Wound healing has been intensely studied in order to develop an "ideal" technique that achieves expeditious recovery and reduces scarring to the minimum, thus ensuring function preservation. The classic approach to wound management is represented by topical treatments, such as antibacterial or colloidal agents, in order to prevent infection and promote a proper wound-healing process. Nanotechnology studies submicroscopic particles (maximum diameter of 100 nm), as well as correlated phenomena. Metal nanoparticles (e.g., silver, gold, zinc) are increasingly being used in dermatology, due to their beneficial effect on accelerating wound healing, as well as treating and preventing bacterial infections. Other benefits include: ease of use, less frequent dressing changes and a constantly moist wound environment. This entry highlights recent findings regarding nanoparticle application in wound management.
1. Definition and Classification
Nanotechnology studies the synthesis, structure and dynamic of atomic and molecular nanometric particles (maximum diameter of 100 nm), termed nanoparticles, upon which nanoproducts are built
[1]. By downscaling to nanometric range, a particle’s surface increases exponentially, whereas its volume decreases, which leads to particular physico-chemical characteristics that account for numerous medical applications. Dynamic light scattering (DLS), fluorescence correlation spectroscopy (FCS) and Raman scattering (RS) offer information regarding the hydrodynamic size distribution of nanoparticles, whereas circular dichroism (CD), Infrared spectroscopy (IR) and Mass spectroscopy (MS) help in investigating their structure, conformation and surface characteristics. In addition, electron microscopy in general and transmission electron microscopy (TEM) and scanning electron microscopy (SEM) in particular, can achieve resolutions of less than 1 nm, thus making them valuable investigational tools employed in studying the properties and dynamics (i.e., diffusion, adherence) of nanomaterials. Through TEM, the morphology of nanomaterials can be investigated, whereas SEM recreates a superficial image of the nanomaterial, thus being solely employed in the study of dimensions and overall shape
[2].
The size and shape of nanoparticles are key properties that determine their biological efficiency, by influencing active substance delivery (carrier circulation), penetrability (either directly through cell membranes or through phagocytosis) and cellular responses (receptor recognition)
[2][3][4].
Due to their antibacterial properties and low toxicity profile, metal nanoparticles such as silver, gold and zinc represent ideal candidates for integration in wound dressings
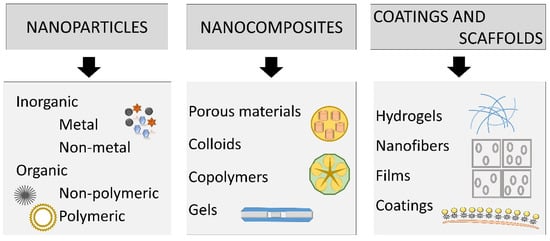
[5]. The main types of nanomaterials used for wound treatment are represented by nanoparticles, nanocomposites, coatings and scaffolds (
Figure 1).
Figure 1. Main types of nanomaterials which can be used for wound treatment.
Nanomaterials for tissue regeneration can be developed under different structures: nanoparticles, nanospheres, nanocapsules, nanoemulsions, nanocarriers and nanocolloids
[1].
Two principal types of nanoparticles (NPs) are commonly employed in wound therapy: (1) NPs that possess intrinsic characteristics that aid wound closure; (2) NPs used as delivery vectors for therapeutic agents. The former can be divided into metallic/metal oxide nanomaterials and nonmetallic nanomaterials (
Figure 1)
[6].
Regarding metallic and metal oxide nanoparticles, the most studied are silver, gold and zinc compounds due to their unique properties: antibacterial activity and reduced penetration into the skin. Their effectiveness, as well as toxicity, relies on key features, for example: dimension and architecture (smaller particles are more biologically active), surface functionalization, zeta potential and polydispersity index
[7]. Zeta potential estimates the particle surface charge which influences receptor binding capacity as well as the penetrability of cellular barriers
[3]. Other particle surface characteristics, such as porosity, chemical structure and heterogeneity, hydrolytic stability, determine the biological behavior of nanomaterials, including their interactions with other biomolecules, which may influence their biodistribution
[4][8].
