–478.
- Gao, Y.; Zhou, S.; Jiang, W.; Huang, M.; Dai, X. Effects of Ganopoly® (a Ganoderma lucidum polysaccharide extract) on the immune functions in advanced-stage cancer patients. Immunol. Investig. 2003, 32, 201–215.
- Gao, Y.; Dai, X.; Chen, G.; Ye, J.; Zhou, S. A randomized, placebo-controlled, multicenter study of Ganoderma lucidum (W.Curt.:Fr.) Lloyd (Aphyllophoromycetideae) polysaccharides (Ganopoly) in patients with advanced lung cancer. Int. J. Med. Mushrooms 2003, 5, 14.
- Zuo, Z.; Zuo, Z.; Liying, Z. Clinical observation on alleviating chemotherapy’s side effect of psp in treating gastric careinoma. Liaoning J. Tradit. Chin. Med. 2001, 28, 668–669.
More
Information
Subjects:
Medical Informatics
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.6K
Revisions:
2 times
(View History)
Update Date:
29 Mar 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




