Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Hetal Desai | + 2354 word(s) | 2354 | 2021-12-13 05:05:38 | | | |
| 2 | Jessie Wu | Meta information modification | 2354 | 2022-01-10 02:38:50 | | | | |
| 3 | Jessie Wu | + 5 word(s) | 2359 | 2022-01-11 07:09:56 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Desai, H. Minimally Invasive Therapies for the Dental Caries. Encyclopedia. Available online: https://encyclopedia.pub/entry/17892 (accessed on 07 February 2026).
Desai H. Minimally Invasive Therapies for the Dental Caries. Encyclopedia. Available at: https://encyclopedia.pub/entry/17892. Accessed February 07, 2026.
Desai, Hetal. "Minimally Invasive Therapies for the Dental Caries" Encyclopedia, https://encyclopedia.pub/entry/17892 (accessed February 07, 2026).
Desai, H. (2022, January 07). Minimally Invasive Therapies for the Dental Caries. In Encyclopedia. https://encyclopedia.pub/entry/17892
Desai, Hetal. "Minimally Invasive Therapies for the Dental Caries." Encyclopedia. Web. 07 January, 2022.
Copy Citation
Resin infiltrants (RI) are low-viscosity triethylene glycol dimethacrylate (TEGDMA) based resins that exhibit high caries permeating ability and a high degree of conversion (DC).
dental caries
minimally invasive
1. Resin Infiltration for the Management of Carious Lesions
1.1. Analysis of Considerations for Use in Non-Cavitated and Cavitated Proximal Lesions
Resin infiltration has been developed as a minimally-invasive intervention to bridge the gap between the “wait and watch” and “drill and fill” approach to the treatment of interproximal caries [1]. Resin infiltrants (RI) are low-viscosity triethylene glycol dimethacrylate (TEGDMA) based resins that exhibit high caries permeating ability and a high degree of conversion (DC) [2] (Figure 1).
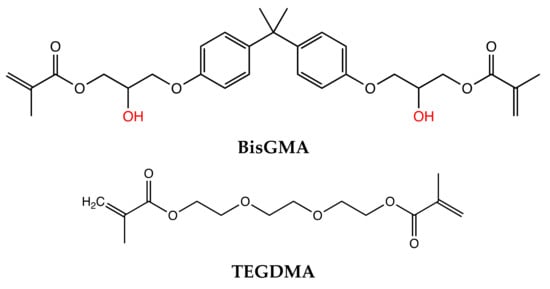
Figure 1. Chemical Structure of resin monomers. Bisphenol A-glycidyl methacrylate (BisGMA) and Triethylene glycol dimethacrylate (TEGDMA).
RIs penetrate the demineralized enamel lesions and occlude the inter-crystalline spaces after polymerization, resulting in the formation of a polymer framework that micromechanically interlocks the remaining enamel prisms and acts as a barrier for hydrogen ions, inhibiting further demineralization and arresting the progress of caries [2][3][4][5] (Figure 2).
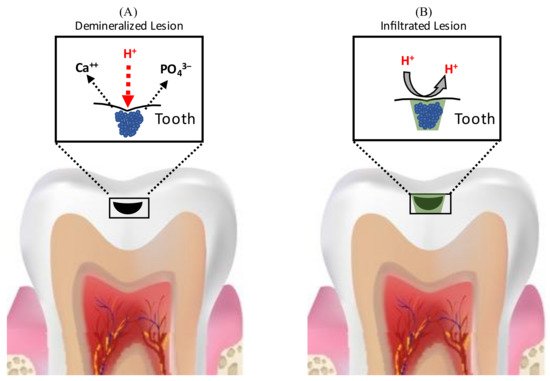
Figure 2. Schematic representation of caries-arresting effect of resin infiltration. (A) Demineralization of enamel due to acids, resulting in the formation of enamel porosities (B) Resin infiltrants penetrate the demineralized enamel lesions and occlude the inter-crystalline spaces after polymerization, resulting in the formation of a polymer framework that acts as a barrier for hydrogen ions, inhibiting further demineralization and arresting the progress of caries.
