
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Lisa van der Water | + 1854 word(s) | 1854 | 2022-01-11 09:00:16 |
Video Upload Options
Clavicle fractures are commonly seen in the pediatric and adolescent populations. In contrast, congenital pseudarthrosis of the clavicle is rare. Although both conditions may present with similar signs and symptoms, especially in the very young, clear differences exist. Clavicle fractures are often caused by trauma and are tender on palpation, while pseudarthrosis often presents with a painless protuberance on the clavicle, which becomes more prominent as the child grows. Its presence may only become apparent after trauma, as it is usually asymptomatic.
1. Epidemiology
1.1. Anatomy
Development of Clavicle
1.2. Trauma Mechanism
1.3. Development of Pseudarthrosis
1.4. Classification of Pseudarthrosis
2. Treatment
2.1. Fractures
2.1.1. Non-Operative Treatment

2.1.2. Operative Treatment

2.2. Pseudarthrosis
2.2.1. Non-Operative Treatment
The majority of patients are treated conservatively (i.e., observation only, no interventions), especially if they experience minimal symptoms and do not have esthetic complaints due to the protuberance [6][10]. Outcomes after non-operative treatment are generally excellent; most patients do not experience any pain, discomfort or limited range of motion .
2.2.2. Operative Treatment
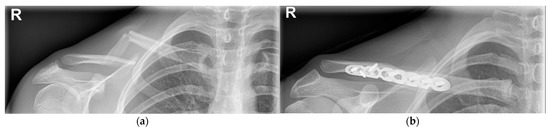
Indications for surgical treatment are progressive pain, functional limitation and late-onset thoracic outlet syndrome [10]. However, most operations are performed for cosmetic reasons [10]. Surgery is considered in Kite type I patients, where the fragments are less than 1 cm apart [10][17]. A displacement greater than 1 cm has a much higher incidence of nonconsolidation and complications after surgery [10][17]. Several surgical treatment options are used: resection of the focus of the pseudarthrosis with the option of using a bone graft, osteosynthesis or both [10]. For stabilization, different techniques are used: an intramedullary Kirschner-wire, plate and screws, screws only, a Steinmann intramedullary pin or external fixation [10][17]. Post-operative treatment includes immobilization with a Velpeau sling or Desault bandage for four to six weeks [2]. Outcomes after surgical treatment are generally successful and complications are rare [10]. Non-union is the most common complication and is often an indication for revision surgery .
2.3. Revision Surgery
References
- van der Meijden, O.A.; Gaskill, T.R.; Millett, P.J. Treatment of clavicle fractures: Current concepts review. J. Shoulder Elb. Surg. 2012, 21, 423–429.
- van Tassel, D.; Owens, B.D.; Pointer, L.; Moriatis Wolf, J. Incidence of clavicle fractures in sports: Analysis of the NEISS Database. Int J. Sports Med. 2014, 35, 83–86.
- Ellis, H.B.; Li, Y.; Bae, D.S.; Kalish, L.A.; Wilson, P.L.; Pennock, A.T.; Nepple, J.J.; Willimon, S.C.; Spence, D.D.; Pandya, N.K.; et al. Descriptive Epidemiology of Adolescent Clavicle Fractures: Results From the FACTS (Function after Adolescent Clavicle Trauma and Surgery) Prospective, Multicenter Cohort Study. Orthop J. Sports Med. 2020, 8.
- Luo, T.D.; Ashraf, A.; Larson, A.N.; Stans, A.A.; Shaughnessy, W.J.; McIntosh, A.L. Complications in the treatment of adolescent clavicle fractures. Orthopedics 2015, 38, e287–e291.
- Hughes, K.; Kimpton, J.; Wei, R.; Williamson, M.; Yeo, A.; Arnander, M.; Gelfer, Y. Clavicle fracture nonunion in the paediatric population: A systematic review of the literature. J. Child. Orthop. 2018, 12, 2–8.
- O’Neill, B.J.; Molloy, A.P.; Curtin, W. Conservative Management of Paediatric Clavicle Fractures. Int. J. Pediatr. 2011, 2011, 172571.
- Yenigül, A.E.; Yenigül, N.N.; Başer, E.; Özelçi, R. A retrospective analysis of risk factors for clavicle fractures in newborns with shoulder dystocia and brachial plexus injury: A single-center experience. Acta Orthop. Traumatol. Turc. 2020, 54, 609–613.
- Beall, M.H.; Ross, M.G. Clavicle fracture in labor: Risk factors and associated morbidities. J. Perinatol. 2001, 21, 513–515.
