Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Marina Perez-Gordo | + 3275 word(s) | 3275 | 2021-11-09 03:48:52 | | | |
| 2 | Vivi Li | Meta information modification | 3275 | 2021-12-27 03:32:53 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Perez-Gordo, M. Non-IgE-Mediated Gastrointestinal Food Protein-Induced Allergic Disorders. Encyclopedia. Available online: https://encyclopedia.pub/entry/17562 (accessed on 07 February 2026).
Perez-Gordo M. Non-IgE-Mediated Gastrointestinal Food Protein-Induced Allergic Disorders. Encyclopedia. Available at: https://encyclopedia.pub/entry/17562. Accessed February 07, 2026.
Perez-Gordo, Marina. "Non-IgE-Mediated Gastrointestinal Food Protein-Induced Allergic Disorders" Encyclopedia, https://encyclopedia.pub/entry/17562 (accessed February 07, 2026).
Perez-Gordo, M. (2021, December 26). Non-IgE-Mediated Gastrointestinal Food Protein-Induced Allergic Disorders. In Encyclopedia. https://encyclopedia.pub/entry/17562
Perez-Gordo, Marina. "Non-IgE-Mediated Gastrointestinal Food Protein-Induced Allergic Disorders." Encyclopedia. Web. 26 December, 2021.
Copy Citation
Non-IgE-mediated gastrointestinal food allergy (non-IgE-GI-FA) is the name given to a series of pathologies whose main entities are food protein-induced allergic proctocolitis (FPIAP), food protein-induced enteropathy (FPE), and food protein-induced enterocolitis syndrome (FPIES). These are more uncommon than IgE-mediated food allergies, their mechanisms remain largely unknown, and their diagnosis is mainly done by clinical history, due to the lack of specific biomarkers.
food allergy
non-IgE-mediated gastrointestinal food allergy
Cow’s milk
Food protein-induced enterocolitis syndrome
Food protein-induced allergic proctocolitis
Food protein-induced enteropathy
Fecal calprotectin
omics
1. Digestive Manifestations of Food Allergy
Food allergy (FA) is a specific immunological response that occurs reproducibly on exposure to a given food. This immune reaction can be due to an IgE-mediated mechanism or a non-IgE-mediated mechanism. IgE-mediated FA is much more common than non-IgE-mediated FA, the symptoms are easily recognized, and the underlying mechanisms are better established [1].
Although the relationship between food allergy and gastrointestinal dysfunction has been known for several years, the exact mechanisms involved have not yet been clearly defined. The diagnosis of non-IgE-mediated gastrointestinal food allergy (non-IgE-GI-FA) is clinical and—due to a lack of a specific biomarker—not always easy. The diagnosis is based on compatible symptoms, the exclusion of other diseases, resolution of the symptoms once the offending food is removed from the diet, and the reappearance of the symptoms when it is reintroduced.
Non-IgE-mediated gastrointestinal food allergy typically comprises three entities: (i) food protein-induced allergic proctocolitis (FPIAP); (ii) food protein-induced enteropathy (FPE), and (iii) food protein-induced enterocolitis syndrome (FPIES).
1.1. Food Protein-Induced Allergic Proctocolitis (FPIAP)
Food protein-induced allergic proctocolitis (FPIAP) is a non-IgE-mediated food allergy characterized by bloody stools in a healthy infant. The symptoms begin within the first months of life; usually in the first two months. It affects both exclusively breastfed infants and formula-fed infants; although it appears to be slightly more common in exclusively breastfed infants (60%) [2].
The most common offending triggers are cow’s milk (CM) proteins (76%), followed by hen’s egg (16%), soy (6%), and corn (2%). In 8% of the cases, the etiology could be multiple [3]. Any food can induce FPIAP and, once the food is removed from the diet, symptoms disappear within a fortnight. Therefore, if the symptoms persist, it is necessary to continue withdrawing food or looking for another diagnosis [4].
The pathophysiological mechanism of FPIAP is not well established. It seems that it involves CD8+ lymphocytes, Th-2 type lymphocytes, and eosinophil infiltrate in all layers of the colonic mucosa [5]. Additionally, some studies suggest the involvement of T-cells in the pathogenesis of this entity, associated with secretion of tumor necrosis factor-alpha (TNF-α) by activated lymphocytes [6].