The ability of the Resin infiltrant (RI) to inhibit caries progression depends on its penetration coefficient (PC) (the rate at which a liquid penetrates a capillary or porous bed; PC is directly related to surface tension and inversely related to the contact angle and liquid viscosity) and penetration depth [6]. Penetration in enamel lesions may depend mainly on the viscosity of the RIs, however, penetration in dentinal lesions may depend on both viscosity and hydrophilicity of the material. Research investigating the impact of hydrophilicity of RIs on their ability to infiltrate dentinal lesions is lacking. Attempts have been made to enhance the infiltration ability of methacrylate-based resins by altering their monomer chemistry and adding solvents. In terms of chemistry, owing to its low viscosity, resins with high triethylene glycol dimethacrylate (TEGDMA) concentrations have been found to have superior caries-infiltrating ability and show better caries-inhibition relative to those with high bisphenol A-glycidyl methacrylate (BisGMA) [6]. Alcohol addition is also an effective way to reduce resin viscosity, however, it has been shown to promote the formation of microgels at the sites of polymerization initiation, which reduces the mobility of the generated free radicals, decreasing polymerization [7][8]. Decreased polymerization reduces the mechanical properties of the RIs and limits their ability to inhibit further demineralization of the carious lesion [9], therefore solvent addition to RI is not recommended.
Meta-analysis assessing the effectiveness of resin infiltration in arresting the progress of non-cavitated proximal lesions have found them to be highly efficacious in permanent teeth when the lesions extend into the enamel and outer third of dentin [10][11][12][13][14][15]. For permanent teeth, the risk of caries progression was shown to be significantly lower in infiltrated lesions (4–14%) relative to control (42–48%) over three years [16][17] and Paris et al. found the seven-year rate of progression to be 9% for infiltrated lesions vs 45% for control lesions [18]. Sub-group analysis of RI efficacy in arresting lesions of varying depths showed that while RI was successful in arresting enamel lesions, for dentinal lesions the caries progression rate was not significantly different from control group [13]. The differential treatment efficacy was attributed to differences in the histology and pathology of enamel and dentin caries and is discussed further in a later section.
For primary teeth, early meta-analysis found the data regarding RI efficacy inconclusive, due to the heterogeneity of study designs and settings [10][11][12]. A meta-analysis by Chen et al. in 2021 concluded that although more clinical studies were needed, findings from current studies were encouraging and resin infiltration is efficacious in arresting decay progress in primary teeth for 12–24 months [15]. Based on these studies, the therapeutic effect of RI was found to range from 21% [19][20] to 38% [21].
The success of RIs in arresting the progress of non-cavitated proximal carious lesions has instigated further research exploring the possibility of expanding their use in the treatment of cavitated lesions. For the successful treatment of cavitated lesions using resin infiltration, the RI must be able to not only infiltrate the demineralized portion of the lesion, but also fill the cavitated portion of the lesion. Studies analyzing the effectiveness of RIs in deep and micro-cavitated proximal lesions (International Caries Detection and Assessment System (ICDAS) 3,4,5) found that while RIs can adequately infiltrate demineralized porous enamel in all carious lesions regardless of depth, they could not fill the cavitated portions of larger lesions [22]. The inadequate filling of the cavitated lesions was attributed to three mechanisms: First, porous demineralized enamel has strong capillary forces that drives the perfusion of RI into the pores, while large cavities have weak capillary forces and therefore do not induce similar filling. Second, the cleaning procedure prior to light curing may partially remove some RI from the cavitated lesions. Lastly, penetration of the RI into the cavitated lesions may be impeded by the surface tension of the air bubbles trapped within This inadequate filling leads to the formation of a thin and in-homogenous resin layer in deeper lesions (ICDAS 4&5) compared to ICDAS 2&3 lesions. The caries-inhibiting ability of the resin layer is correlated to the thickness of the resin layer and therefore the thin layer is less efficient at inhibiting demineralization in deeper lesions. Moreover, since incomplete filling of the cavities facilitates biofilm accumulation, it further reduces the caries-inhibiting efficacy of RI in deeper lesions [22].