Nanospheres are small polymeric matrix systems composed of a fixed porous polymer onto which active substances (e.g., aminoacids, minerals or organic substances) can bind. As a result, active compounds become more stable and exhibit increased biocompatibility and improved pharmaceutical properties
[1].
Nanocapsules are capable of enclosing an active agent within their structure, releasing it at a specific time, ensuring a more controlled delivery. They can also improve the penetration of active ingredients into deeper layers of the dermis. On the other hand, the effectiveness of the substances may be reduced
[1].
Nanoemulsions represent homogenous, thermally stable oil-in-water emulsions with a droplet size of maximum 100 nm that also contain surfactant and can easily incorporate biologically active substances, preventing their sedimentation. They are also characterized by high solubilization capacity and fluidity and decreased viscosity. Their disadvantage would be the uncontrolled accumulation of active substances in reticular dermis or subcutaneous fat
[1].
Nanocarriers structurally resemble liposomes, but contain synthetic, non-ionic surfactants. In addition, they express surface receptors capable of binding to specific loci, thus increasing the efficacy of the active agent, while also minimizing any adverse reactions
[1].
Nanocolloids are composed of 1.5 to 5 nm non-ionic metal nanoparticles highly scattered in demineralized water due to their perpetual Brownian motion which allows them to penetrate eukaryotic and prokaryotic cells, thus exhibiting antimicrobial activity. Moreover, they are characterized by good electrical conductivity, being positively charged particles
[1].
2. Nanoparticles
2.1. Silver Nanoparticles
Silver nanoparticles (AgNPs) might overcome the limitations of standard silver compounds. Due to their increased surface-to-volume ratio, AgNPs are more potent at reduced concentrations, thus lowering their toxicity. Pure silver nanoparticles can modulate anti-inflammatory cytokine release, in order to promote rapid wound closure without increasing scarring
[6]. By inducing the differentiation of myofibroblasts from normal fibroblasts, AgNPs promote wound contractility, thus accelerating the healing process
[8]. Moreover, AgNPs stimulate epidermal re-epithelialization through the proliferation and relocation of keratinocytes
[8]. However, Szmyd et al. reported that higher concentrations of AgNPs decrease keratinocyte viability, metabolism, as well as migration and differentiation of these cells, through the activation of caspase 3 and 7 (proteases involved in programmed cell death) and dose-dependent DNA damage
[9]. In order to reduce side effects, silver nanoparticles can be used in low doses along with antimicrobial drugs to achieve increased efficiency. This nanomaterial proved a high bacteria-killing performance against Gram negative pathogens and promoted wound healing
[10]. Similar results have been reported by Holban et al. who coated polyester-nylon dressings with AgNPs which interfered with bacterial colonization as well as biofilm synthesis, while maintaining a low toxicity profile
[11].
The main anti-bacterial mechanism of AgNPs is creating sulfuric bonds with either bacterial cell membrane proteins or thiol groups of various enzymes, especially those involved in the respiratory chain, thus leading to apoptosis
[8]. Moreover, since DNA contains sulfurous and phosphorous bonds, AgNPs can interfere with DNA synthesis during cell division, thus inhibiting bacterial multiplication
[8].
Moreover, silver nanoparticles were used for numerous clinical trials in the therapy of wounds, especially burns and chronic wounds (i.e., diabetic ulcers)
[12]. Currently, there are some commercially available dressings containing AgNPs. Such example is Acticoat©-wound dressing containing AgNPs with average size of 15 nm. The proved properties of Anticoat© are: wound healing, infection reduction on the site of the wound, and pain reduction, aspects observed in most tested patients. However, this coating is still under investigation for the therapy of burns. Recent clinical trials concluded that Anticoat© may be efficient in avoiding infections in burns when applied together with silver sulphadiazine and chlorhexidine digluconate cream
[13].
