Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Yingxiao Li | + 1447 word(s) | 1447 | 2022-01-20 05:19:35 | | | |
| 2 | Vivi Li | Meta information modification | 1447 | 2022-02-07 03:11:49 | | | | |
| 3 | Vivi Li | Meta information modification | 1447 | 2022-02-08 11:20:33 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Li, Y. Gan-Mai-Da-Zao and Depression in Rat Models. Encyclopedia. Available online: https://encyclopedia.pub/entry/19108 (accessed on 07 January 2026).
Li Y. Gan-Mai-Da-Zao and Depression in Rat Models. Encyclopedia. Available at: https://encyclopedia.pub/entry/19108. Accessed January 07, 2026.
Li, Yingxiao. "Gan-Mai-Da-Zao and Depression in Rat Models" Encyclopedia, https://encyclopedia.pub/entry/19108 (accessed January 07, 2026).
Li, Y. (2022, February 04). Gan-Mai-Da-Zao and Depression in Rat Models. In Encyclopedia. https://encyclopedia.pub/entry/19108
Li, Yingxiao. "Gan-Mai-Da-Zao and Depression in Rat Models." Encyclopedia. Web. 04 February, 2022.
Copy Citation
Gan-Mai-Da-Zao (GMDZ) is a well-known product in Chinese traditional medicine and includes three major plants: blighted wheat (Fu Mai), licorice (Gan Cao), and jujube (Da Zao). GMDZ is widely used as an efficacious and well-tolerated prescription for depression in clinics.
Gan-Mai-Da-Zao
depression
brain-derived neurotrophic factor
serotonin transporter
unpredictable chronic mild stress
1. Introduction
Major depression is a common psychiatric disorder and it may lead to emotional depression, suicidal tendencies, and a recurrence of morbidity [1]. Dysfunction of the serotonin (5-HT) system is commonly considered to be the cause of depression. Depression has been shown as the negative factor that affects the rate of adult hippocampal neurogenesis. The serotonin transporter (5-HTT) responsible for the reuptake of 5-HT is related to the role of 5-HT in neurodevelopmental processes [2]. The evidence from animal models and human studies indicates that reduced function of 5-HTT is associated with the decreased expression of brain-derived neurotrophic factor (BDNF) [3]. Additionally, BDNF is highly expressed in the adult hippocampus and hypothalamus [4], and is involved in the etiopathology of mood disorders [5]. In depressive patients, serum BDNF levels are markedly decreased [6] that can be restored by antidepressant treatment [7]. Although today’s treatments for depression have greatly improved, it is still necessary to find more safe and effective agents to prevent depression.
Traditional Chinese medicine (TCM) has shown the therapeutic effects of depression [8][9]. GMDZ is one of the well-known products in TCM and it has widely been used to treat depressive patients in Asia. Despite the large variety of TCM patterns among participants, dozens of herbal formulas for depression were GMDZ-based [10]. This was first documented in the Chinese medical book Jin-Gui-Yao-Lue (Synopsis of Prescriptions of the Golden Chamber) written by Dr. Zongjing Zhang (AD 152-219) [11]. GMDZ is believed to be effective for depression [12]. Clinical studies indicated that GMDZ decoction is an efficacious and well-tolerated antidepressant prescription for depressive disorders, even postpartum depression [13][14][15]. Moreover, GMDZ could protect hippocampal neurons against glutamate toxicity in depression-like rats [16][17]. The composition of GMDZ includes three major plants: blighted wheat (FuMai, M), licorice (GanCao, G), and jujube (DaZao, D) [16]. The combination of three plants may enhance the efficiency and/or reduce toxicity in clinical applications. However, the role of these components in GMDZ is still vague.
2. Chronic GMDZ Treatment Ameliorated Depression-Like Behaviors in UCMS Rats and PCPA Treated Rats
FST shows a high predictive validity for antidepressant activity. OFT is classically used to assess anxiety in rodents. In the present study, the UCMS group significantly prolonged the immobility time in the FST (Figure 1a); and also reduced the time spent at the center and decreased the total distance traveled in the OFT compared with the control group (Figure 1b,c). Similar results were observed in depressive rats induced by PCPA in FST (Figure 1e) and OFT (Figure 1f,g). To assess the antidepressant-like effects of GMDZ, rats were orally administrated GMDZ for 21 days while fluoxetine (10 mg/kg) was included as the positive control. The results showed that GMDZ produced a significant reduction in the duration of immobility as well as the time in the center and distance of traveling in OFT. It indicated that GMDZ significantly ameliorated depression-like behaviors compared with the vehicle-treated animals. Additionally, fluoxetine showed marked effects on FST and OFT in the UCMS group which were not observed in the PCPA-induced model.