To enhance the caries-arresting effect of resin infiltration in deep cavitated lesions, (1) its ability to fill cavities must be improved without diminishing its infiltrating capabilities [23][24]. One strategy to improve the filling ability of the RI is to modify its mechanical properties with the addition of fillers such that its viscosity and mechanical properties are optimized while its penetration capability is maintained [23][24]. (2) it may be endowed with antimicrobial properties to increase its ability to eliminate the bacteria within the incompletely filled cavitated lesions and prevent bacterial re-infection.
2. Micro-Filled Infiltrant Resins (MFIR)
RIs have poor mechanical properties such as low mechanical strength, high polymerization shrinkage and low wear resistance. Due to their low viscosity, they have inadequate filling abilities.
To address these issues, micro-filled infiltrant resins (MFIRs) were developed by adding fillers (glass and organic) to RIs since the addition of fillers has been shown to improve the resin mechanical properties such as flexure strength and modulus of elasticity. Filler also reduces polymerization shrinkage and water sorption [25][26]. Ideally, MFIRs should have the infiltrating properties similar to RIs and filling properties comparable to flowable composites.
2.1. Effect of Fillers on RI Properties
When fillers are added to resins, the properties of the resultant resin are influenced by several factors such as the filler shape, size, concentration and interactions between filler particles and resin matrix [27]. When the filler content is low, the inter-particle interaction is weak and as the number of particles increases, they become closely packed and exert stronger inter-particle interactions, increasing resin viscosity [27]. Regarding particle size alone, the addition of very small sized filler particles increases the viscosity of the material more compared to the addition of large filler particles due to the increased surface area and interaction between the filler particle and matrix. The incorporation of larger filler particles, on the other hand, results in the formation of in-homogenous resins with impaired enamel wetting ability, resulting in compromised penetrating properties [24][28].
2.2. Factors Affecting the Movement of RI from Micro-Filled Infiltrant Resin (MFIR)
When the MFIR is applied to a carious lesion, there are two competing phenomena affecting the flow of the infiltrant resin: capillary forces drive the RI from the MFIR to the pores in the demineralized lesion, while the interfacial interaction between the filler particles and the RI in the MFIR restricts the RI’s movement. As the interfacial surface area increases, conversely related to the size of the filler, the amount of RI needed to coat the filler particles increases, reducing the amount of free resin available to infiltrate the carious lesion [23][24][28].
Studies evaluating the effectiveness of MFIR modified with pre-polymerized methacrylate-based fillers (42 μm) in deeper lesions (ICDAS 3&5) found no significant difference in the penetration ability of RI and MFIR. Additionally, the filling ability of MFIR was higher (100% for both groups) than RI (25% for ICDAS 3 and 38% for ICDAS 5). MFIRs had infiltrating properties comparable to RI and filling properties comparable to the flowable composite. This was observed because when MFIR is applied to a carious lesion, the resin infiltrates the carious lesion while the filler is left embedded in the remaining surface monomer, which acts in the same way as flowable resin and fills the cavities [23][24]. These findings suggest that MFIRs may present a promising approach to inhibit caries progression in deep and cavitated proximal lesions.
2.3. RIs for Arresting Occlusal Carious Lesions
In expanding the scope of their use, RIs’ application to arrest occlusal carious lesions has also been investigated. However, due to the poor mechanical properties the use of RIs alone is not recommended for the arrest of occlusal carious lesions [24][29][30]. In vitro studies have advocated the use of micro-filled infiltrant resins (MFIR) or RIs in combination with conventional sealants/flowable composites applied overtop of the infiltrated tooth structure for this purpose [24][30]. These studies have demonstrated that the use of MFIR or RIs with conventional sealants/flowable composites for the arrest of occlusal carious lesions offer several advantages over conventional sealants: First, the diffusion barrier is shifted from the enamel surface to the body of the carious lesion and therefore even if the sealant is lost or does not remain completely intact, the infiltration of the body of the lesion will remain and therefore could prevent the progression of the carious lesion. Second, the ability of RIs to penetrate into carious fissures is superior to that of conventional sealants due to higher penetration coefficients and more intense surface erosion with 15% hydrochloric acid for RIs which facilitates deeper infiltration [24][31]. (Although HCl effectively removes the surface layer of the carious lesion, it must be used cautiously in the oral environment since it may cause accidental injuries to the soft tissue). Third, use of RIs with flowable composites has been shown to reduce immediate microleakage more effectively compared to conventional sealants [32]. Thus, the use of RIs in combination with sealants can mitigate some of the challenges of conventional sealing in carious occlusal fissures including retention, poor penetration and microleakage. Hence, this may be an effective minimally invasive approach to treat carious fissures. The addition of antimicrobial agents to RIs can aid in eliminating the bacteria trapped within the deeper portions of the lesions and could further enhance the caries-arresting efficacy of this treatment modality.