2.2. Gold Nanoparticles
Gold nanoparticles (AuNPs) represent a solid option when it comes to wound therapy due to their chemical stability and capacity of absorbing near infrared light, while, at the same time, being relatively easy to synthetize
[1]. Moreover, by tuning the surface plasmon resonance, AuNP gels gain thermoresponsiveness, as described by Arafa et al., who demonstrated their antibacterial and healing properties both in vitro and in vivo, backed by histopathologic examinations
[14]. AuNPs can either directly target the bacterial cell wall, or they can bind to bacterial DNA, blocking the double-helix from uncoiling during replication or transcription, thus exerting bactericidal and bacteriostatic properties.
2.3. Zinc Oxide Nanoparticles
Zinc oxide nanoparticles (ZnONPs) represent a reliable antibacterial agent, by inducing bacterial cell membrane perforations. Moreover, when incorporated in hydrogel-based wound dressings
[6], the overall contact time is increased, promoting keratinocyte migration, thus improving re-epithelialization
[8]. In addition, in a recent study, a microporous chitosan hydrogel/ZnONPs dressing presented a high capacity of absorbing wound exudates and enabled the formation of hemostatic blood clots, while also displaying antibacterial properties with little cytotoxicity
[15].
However, the intrinsic high toxicity of these material limit their usage in wound healing therapies
[6]. For example, high concentrations of ZnONPs are associated with mitochondrial dysfunction in keratinocytes, causing the release of lactate dehydrogenase. Moreover, ZnONPs produce reactive oxygen species, while also inhibiting the expression of superoxide dismutase and glutathione peroxidase genes in human keratinocytes, inducing cell membrane oxidative stress and apoptosis. In addition, it has been described that ZnONPs generate carcinogenic transformations
[16].
In a skin wound mouse model, ZnONPs achieve successful wound closure and aesthetic wound healing, suggesting their capability as an effective antimicrobial tissue adhesive
[17].
3. Nanocomposites or Composite Nanoparticles
Artificial synthesis of NPs is limited due to the fact that it involves high costs, energy consumption and additional resources to dispose of toxic by-products. Therefore, non-polluting, cheap and renewable sources such as plant extracts have gained popularity as they contain alkaloids, phenols, amino acids and proteins which are employed in the reduction and stabilization of Ag ions in AgNPs.
Gelatin is a natural, biodegradable, highly biocompatible, non-immunogenic polymer, rich in hydroxyproline that can reduce AgNO
3 in situ through the hydroxyl groups. Moreover, its non-polar aminoacids help stabilize AgNPs. As a result, Ye et al. developed gelatin-chitosan-Ag, a new composite with a high density of pores with diameters of 100–250 µm, in which AgNPs were initially mixed with chitosan, cross-linked with tannic acid and cryodesiccated. The compound exhibited wound healing and anti-bacterial properties, while maintaining low cytotoxicity
[18]. In addition, Shao et al. used
Barleria gibsoni aqueous leaves to synthetize a ZnONPs gel efficient in treating both Gram-positive and Gram-negative infected burns
[19].
Polymeric nanomaterial therapy employs polymeric nanoparticles (e.g., chitosan) as wound dressings or as delivery vectors due to the fact that they exhibit antibacterial and re-epithelialization properties
[6]. Biopolymers are biocompatible polymeric networks that can absorb significant quantities of liquid, while also ensuring a moist wound environment
[20].
Chitosan is a hydrophilic biopolymer commonly extracted from the exoskeleton of crustacean arthropods, characterized by high bioavailability and low toxicity, in addition to being one of the few polymers with antibacterial properties
[20]. Chemically, this biopolymer is a linear polysaccharide containing D-glucosamine and N-acetyl glucosamine units. Apart from its affinity to metals, proteins and dyes, chitosan can also form complexes with anions, such as sulfate and phosphate, due to its cationic nature
[21]. Moreover, its degradation products can stimulate synthesis of extracellular matrix components
[20].