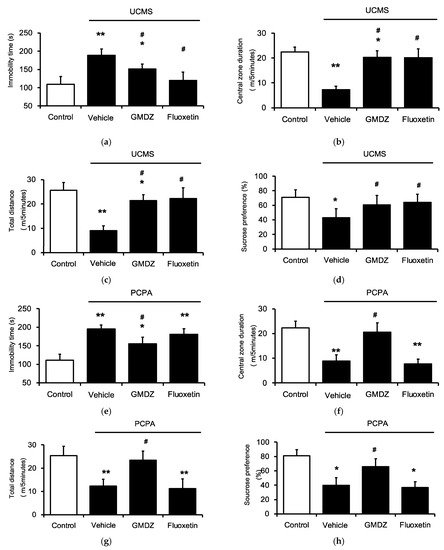
Figure 1. GMDZ ameliorated depression-like behaviors in two rat models induced by the UCMS or PCPA injection. (a) The changes of immobility time in FST in UCMS model; (b) the changes of time in central in OFT in UCMS model; (c) the changes of traveling distance in OFT in UCMS model; (d) the changes of sucrose solution consumption (%) in SPT in UCMS model; (e) the changes of immobility time in FST in PCPA treated groups; (f) the changes of time in central in OFT in PCPA treated groups; (g) the changes of traveling distance in OFT in PCPA treated groups; (h) the changes of sucrose solution consumption (%) in SPT in PCPA treated groups. Responses to fluoxetine used as the positive control. Data are expressed as mean ± SE (n = 8). * p < 0.05, ** p < 0.01 compared with the normal control group; # p < 0.05 compared with vehicle-treated group.
The SPT is a procedure which is used to measure the hedonic value of sucrose, typically reduced in animals with depression-like disorders. Both the UCMS and PCPA groups (Figure 1h) showed a significant decrease in sucrose consumption as compared with the control. However, the sucrose consumption in both models was significantly restored by the chronic administration of GMDZ. PCPA-induced stressed rats treated with fluoxetine did not differ in sucrose preference from the vehicle-treated group. Therefore, GMDZ produces antidepressant effects through different mechanisms to fluoxetine.
3. Effects of Two-Herb Mixture of GMDZ on Behavioral Tests in PCPA-Induced Rats
To understand the major plant in GMDZ, a one-plant deletion from the mixture was prepared. Then, five groups of PCPA-induced rats were administered with GMDZ, G and M, M and DZ, G and DZ, and the vehicle, respectively, for 21 days. In both G and M and G and DZ groups, rats showed a shorter immobility time in FST (Figure 2a), a longer central zone duration and a greater total distance in OFT (Figure 2b,c), and a higher sucrose intake in SPT (Figure 2d) which ameliorated the depression-like behaviors. However, M and DZ did not show an obvious effect in FST, OFT, or SPT, respectively. These results suggest that G seems to play a crucial role in the effect of GMDZ using PCPA-induced rats showing depression-like behavior.
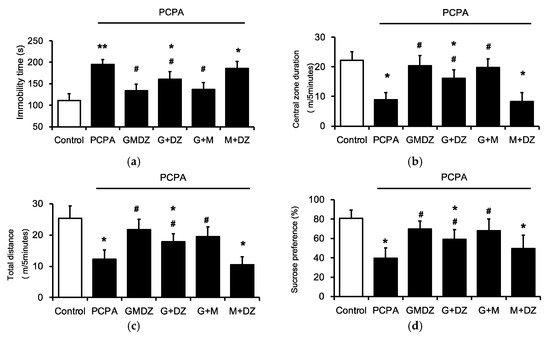
Figure 2. Effects of the one herb-deleted mixture of GMDZ in depression-like behaviors using the PCPA treated rats. (a) The changes of immobility time in FST; (b) the changes of time in central in OFT; (c) the changes of traveling distance in OFT; (d) the changes of sucrose solution consumption (%) in SPT. Data are expressed as mean ± SE (n = 8). * p < 0.05, ** p < 0.01 compared with the normal control; # p < 0.05 compared with vehicle-treated group.