- Linder, N.; Linder, I.; Fridman, E.; Kouadio, F.; Lubin, D.; Merlob, P.; Yogev, Y.; Melamed, N. Birth trauma-risk factors and short-term neonatal outcome. J. Matern. Neonatal Med. 2013, 26, 1491–1495.
- de Figueiredo, M.J.P.S.S.; Dos Reis Braga, S.; Akkari, M.; Prado, J.C.L.; Santili, C. Congenital pseudarthrosis of the clavicle. Rev. Bras. Ortop. 2012, 47, 21–26.
- O’Neill, B.J.; Hirpara, K.M.; O’Briain, D.; McGarr, C.; Kaar, T.K. Clavicle fractures: A comparison of five classification systems and their relationship to treatment outcomes. Int. Orthop. 2011, 35, 909–914.
- Alldred, A.J. Congenital pseudarthrosis of the clavicle. J. Bone Jt. Surg. Br. 1963, 45, 312–319.
- Price, B.D.; Price, C.T. Familial congenital pseudoarthrosis of the clavicle: Case report and literature review. Iowa Orthop. J. 1996, 16, 153–156.
- Toledo, L.C.; MacEwen, G.D. Severe complication of surgical treatment of con-genital pseudarthrosis of the clavicle. Clin. Orthop. Relat. Res. 1979, 139, 64–67.
- Shim, J.S.; Chang, M.J. Congenital pseudarthrosis of the clavicle—Report of 4 cases treated with surgical methods. J. Korean Orthop. Assoc. 2008, 43, 396–399.
- Persiani, P.; Molayem, I.; Villani, C.; Cadilhac, C.; Glorion, C. Surgical treatment of congenital pseudarthrosis of the clavicle: A report on 17 cases. Acta Orthop. Belg. 2008, 74, 161–166.
- Kite, J.H. Congenital pseudarthrosis of the clavicle. South. Med. J. 1968, 61, 703–710.
- Kihlström, C.; Möller, M.; Lönn, K.; Wolf, O. Clavicle fractures: Epidemiology, classification and treatment of 2 422 fractures in the Swedish Fracture Register; an observational study. BMC Musculoskelet. Disord. 2017, 18, 82.
- Andersen, K.; Jensen, P.O.; Lauritzen, J. Treatment of clavicular fractures. Figure-of-eight bandage versus a simple sling. Acta Orthop. Scand. 1987, 58, 71–74.
- Randsborg, P.H.; Fuglesang, H.F.; Røtterud, J.H.; Hammer, O.L.; Sivertsen, E.A. Long-term patient-reported outcome after fractures of the clavicle in patients aged 10 to 18 years. J. Pediatr. Orthop. 2014, 34, 393–399.
- Schulz, J.; Moor, M.; Roocroft, J.; Bastrom, T.P.; Pennock, A.T. Functional and radiographic outcomes of nonoperative treatment of displaced adolescent clavicle fractures. J. Bone Jt. Surg. Am. 2013, 95, 1159–1165.
- Leal-Oliva, A.; Mora-Ríos, F.G.; Mejía-Rohenes, C.; López-Marmnolejo, A.; Acevedo-Cabrera, M.J. Acortamiento relativo de clavícula en fracturas pediátricas: Su importancia en la decisión del tratamiento conservador . Acta Ortop. Mex. 2014, 28, 82–87.
- Swarup, I.; Maheshwer, B.; Orr, S.; Kehoe, C.; Zhang, Y.; Dodwell, E. Intermediate-Term Outcomes Following Operative and Nonoperative Management of Midshaft Clavicle Fractures in Children and Adolescents: Internal Fixation May Improve Outcomes. JB JS Open Access 2021, 6, e20.00036.
- McGraw, M.A.; Mehlman, C.T.; Lindsell, C.J.; Kirby, C.L. Postnatal growth of the clavicle: Birth to 18 years of age. J. Pediatr. Orthop. 2009, 29, 937–943.
- Riiser, M.O.; Molund, M. Long-term Functional Outcomes and Complications in Operative Versus Nonoperative Treatment for Displaced Midshaft Clavicle Fractures in Adolescents: A Retrospective Comparative Study. J. Pediatr. Orthop. 2021, 41, 279–283.
- Scott, M.L.; Baldwin, K.D.; Mistovich, R.J. Operative Versus Nonoperative Treatment of Pediatric and Adolescent Clavicular Fractures. JBJS Rev. 2019, 7, e5.
- Mukhtar, I.A.; Yaghmour, K.M.; Ahmed, A.F.; Ibrahim, T. Flexible intramedullary nailing versus nonoperative treatment for paediatric displaced midshaft clavicle fractures. J. Child. Orthop. 2018, 12, 104–110.