Clinical trials evaluating the effectiveness of RIs in arresting occlusal carious lesions have found that sealing and infiltrating occlusal lesions in combination with fluoride varnish application was highly efficacious in arresting carious lesions relative to varnish application alone in primary dentition over a 2–3 year period [33]. Anauate-Netto et. al., demonstrated that the caries arresting efficacy of both infiltrating and sealing non-cavitated occlusal lesions was comparable over a 3 year period in permanent dentition [34]. In contrast to these findings, Elkwatehy et al. found that in sound and non-cavitated permanent molars, sealing alone and a combination of infiltrating and sealing occlusal lesions was more effective in preventing and arresting the progress of carious lesions whereas the use of RI alone was not effective [35]. The differences in these studies could be attributed to variations in the depth of selected lesions. While the former study included deeper lesions (most ICDAS 2), the latter selected teeth with ICDAS 0,1,2 lesions. It has been shown that sound fissures (ICDAS 0) and incipient lesions (ICDAS 1) may not benefit from infiltration compared to conventional sealants whereas deeper lesions (ICDAS 2) demonstrate higher penetration of RI and consequently superior caries-inhibiting effect compared to sealants alone.
3. Atraumatic Restorative Treatment (ART)
Atraumatic Restorative Treatment (ART) was developed as a treatment approach for restoring caries in developing countries where rendering definitive treatment may be difficult due to lack of resources [36]. It involves the removal of infected tooth structure with hand instruments without the use of anesthesia followed by the filling of the cavity with a fluoride-releasing restorative material such as glass ionomer cement (GIC) or resin modified glass ionomer (RMGI) [37]. The fluoride release from the GIC induces the formation of fluorapatite which is more acid-resistant, making the tooth less susceptible to future caries [38][39]. GIC can be recharged and acts as a reservoir of fluoride ions taken up from topical applications [40][41]. More recently, the use of SDF with ART has been propagated [42]. The most common problems associated with ART are marginal gaps, lack of wear resistance and loss of restorations [43][44].
Meta-analysis assessing the survival rates of ART have found that for primary posterior teeth, they were 94.3% (±1.5) for single surface restorations and 65.4% (±3.9) for multi-surface restorations over 2 years. For permanent posterior teeth, the survival rates were 87.1% (±3.2) for single surface and 77% (±9.0) for multi-surface restorations over 3 and 5 years respectively [45].
ART has been used in the treatment of Early Childhood Caries (ECC) since it does not require administration of GA and prompt, early intervention is key in the treatment of ECC. Silva et al. found the 4-year success rate of ART in children (18–36 months) to be 94 %, 87.5% and 82.9% in 1,2- and 4-year follow-up period. Faccin et al. also assessed ART success amongst preschool children (average age 31 months) and found lower yet acceptable rate of 72% over 25–48 months [46]. These findings show that ART is an effective treatment modality for ECC and yields excellent clinical outcomes.
Attempts have been made to improve the efficacy of ART with the addition of antimicrobial agents. To reduce the number of residual bacteria remaining in the cavity after the removal of infected tissue, CHX was added to GIC. An in vitro study found that incorporating CHX in GIC significantly lowered the residual populations of S. mutans and Lactobacillus in the cavity over 3 months [47]. In vivo studies showed that while the addition of CHX significantly improved the antibacterial properties of GIC, it increased failures due to marginal defects after 9 months [48]. Further research into improving the antimicrobial properties of ART restorations without negatively impacting their mechanical properties is warranted.