Various forms of chitosan have been investigated for wound-healing therapies, such as hydrogels, membranes, films, sponges and scaffolds
[21]. Chitosan nanoparticles are characterized by superior permeability, antibacterial properties and immune modulation, while also being non-toxic to human cells. Polydopamine nanoparticles were loaded with ciprofloxacin which was released on demand through near-infrared light stimulation, even though the hydrogel complex exhibited minimal leakage under physiological conditions
[22].
Hernandez Martinez et al. described a nanocomposite of AuNPs, chitosan and calreticulin for the therapy of diabetic lesions. Calreticulin is a 46 kDa calcium-binding protein found in the endoplasmic reticulum which regulates cytosolic and endoplasmic reticulum calcium levels. In addition, calreticulin acts as a molecular chaperone that controls the proper folding of proteins. The gold nanoparticles-chitosan-calreticulin composite promoted the growth, migration and differentiation of keratinocytes, fibroblasts and endothelial cells, without affecting cell viability, in vitro as well as in vivo. Moreover, the histological examination described granulation, re-epithelization and increased collagen synthesis
[23].
Bacterial cellulose is a biopolymer synthetized by various microorganisms, such as
Acetobacter,
Pseudomonas,
Salmonella, through carbohydrate fermentations. Bacterial cellulose represents an excellent skin substitute due to its physico-chemical traits, such as very high surface area per unit, increased biocompatibility, hydrophilicity and nontoxicity. Bacterial nanocellulose is characterized by three-dimensional porous networks capable of retaining a high quantity of water, thus ensuring a damp environment, proper for wound healing
[24]. Khalid et al. analyzed the healing properties of bacterial cellulose combined with ZnONPs and discovered that the added ZnONPs granted antibacterial properties
[25]. Moniri et al. combined bacterial nanocellulose obtained from the fermentation of Gram-negative
Gluconacetobacter xylinus, with silver nanoparticles (BNC-Ag). The nanocomposite improved wound healing and reduced
Staphylococcus aureus colonization in vitro
[26].
Nano-Carriers for Wound Healing
Nanomaterials can also act as carriers for therapeutic agents, controlling their release. Nitric oxide exhibits a crucial role in inflammatory pathways, cellular growth, angiogenesis and extracellular matrix deposition and remodeling. In addition, nitric oxide exhibits wide spectrum antibacterial properties, while also interfering with biofilm synthesis. As a result, many studies have tried to produce a delivery system with high loading capacity, controlled release and reduced cytotoxicity
[6]. Nitric oxide-releasing poly(lactic-co-glycolic acid)-polyethylenimine nanoparticles were designed to provide prolonged nitric oxide release, antibacterial efficacy against methicillin-resistant
Staphylococcus aureus and
Pseudomonas aeruginosa, as well as accelerated wound closure in vivo
[27].
Curcumin, the dynamic component of the nutritional spice turmeric, also presented interest due to its antibiotic and antioxidant properties, as well as stimulating the production of granulation tissue. A recent study attempted to increase curcumin’s poor solubility by encapsulating it into a saline-hydrogel nanoparticle vector, and the results demonstrated in vitro efficacy against methicillin-resistant
Staphylococcus aureus and enhanced wound closure activity
[28]. Ghaffari et al. stated that both gel and ointment preparations containing curcumin-Ampicillin solid lipid nanoparticles exhibited antibacterial effects, while also increasing wound closure rate compared to control and placebo groups, both in vitro and in vivo, without additional toxicity
[29]. In addition, in a mouse model experiment, Moradi et al. studied the associated effect of pulse photo-bio-modulation with curcumin loaded super-paramagnetic iron oxide nanoparticles and reported accelerated wound healing and an important reduction in
Staphylococcus aureus colonies
[30].
4. Coatings and Scaffolds
Another application of nanomaterials is the production of scaffolds that mimic the properties of extracellular matrix. Several techniques are used to produce them, such as electro-spinning, self-assembly and phase separation. The most employed is electro-spinning which creates porous polymeric nanofibers that can be used as hybrid scaffolds for the adherence and development of fibroblasts in wounds
[6]. Other nano-polymers, such as dendrimers, can exhibit anti-inflammatory properties, while also forming networks that can incorporate antibacterial agents (e.g., silver)
[31].