- McIntosh, A.L. Surgical treatment of adolescent Clavicle Fractures: Results and complications. J. Pediatr. Orthop. 2016, 36 (Suppl. 1), S41–S43.
- Song, M.H.; Yun, Y.H.; Kang, K.; Hyun, M.J.; Choi, S. Nonoperative versus operative treatment for displaced midshaft clavicle fractures in adolescents: A comparative study. J. Pediatr. Orthop. Part B 2019, 28, 45–50.
- Fanter, N.J.; Kenny, R.M.; Baker, C.L., III; Baker, C.L., Jr. Surgical treatment of clavicle fractures in the adolescent athlete. Sports Health 2015, 7, 137–141.
- Pecci, M.; Kreher, J.B. Clavicle fractures. Am. Fam. Physician 2008, 77, 65–70.
- Kim, H.Y.; Yang, D.S.; Bae, J.H.; Cha, Y.H.; Lee, K.W.; Choy, W.S. Clinical and Radiological Outcomes after Various Treatments of Midshaft Clavicle Fractures in Adolescents. Clin. Orthop. Surg. 2020, 12, 396–403.
- Lazarides, S.; Zafiropoulos, G. Conservative treatment of fractures at the middle third of the clavicle: The relevance of shortening and clinical outcome. J. Shoulder Elb. Surg. 2006, 15, 191–194.
- Hill, J.M.; McGuire, M.H.; Crosby, L.A. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J. Bone Jt. Surg. Br. 1997, 79, 537–539.
- Herzog, M.M.; Whitesell, R.C.; Mac, L.M.; Jackson, M.L.; Culotta, B.A.; Axelrod, J.R.; Busch, M.T.; Willimon, S.C. Functional outcomes following non-operative versus operative treatment of clavicle fractures in adolescents. J. Child. Orthop. 2017, 11, 310–317.
- Bae, D.S.; Shah, A.S.; Kalish, L.A.; Kwon, J.Y.; Waters, P.M. Shoulder motion, strength, and functional outcomes in children with established malunion of the clavicle. J. Pediatr. Orthop. 2013, 33, 544–550.
- Vander Have, K.L.; Perdue, A.M.; Caird, M.S.; Farley, F.A. Operative versus nonoperative treatment of midshaft clavicle fractures in adolescents. J. Pediatr. Orthop. 2010, 30, 307–312.
- Matsumura, N.; Ikegami, H.; Nakamichi, N.; Nakamura, T.; Nagura, T.; Imanishi, N.; Aiso, S.; Toyama, Y. Effect of shortening deformity of the clavicle on scapular kinematics: A cadaveric study. Am. J. Sports Med. 2010, 38, 1000–1006.
- Ledger, M.; Leeks, N.; Ackland, T.; Wang, A. Short malunions of the clavicle: An anatomic and functional study. J. Shoulder Elb. Surg. 2005, 14, 349–354.
- Pandya, N.K.; Namdari, S.; Hosalkar, H.S. Displaced clavicle fractures in adolescents: Facts, controversies, and current trends. J. Am. Acad. Orthop. Surg. 2012, 20, 498–505.
- Parry, J.A.; Van Straaten, M.; Luo, T.D.; Simon, A.L.; Ashraf, A.; Kaufman, K.; Larson, A.N.; Shaughnessy, W.J. Is There a Deficit After Nonoperative Versus Operative Treatment of Shortened Midshaft Clavicular Fractures in Adolescents? J. Pediatr. Orthop. 2017, 37, 227–233.
- Odorizzi, M.; Fitzgerald, M.; Gonzalez, J.; Giunchi, D.; Hamitaga, F.; De Rosa, V. Posttraumatic Pseudoarthrosis of a Clavicle Fracture in an 11-Year-Old Girl: A Case Report and Analysis.. Case Reports in Orthopedics 2020, 2020, 4069431-5.
- Da Costa, J.C. Modern Surgery - Chapter 34. Bandages; W.B. Saunders: Philadelphia, PA, USA, 1903; 11.
- Dzupa, V.; Bartonicek, J.; Zidka, M. Fracture of the clavicle after surgical treatment for congenital pseudarthrosis. Med Sci Monit 2004, 10.
- Pennock, A.T.; Edmonds, E.W.; Bae, D.S.; Kocher, M.S.; Li, Y.; Farley, F.A.; Ellis, H.B.; Wilson, P.L.; Nepple, J.; Gordon, J.E.; et al. Adolescent clavicle nonunions: Potential risk factors and surgical management. J. Shoulder Elb. Surg. 2018, 27, 29–35.
- Kubiak, R.; Slongo, T. Operative treatment of clavicle fractures in children: A review of 21 years. J. Pediatr. Orthop. 2002, 22, 736–739.