References
- Anand, V.; Arumugam, S.B.; Manoharan, V.; Kumar, S.A.; Methippara, J.J. Is Resin Infiltration a Microinvasive Approach to White Lesions of Calcified Tooth Structures?: A Systemic Review. Int. J. Clin. Pediatr. Dent. 2019, 12, 53–58.
- Paris, S.; Meyer-Lueckel, H.; Cölfen, H.; Kielbassa, A.M. Resin Infiltration of Artificial Enamel Caries Lesions with Experimental Light Curing Resins. Dent. Mater. J. 2007, 26, 582–588.
- Kielbassa, A.M.; Muller, J.; Gernhardt, C.R. Closing the gap between oral hygiene and minimally invasive dentistry: A review on the resin infiltration technique of incipient (proximal) enamel lesions. Quintessence Int. 2009, 40, 663–681.
- Kielbassa, A.; Ulrich, I.; Treven, L.; Mueller, J. An updated review on the resin infiltration technique on incipient proximal enamel lesions. Med. Evol. 2010, 16, 3–15.
- Enan, E.T.; Aref, N.S.; Hammad, S.M. Resistance of resin-infiltrated enamel to surface changes in response to acidic challenge. J. Esthet. Restor. Dent. 2019, 31, 353–358.
- Paris, S.; Meyer-Lueckel, H.; Cölfen, H.; Kielbassa, A.M. Penetration coefficients of commercially available and experimental composites intended to infiltrate enamel carious lesions. Dent. Mater. 2007, 23, 742–748.
- Ye, Q.; Spencer, P.; Wang, Y.; Misra, A. Relationship of solvent to the photopolymerization process, properties, and structure in model dentin adhesives. J. Biomed. Mater. Res. Part A 2007, 80, 342–350.
- Araújo, G.S.A.; Sfalcin, R.A.; Araújo, T.G.F.; Alonso, R.C.B.; Puppin-Rontani, R.M. Evaluation of polymerization characteristics and penetration into enamel caries lesions of experimental infiltrants. J. Dent. 2013, 41, 1014–1019.
- Meyer-Lueckel, H.; Paris, S. Infiltration of Natural Caries Lesions with Experimental Resins Differing in Penetration Coefficients and Ethanol Addition. Caries Res. 2010, 44, 408–414.
- Ammari, M.M.; Soviero, V.M.; Fidalgo, T.; Lenzi, M.; Ferreira, D.M.T.; Mattos, C.T.; Souza, I.P.; Maia, L.C. Is non-cavitated proximal lesion sealing an effective method for caries control in primary and permanent teeth? A systematic review and meta-analysis. J. Dent. 2014, 42, 1217–1227.
- Dorri, M.; Dunne, S.M.; Walsh, T.; Schwendicke, F. Micro-invasive interventions for managing proximal dental decay in primary and permanent teeth. Cochrane Database Syst. Rev. 2015, 2015, CD010431.
- Chatzimarkou, S.; Koletsi, D.; Kavvadia, K. The effect of resin infiltration on proximal caries lesions in primary and permanent teeth. A systematic review and meta-analysis of clinical trials. J. Dent. 2018, 77, 8–17.
- Liang, Y.; Deng, Z.; Dai, X.; Tian, J.; Zhao, W. Micro-invasive interventions for managing non-cavitated proximal caries of different depths: A systematic review and meta-analysis. Clin. Oral Investig. 2018, 22, 2675–2684.
- Elrashid, A.H.; Alshaiji, B.S.; Saleh, S.A.; Zada, K.A.; Baseer, M.A. Efficacy of Resin Infiltrate in Noncavitated Proximal Carious Lesions: A Systematic Review and Meta-Analysis. J. Int. Soc. Prev. Community Dent. 2019, 9, 211–218.
- Chen, Y.; Chen, D.; Lin, H. Infiltration and sealing for managing non-cavitated proximal lesions: A systematic review and meta-analysis. BMC Oral Health 2021, 21, 13.
- Peters, M.; Hopkins, A.; Zhu, L.; Yu, Q. Efficacy of Proximal Resin Infiltration on Caries Inhibition: Results from a 3-Year Randomized Controlled Clinical Trial. J. Dent. Res. 2019, 98, 1497–1502.
