1000/1000
Hot
Most Recent

| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Anna Kurek-Górecka | + 1074 word(s) | 1074 | 2022-01-04 07:05:16 | | | |
| 2 | Catherine Yang | + 1 word(s) | 1075 | 2022-01-13 01:50:48 | | |
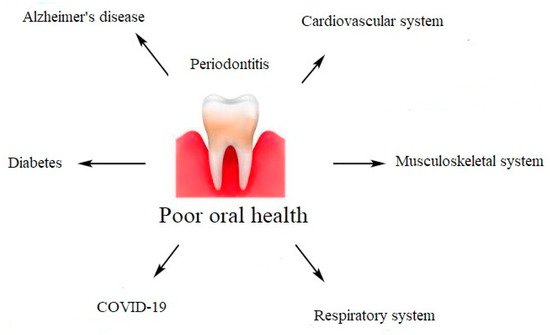
Periodontal diseases are not just simple bacterial infections, but rather complex diseases of multifactorial complexity. The connection between the subgingival microbes, the host immune, and inflammatory responses seems to be very clear. The mechanisms explaining the association between chronic periodontal disease and systemic diseases include a direct and an indirect route. The direct route results in ulceration in the lining of periodontal pockets, which can become a passage for bacteria into the systemic circulation. It leads to bacteremia, which allows bacteria to settle in distant organs aggravating existing disease conditions. The indirect route is based on the fact that chronic periodontal disease, being a significant source of inflammation, may play a role in other disease conditions in which inflammation is a major component.