Using a porcine model of superficial partial thickness wounds, Haik et al. studied the healing properties of a polymer nanofiber dressing applied by a mobile handheld electrospinning device. Regarding safety (risk of infection, delayed healing) the results were similar to the traditional paraffin tulle gras dressing. The non-touch technique and the ease of application represent advantages of this therapeutic option
[32].
Electrospun chitosan-poly-vinyl alcohol nanofibrous blend scaffolds were applied to treat models of diabetic wounds in rats, showing increased healing rates compared with controls
[33].
The in vivo study in Wistar rats of a electrospun nanofiber membrane enhanced with silver nanoparticles showed multiple favorable effects: low cytotoxicity, long-term antibacterial activity, reduced inflammation and enhanced wound healing
[34].
An electrospun composite scaffold with curcumin showed low cytotoxicity and anti-oxidant effect in vitro, as well as enhanced wound healing in vivo, in a full-thickness dermal model for Wistar rats
[35].
Other nanoscale system compounds attempted to deliver growth factors, such as recombinant human epidermal growth factor, in order to stimulate the healing of full-thickness diabetic wounds. However, their application was limited by the highly proteolytic environment, as well as the down-regulation of the associated growth factor receptors and signaling molecules in chronic lesions
[36]. In contrast, other authors described better results when using basic fibroblast growth factor (bFGF). For example, Zhang et al. described a hydrogel that employed Ca
2+ as a cross-linker between carboxyl groups (–COO) and that was capable of releasing preloaded bFGF. They observed that both calcium and bFGF stimulated fibroblast growth and differentiation, and that the effect was more potent in the early phases of re-epithelialization, inducing wound contraction, both in vitro and in vivo. In addition the hydrogel presented two profiles of bFGF release: an initial burst which accounted for approximately 40% in the first 12 h and a secondary, prolonged phase, which ensured a constant release of bFGF over 8 days. These dynamics suggest that the compound achieves increased levels and stability of local bFGF over a longer period of time
[37].
Furthermore, electro-spun nano-fibrous meshes have been used as networks for gene encapsulation in wound-dressing materials. Gene-activated matrix therapy, which associates gene therapy and tissue engineering, has the advantage of increasing or decreasing the expression of a target gene involved in regeneration. DNA is also more stable compared to growth factors. However, more studies need to be performed in order to obtain additional data about gene therapy effectiveness, bioavailability and safety in the presence of wound bacterial colonization
[6].
The multiple properties of nanomaterials regarding antimicrobial effects, the stimulation of wound healing by inducing angiogenesis, re-epithelialization, granulation and/or collagen synthesis, as well as their role in the prevention of abnormal scarring represent advantages compared to standard treatment and arguments towards their use in clinical practice (Table 1).
Table 1. Properties of nanomaterials developed for wound management. bFGF—basic fibroblast growth factor.
| Material |
Properties |
References |
| Antibacterial |
Stimulation of Wound Healing 1 |
Prevention of Abnormal Scarring |
| Nanoparticles |
Silver nanoparticles |
+ |
+ |
+ |
[6][8][10][11] |
| Gold nanoparticles |
+ |
+ |
Unknown |
[14][8][38] |
| Zinc oxide nanoparticles |
+ |
+ |
Unknown |
[6][15][8][39] |
| Composite nanoparticles Eg. chitosan nanoparticles, nanocellulose |
+ |
+ |
+ |
[6][40][18][20][41][42][43][22][23][44][45][25][26] |
| Nanocarriers |
Eg. Nitric oxide-releasing poly(lactic-co-glycolic acid)-polyethylenimine nanoparticles, curcumin loaded super-paramagnetic iron oxide |
+ |
+ |
Unknown |
[27][46][28][29][30] |
| Coatings and Scaffolds |
Eg. hydrogel preloaded with bFGF, Hydrogels reinforced with AgNPs |
++ |
++ |
Unknown |
[47][48][49] |