- Meyer-Lueckel, H.; Bitter, K.; Paris, S. Randomized Controlled Clinical Trial on Proximal Caries Infiltration: Three-Year Follow-Up. Caries Res. 2012, 46, 544–548.
- Paris, S.; Bitter, K.; Krois, J.; Meyer-Lueckel, H. Seven-year-efficacy of proximal caries infiltration—Randomized clinical trial. J. Dent. 2020, 93, 103277.
- Page, L.F.; Beckett, D.; Ahmadi, R.; Schwass, D.; De La Barra, S.L.; Moffat, S.; Meldrum, A.; Thomson, W. Resin Infiltration of Caries in Primary Molars in a Community Setting: 24-Month Randomized Controlled Trial Findings. JDR Clin. Transl. Res. 2017, 2, 287–294.
- Ammari, M.M.; Jorge, R.C.; Souza, I.P.; Soviero, V.M. Efficacy of resin infiltration of proximal caries in primary molars: 1-year follow-up of a split-mouth randomized controlled clinical trial. Clin. Oral Investig. 2017, 22, 1355–1362.
- Ekstrand, K.; Bakhshandeh, A.; Martignon, S. Treatment of Proximal Superficial Caries Lesions on Primary Molar Teeth with Resin Infiltration and Fluoride Varnish versus Fluoride Varnish Only: Efficacy after 1 Year. Caries Res. 2010, 44, 41–46.
- Paris, S.; Bitter, K.; Naumann, M.; Dörfer, C.E.; Meyer-Lueckel, H. Resin infiltration of proximal caries lesions differing in ICDAS codes. Eur. J. Oral Sci. 2011, 119, 182–186.
- Askar, H.; Schwendicke, F.; Lausch, J.; Meyer-Lueckel, H.; Paris, S. Modified resin infiltration of non-, micro- and cavitated proximal caries lesions in vitro. J. Dent. 2018, 74, 56–60.
- Askar, H.; Lausch, J.; Dörfer, C.E.; Meyer-Lueckel, H.; Paris, S. Penetration of micro-filled infiltrant resins into artificial caries lesions. J. Dent. 2015, 43, 832–838.
- Bourbia, M.; Finer, Y. Biochemical Stability and Interactions of Dental Resin Composites and Adhesives with Host and Bacteria in the Oral Cavity: A Review. J. Can. Dent. Assoc. 2018, 84, i1.
- Klapdohr, S.; Moszner, N. New Inorganic Components for Dental Filling Composites. Mon. Chem.-Chem. Mon. 2004, 136, 21–45.
- Lee, J.-H.; Um, C.-M.; Lee, I.-B. Rheological properties of resin composites according to variations in monomer and filler composition. Dent. Mater. 2006, 22, 515–526.
- Beun, S.; Bailly, C.; Dabin, A.; Vreven, J.; Devaux, J.; Leloup, G. Rheological properties of experimental Bis-GMA/TEGDMA flowable resin composites with various macrofiller/microfiller ratio. Dent. Mater. 2009, 25, 198–205.
- Zhao, X.; Pan, J.; Zhang, S.; Malmstrom, H.S.; Ren, Y.-F. Effectiveness of resin-based materials against erosive and abrasive enamel wear. Clin. Oral Investig. 2017, 21, 463–468.
- Lausch, J.; Askar, H.; Paris, S.; Meyer-Lueckel, H. Micro-filled resin infiltration of fissure caries lesions in vitro. J. Dent. 2017, 57, 73–76.
- Paris, S.; Lausch, J.; Selje, T.; Dörfer, C.; Meyer-Lueckel, H. Comparison of sealant and infiltrant penetration into pit and fissure caries lesions in vitro. J. Dent. 2014, 42, 432–438.
- Da Silva, V.B.; De Carvalho, R.N.; Bergstrom, T.G.; Dos Santos, T.M.P.; Lopes, R.T.; Neves, A.D.A. Sealing Carious Fissures with Resin Infiltrant in Association with a Flowable Composite Reduces Immediate Microleakage? Pesqui. Bras. Odontopediatria Clín. Integr. 2020, 20, e5114.