4. Chronic GMDZ Treatment Restores the 5-HTT and BDNF Levels in the Hippocampus of PCPA Treated Rats
To investigate the potential mechanism(s) underlying GMDZ-induced antidepressant effects, authors determined the gene expressions and protein levels of 5-HTT (Figure 3a,b) and BDNF in the hippocampus of PCPA-treated rats (Figure 3c,d). The mRNA and protein levels of 5-HTT were significantly decreased in the PCPA-treated group, which was restored by GMDZ. Additionally, chronic treatment with GMDZ also increased the protein and mRNA levels of BDNF in the hippocampus of PCPA-treated rats.
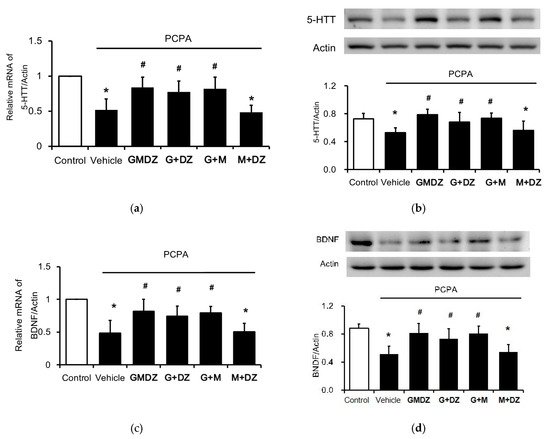
Figure 3. Effects of GMDZ and the one plant-deleted mixture of GMDZ on the expressions of 5-HTT and BDNF in the hippocampus. (a) The mRNA levels of 5-HTT; (b) The protein levels of 5-HTT; (c) the mRNA levels of BDNF; (d) the protein levels of BDNF. Data are expressed as mean ± SE (n = 8). * p < 0.05 compared with the normal control; # p < 0.05 compared with vehicle-treated group.
Same as the results in behavior experiments, G and M or G and DZ treatment significantly restored the mRNA and protein levels of 5-HTT. Moreover, as shown in Figure 3, G and M or G and DZ treatment also restored the protein level and mRNA level of BDNF. However, the treatment of M and DZ did not modify the expressions of 5-HTT and BDNF in the hippocampus. It supports that G played an important role in GMDZ for depression improvement.
5. Effects of Glycyrrhizic Acid on 5-HTT and BDNF Expression in the Corticosterone-Treated H19-7 Cell Line
Authors hypothesized that licorice played a major role in GMDZ mixture, since the antidepressant-like effect in G and M and G and DZ treatments seemed to be more significant than that in the M and DZ treatment group. In addition, long-term exposure to stress or high glucocorticoid levels leads to depression-like behavior in rodents [18]. Therefore, authors investigated the potential mechanism of glycyrrhizic acid (the active component of licorice) for corticosterone-induced stress injury in cells. Authors' results show that the in vitro findings correlate with the vivo results. It showed that chronic exposure of H19-7 cells to corticosterone markedly decreased the gene expressions of 5-HTT (Figure 4a) and BDNF (Figure 4b). Interestingly, glycyrrhizic acid significantly reversed these expressions in a dose-dependent manner.
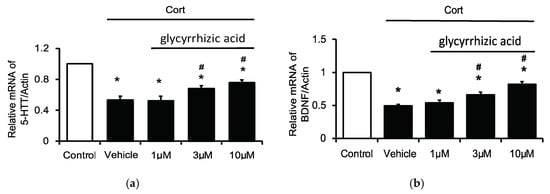
Figure 4. Effects of glycyrrhizic acid (GA) on 5-HTT and BDNF expressions in the corticosterone-treated H19-7 cells. H19-7 cells were incubated under normal differentiating conditions in the presence or absence of corticosterone (Cort) at concentration of 1 μM for five days. Then, cells were respectively incubated with glycyrrhizic acid at 1 μM, 3 μM, or 10 μM for 24 h. (a) The mRNA levels of 5-HTT; (b) the mRNA levels of BDNF. Data are expressed as mean ± SE (n = 8). * p < 0.05 compared to the cells without treatment of corticosterone (control). # p < 0.05 compared with the vehicle-treated group.
References
- Lepine, J.P.; Briley, M. The increasing burden of depression. Neuropsychiatr. Dis. Treat. 2011, 7, 3–7.
- Hansson, S.R.; Mezey, E.; Hoffman, B.J. Serotonin transporter messenger RNA in the developing rat brain: Early expression in serotonergic neurons and transient expression in non-serotonergic neurons. Neuroscience 1998, 83, 1185–1201.