The typical clinical manifestations are mucus bloody stools in a healthy appearing infant. The bleeding is usually visible although it can appear as occult blood in the stools. Some patients have iron-deficiency anaemia and less frequent hypoalbuminemia and peripheral eosinophilia [7]. Symptoms such as vomiting, frank diarrhoea, or unwell appearance are not present, unlike FPE and FPIES.
FPIAP is a very common cause of rectal bleeding in infants although the real prevalence is unknown. The population prevalence in infants is approximately 1% to 2%. The prevalence among infants with rectal bleeding ranges from 18% to 64% [8]. Elizur et al. found an accumulative incidence in 13,019 newborns over a two-year period of 0.16% [9]. Other studies have reported that FPIAP represents between 18% and 64% of children with rectal bleeding when the diagnosis is based on withdrawal of the offending food or by biopsy findings from the flexible sigmoidoscopy [10][11].
The diagnosis is clinical and based on the following criteria: (a) small amount of rectal bleeding in an otherwise healthy infant; (b) disappearance of symptoms after all causal food is removed from diet; and (c) exclusion of other causes of rectal bleeding [12]. Although the histopathological findings are not pathognomonic of the disease, Odze et al. suggest that the finding of ≥60 eosinophils/10 high-power fields is enough to establish the diagnosis in 97.4% of the cases [13].
The differential diagnosis includes anal fissure, which is the most common cause of rectal bleeding in children under 12 months; swallowed maternal blood, or other diseases, such as enteric infection, malrotation with volvulus or Hirschsprung disease—but these usually affect the general condition [8].
FPIAP can be an over-diagnosed entity, which is why some authors advocate the performance of an early oral food challenge (OFC) to avoid unnecessary elimination diets [14].
The prognosis is excellent and nearly all infants outgrow the disease by 1 to 3 years of age [15].
1.2. Food Protein-Induced Enteropathy (FPE)
Food protein-induced enteropathy (FPE) is also a non-IgE-GI-FA. It is probably the most forgotten disorder of the three, and in recent years there are hardly reports of FPE in the literature. The symptoms begin in the first year of life and manifest as chronic diarrhea and intermittent vomiting. If the symptoms persist, they will lead to poor weight gain, failure to thrive, and villous atrophy. Some children develop an iron-deficiency anemia associated with the presence of occult blood in the stools [16]. The pathophysiologic mechanisms are unknown, as is the real prevalence.
The most common offending triggers are CM proteins and soy. The diagnosis is based on a compatible clinical history, the anatomopathological findings, and the disappearance of the symptoms once the food is removed from the diet. Intestinal lesions are patchy with villus atrophy, crypt hyperplasia, increased number of intraepithelial lymphocytes, and eosinophilic infiltration [12].
The main differential diagnosis is with celiac disease. Clinically and pathologically, they are indistinguishable, but the typical celiac disease antibodies are absent in FPE [17].
1.3. Food Protein-Induced Enterocolitis Syndrome (FPIES)
FPIES has been considered a rare disease, whose cumulative incidence rates are between 0.15–0.7% [18]. However, it might be under-diagnosed since the epidemiological data are scarce and variable.
FPIES is a non-IgE-GI-FA and is considered a heterogenous disorder with a wide spectrum of clinical phenotypes. These are based on: (i) time and duration of the symptoms, (ii) age of presentation, and (iii) specific IgE-positive of the causal food. Thus, we can classify FPIES into acute, chronic, later onset, and atypical [19].
Acute FPIES usually presents in infancy, with repetitive protracted vomiting that begins 1 to 4 h after food ingestion. Vomiting is often accompanied by lethargy and pallor and can be followed by diarrhea. Some patients have an isolated fever peak and severe cases can progress to hypothermia, methemoglobinemia, acidemia, and hypotension, mimicking sepsis [20]. Children are well between episodes and have normal growth, and these typical symptoms commonly disappear within 24 h.