- Bakhshandeh, A.; Ekstrand, K. Infiltration and sealing versus fluoride treatment of occlusal caries lesions in primary molar teeth. 2-3 years results. Int. J. Paediatr. Dent. 2014, 25, 43–50.
- Anauate-Netto, C.; Neto, L.B.; Amore, R.; Di Hipólito, V.; Alpino, P.H.P.D. Caries progression in non-cavitated fissures after infiltrant application: A 3-year follow-up of a randomized controlled clinical trial. J. Appl. Oral Sci. 2017, 25, 442–454.
- Elkwatehy, W.M.A.; Bukhari, O.M. The efficacy of different sealant modalities for prevention of pits and fissures caries: A randomized clinical trial. J. Int. Soc. Prev. Community Dent. 2019, 9, 119–128.
- Smales, R.J.; Yip, H.K. The atraumatic restorative treatment (ART) approach for primary teeth: Review of literature. Pediatr. Dent. 2000, 22, 294–298.
- Holmgren, C.J.; Roux, D.; Doméjean, S. Minimal intervention dentistry: Part 5. Atraumatic restorative treatment (ART)—A minimum intervention and minimally invasive approach for the management of dental caries. Br. Dent. J. 2013, 214, 11–18.
- Tyas, M. Cariostatic effect of glass ionomer cement: A five-year clinical study. Aust. Dent. J. 1991, 36, 236–239.
- Tam, L.E.; Chan, G.P.; Yim, D. In vitro caries inhibition effects by conventional and resin-modified glass-ionomer restorations. Oper. Dent. 1997, 22, 4–14.
- Forsten, L. Fluoride release and uptake by glass-ionomers and related materials and its clinical effect. Biomaterials 1998, 19, 503–508.
- Donly, K.J.; Nelson, J.J. Fluoride release of restorative materials exposed to a fluoridated dentifrice. ASDC J. Dent. Child. 1997, 64, 249–250.
- Crystal, Y.O.; Marghalani, A.A.; Ureles, S.D.; Wright, J.T.; Sulyanto, R.; Divaris, K.; Fontana, M.; Graham, L. Use of Silver Diamine Luoride for Dental Caries Management in Children and Adolescents, Including Those with Special Health Care Needs. Pediatr. Dent. 2017, 39, 135–145.
- Kemoli, A.M.; Van Amerongen, W.E. Effects of oral hygiene, residual caries and cervical Marginal-gaps on the survival of proximal atraumatic restorative treatment approach restorations. Contemp. Clin. Dent. 2011, 2, 318–323.
- Da Franca, C.; Colares, V.; Van Amerongen, E. Two-year evaluation of the atraumatic restorative treatment approach in primary molars class I and II restorations. Int. J. Paediatr. Dent. 2011, 21, 249–253.
- De Amorim, R.G.; Frencken, J.E.; Raggio, D.P.; Chen, X.; Hu, X.; Leal, S.C. Survival percentages of atraumatic restorative treatment (ART) restorations and sealants in posterior teeth: An updated systematic review and meta-analysis. Clin. Oral Investig. 2018, 22, 2703–2725.
- Faccin, E.S.; Ferreira, S.H.; Kramer, P.F.; Ardenghi, T.; Feldens, C.A. Clinical Performance of Art Restorations in Primary Teeth: A Survival Analysis. J. Clin. Pediatr. Dent. 2009, 33, 295–298.
- Joshi, J.S.; Roshan, N.M.; Sakeenabi, B.; Poornima, P.; Nagaveni, N.B.; Subbareddy, V.V. Inhibition of Residual Cariogenic Bacteria in Atraumatic Restorative Treatment by Chlorhexidine: Disinfection or Incorporation. Pediatr. Dent. 2017, 39, 308–312.
- Kabil, N.S.; Badran, A.; Wassel, M.O. Effect of the addition of chlorhexidine and miswak extract on the clinical performance and antibacterial properties of conventional glass ionomer: An in vivo study. Int. J. Paediatr. Dent. 2016, 27, 380–387.
More
Information
Subjects:
Dentistry, Oral Surgery & Medicine
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.5K
Revisions:
3 times
(View History)
Update Date:
11 Jan 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