- Molteni, R.; Cattaneo, A.; Calabrese, F.; Macchi, F.; Olivier, J.D.; Racagni, G.; Ellenbroek, B.A.; Gennarelli, M.; Riva, M.A. Reduced function of the serotonin transporter is associated with decreased expression of BDNF in rodents as well as in humans. Neurobiol. Dis. 2010, 37, 747–755.
- Schmidt-Kastner, R.; Wetmore, C.; Olson, L. Comparative study of brain-derived neurotrophic factor messenger RNA and protein at the cellular level suggests multiple roles in hippocampus, striatum and cortex. Neuroscience 1996, 74, 161–183.
- Lesch, K.P.; Bengel, D.; Heils, A.; Sabol, S.Z.; Greenberg, B.D.; Petri, S.; Benjamin, J.; Muller, C.R.; Hamer, D.H.; Murphy, D.L. Association of anxiety-related traits with a polymorphism in the serotonin transporter gene regulatory region. Science 1996, 274, 1527–1531.
- Karege, F.; Perret, G.; Bondolfi, G.; Schwald, M.; Bertschy, G.; Aubry, J.M. Decreased serum brain-derived neurotrophic factor levels in major depressed patients. Psychiatry Res. 2002, 109, 143–148.
- Shirayama, Y.; Chen, A.C.; Nakagawa, S.; Russell, D.S.; Duman, R.S. Brain-derived neurotrophic factor produces antidepressant effects in behavioral models of depression. J. Neurosci. 2002, 22, 3251–3261.
- Qin, F.; Wu, X.A.; Tang, Y.; Huang, Q.; Zhang, Z.J.; Yuan, J.H. Meta-analysis of randomized controlled trials to assess the effectiveness and safety of Free and Easy Wanderer Plus, a polyherbal preparation for depressive disorders. J. Psychiatr. Res. 2011, 45, 1518–1524.
- Wang, Y.; Fan, R.; Huang, X. Meta-analysis of the clinical effectiveness of traditional Chinese medicine formula Chaihu-Shugan-San in depression. J. Ethnopharmacol. 2012, 141, 571–577.
- Yeung, W.F.; Chung, K.F.; Ng, K.Y.; Yu, Y.M.; Ziea, E.T.; Ng, B.F. A meta-analysis of the efficacy and safety of traditional Chinese medicine formula Ganmai Dazao decoction for depression. J. Ethnopharmacol. 2014, 153, 309–317.
- Jun, J.H.; Lee, J.A.; Choi, T.Y.; Yun, K.J.; Lim, H.J.; Lee, M.S. Herbal medicine (Gan Mai Da Zao decoction) for depression: A systematic review protocol. BMJ Open 2014, 4, e003690.
- Spitzer, R.L.; Robins, E.; Endicott, J. Research Diagnostic Criteria (RDC) for a Selected Group of Functional Disorders; New York State Psychiatric Institute: New York, NY, USA, 1978.
- Yang, F.; Qiao, Q.; Gong, Y. Antidepressant effect of gan-maida-zao tang on 30 women with postpartum depression. Shanxi J TCM 2009, 30, 851–852.
- Wu, J. Antidepressant effect of gan-mai-da-zao tang on depression compared with fluoxetine. J. Chin. Physician 2002, 11, 18–19.
- Kurebayashi, L.F.; Turrini, R.N.; Kuba, G.; Shimizu, M.H.; Takiguch, R.S. Chinese phytotherapy to reduce stress, anxiety and improve quality of life: Randomized controlled trial. Rev. Esc. Enferm. USP 2016, 50, 853–860.
- Lou, J.S.; Li, C.Y.; Yang, X.C.; Fang, J.; Yang, Y.X.; Guo, J.Y. Protective effect of gan mai da zao decoction in unpredictable chronic mild stress-induced behavioral and biochemical alterations. Pharm. Biol. 2010, 48, 1328–1336.
- Almeida, R.D.; Manadas, B.J.; Melo, C.V.; Gomes, J.R.; Mendes, C.S.; Graos, M.M.; Carvalho, R.F.; Carvalho, A.P.; Duarte, C.B. Neuroprotection by BDNF against glutamate-induced apoptotic cell death is mediated by ERK and PI3-kinase pathways. Cell Death Differ. 2005, 12, 1329–1343.
- McEwen, B.S. Stress and hippocampal plasticity. Annu. Rev. Neurosci. 1999, 22, 105–122.
More
Information
Subjects:
Medicine, Research & Experimental
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
876
Revisions:
3 times
(View History)
Update Date:
08 Feb 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