Chronic FPIES is less well characterized. In this presentation, the symptoms occur over several days or weeks and do not have a clear relationship with the offending food. Children have intermittent vomiting and/or diarrhea, failure to thrive, or poor weight gain. The severe form can develop dehydration and hypovolemic shock. In chronic FPIES, once the offending food is removed from the diet, the symptoms subside within two weeks, but re-exposure to it triggers the typical symptoms of acute FPIES. When the disease onsets in adolescence or adulthood, the symptoms appear after years of tolerance to the food and the predominant symptoms are, in most cases, colic abdominal pain and diarrhea [19][20][21][22].
Although FPIES is considered a non-IgE-mediated FA, in some patients, it is possible to detect specific IgE against the causal food, either at the beginning or during the course of the disease. This form of presentation is known as atypical FPIES and it seems to have a protracted course, with a further risk of developing IgE-mediated symptoms. In adults, it has been also described that severe FPIES phenotypes developed IgE and this is linked to the worst prognosis of the disease [19][21][23][24][25][26].
Any food can trigger FPIES; however, there are geographical differences, and some foods are more prevalent than others. In the USA, the most causative foods are CM proteins and soy. Children with either CM- or soy-induced FPIES can also react to both foods and have an increased likelihood of reacting to a solid food, most commonly oats and rice. In Asia, CM, soy-based formulas, and rice are the most common causal foods. Soy is especially frequent in Korea, but it has a better prognosis and earlier resolution than in other countries. Rice has been observed to be the main trigger of FPIES among the Australian pediatric population, and in European countries, CM and fish are the most frequent triggers of FPIES [27][28][29].
The development of tolerance varies by type of trigger and geographic location. CM- and soy-induced FPIES are reported to occur at an earlier age than other foods. The average age of tolerance of grains-FPIES is 35 months and fish-FPIES usually resolves within the first 5 years [27][28].
Nowadays, there is not a specific biomarker for FPIES that allows for confirmation of the diagnosis or to predict when the tolerance to the offending food has been achieved. For this reason, all patients with FPIES should undergo an oral food challenge (OFC) at least once in life. The OFC is a risky procedure and patients can develop moderate or severe symptoms after it, so it should be always performed under medical supervision [20][30].
The diagram shown in Figure 1 summarizes similarities and differences of FPIAP, FPE, and FPIES.
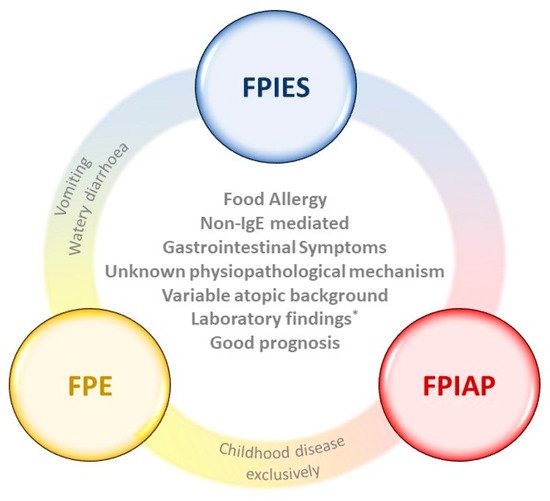
Figure 1. Description of differences and similarities between FPIES, FPE, and FPIAP. FPIES: food protein-induced enterocolitis syndrome; FPE: food protein-induced enteropathy; FPIAP: food protein-induced allergic proctocolitis. * Laboratory findings (e.g., anemia, iron deficiency, eosinophilia, rectal bleeding, etc.) are similar as long as the food is not withdrawn from the diet.
2. Approaches for the Study of Non-IgE-GI-FA
The most important diagnostic tool in the evaluation of non-IgE-GI-FA is a careful clinical history. However, when the clinical history is not sufficiently thorough, the OFC should be used as the gold standard to confirm the diagnosis of this disease, as has been mentioned above [21][31][32].
There are no other specific diagnostic procedures for these diseases, mainly because their pathophysiological mechanisms are poorly understood. However, there are a variety of laboratory tests to support the diagnosis and, more importantly, to rule out other conditions such as lactose intolerance, sepsis, necrotizing enterocolitis, anaphylaxis, gastrointestinal reflux disease, and celiac disease, among others [20]. In this sense, animal models are also playing an important role in the understanding of the pathophysiological mechanisms involved in these pathologies.
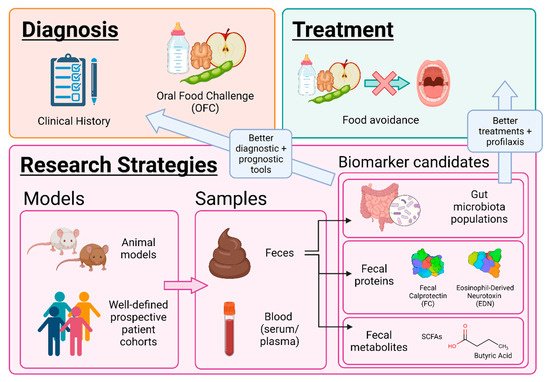
For the in-depth study of non-IgE-GI-FA, feces are the sample of choice. This is due to the fact that the main system affected is the gastrointestinal tract and to their non-invasive collection [33]. There are fecal biomarkers, such as immune cell derived proteins and/or gut microbiota metabolites, defined as biological entities capable of predicting an individual’s physiological state or pathological condition. The detection of these biomarkers by analytical techniques is on the rise to learn more about the underlying mechanisms of these pathologies [16][34]. In this review, different emerging approaches, such as animal models, omics techniques, and identification of fecal biomarkers are described to deepen the understanding of non-IgE-GI-FA (Figure 2).
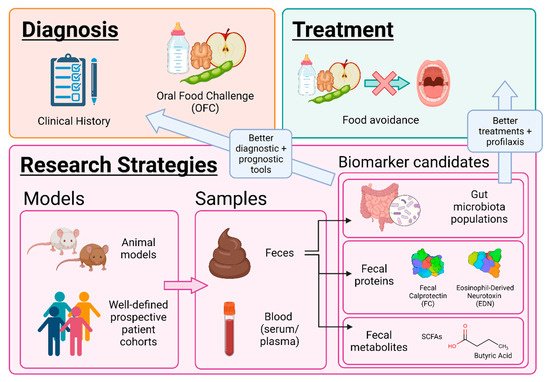
Figure 2. Approaches for the study of non-IgE-mediated gastrointestinal food allergy. SCFAs: short-chain fatty acids.
2.1. Animal Models
Animal models are a useful tool to study allergic diseases in vivo. Several mouse models have been developed to study the gastrointestinal reactions related to food allergy [35][36][37][38][39][40][41][42][43]. Unfortunately, while several IgE-mediated food allergy models have been developed [35][41][42][43][44][45], the generation of non-IgE-mediated murine models has been harder to accomplish. For example, to our knowledge, no animal models have been successfully developed for FPIES, FPIAP, and FPE. However, Burggraf et al. generated a mouse model with intestinal symptoms of a food allergy which resemble these pathologies to study their pathomechanism. This model is known as allergic enteritis (AE), and it mimics in mice some traits observed in patients with non-IgE-GI-FA, such as intestinal inflammation characterized by thicker basal layer, crypt elongation, villous atrophy, and granulocyte infiltration [37]. The initial stimulus leading to the development of allergic enteritis remains to be elucidated, but it is postulated that delayed Th2 cell mediated responses are involved in the development of the inflammation [21][23][24][25][26]. In this model, mice are intraperitoneally sensitized with ovalbumin (OVA) and alum as adjuvant and then challenged with a diet containing high amounts of egg white (EW-diet) [37]. After 4 weeks, tolerance is achieved, but chronic inflammation is still present, despite the lack of allergic signs and the OVA-specific IgE reduction [37]. In a recent study, this AE murine model was used to elucidate the molecular and cellular mechanisms underlying AE [46]. A CC chemokine receptor 8 (CCR8) knock-out mouse was used. CCR8 deficiency translated in a reduced inflammatory profile, characterized by a reduction in the number of infiltrating eosinophils and an enhanced number of neutrophils in the lamina propria of the CCR8KO mice [46]. This revealed that the chemokine CCL1 and its receptor CCR8 are essential for the recruitment of eosinophils in AE sites [46].
2.2. Gut Microbiota and Omics Techniques
The human microbiota and its genetic composition—known as the human microbiome—began to be studied on a large scale at the beginning of the 21st century within the framework of major projects such as the Human Microbiome Project [47]. Among the microbial ecosystems of the human body, the gut microbiota, present in the gastrointestinal tract, is considered a highly important “superorganism” due to its diversity and complexity [48][49].
Approximately 70% of the primary colonization of the gut microbiota of newborns is vertically transmitted, occurring directly from mother to offspring. However, the composition of the gut microbiota is dynamic and changes throughout life due to factors such as delivery mode, age, diet, antibiotic consumption, ethnicity, lifestyle, environmental factors, and diseases and disorders, among others [33][50][51][52].
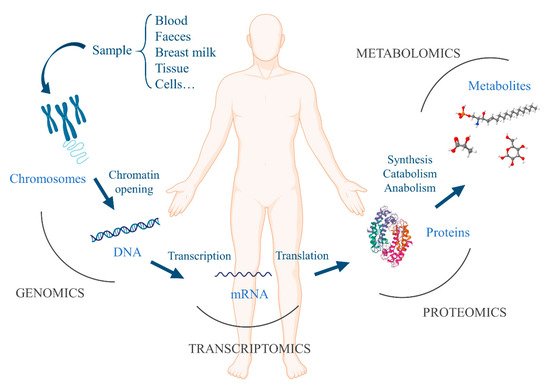
The development of the gut microbiota during the first years of life correlates with the development and maturation of the immune system. Moreover, the gut microbiota and the production of gut microbiota-derived short-chain fatty acids (SCFAs: acetic, propionic, and butyric acids) have been shown to be crucial for the proper expression and function of regulatory T cells (Treg), which are important in the induction and maintenance of oral tolerance to food antigens in humans [53][54][55][56][57][58][59][60]. Trompette et al. described in 2014 how high-fiber diet intake in mice offered protection against allergic inflammation in the lungs due to an increased level of circulating SCFAs compared to normal diet-fed mice [61]. Bunyavanich et al. studied the association between CM allergy resolution and early-life gut microbiota, showing an association between gut microbiome at early stages of life (from 3 to six months of age) and milk allergy resolution by age 8 years. This fact was due to the presence of bacterial taxa Clostridia and Firmicutes, suggesting them as potential probiotics candidates for milk allergy treatment [56]. For the analysis and understanding of the gut microbiota, omics are the techniques of election. In the last decades, advances in bioinformatics, as well as the development of high-throughput technologies, have contributed to the development of omics sciences for the study of multifactorial diseases, including allergy [62]. This group of sciences encompasses different disciplines such as genomics (the genome and its function), transcriptomics (mRNA and gene expression), proteomics (structure, function, location, and interaction of proteins), and metabolomics (metabolites and metabolism) (Figure 3) [63].
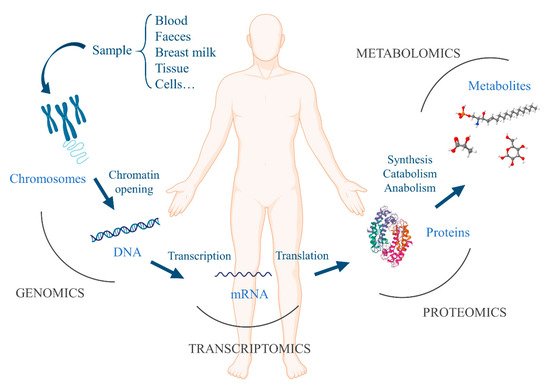
Figure 3. Main omics techniques: genomics, transcriptomics, proteomics, and metabolomics.
The trend in publications of studies analyzing the intestinal microbiota through omics techniques in patients with non-IgE-GI-FA is growing. For this reason, this field is likely to evolve very rapidly in the coming years. Table 1 lists all the studies to date and summarizes what has been found in terms of genomics and metabolomics.
Table 1. Summary of described studies using genomics and metabolomics to study non-IgE-GI-FA.
| Disease | Description | Diet of Allergic Infants | Microbial Communities (Genomics) |
Metabolites (Metabolomics) |
Reference |
|---|---|---|---|---|---|
| Non-IgE-mediated CMA | Allergic vs. healthy children | No dietary restriction (collection at diagnosis) | ↑ Phylum Bacteroidetes ↑ Genera Bacteroides, Alistipes, and Sarcina |
↓ Fecal butyrate | Berni Canani et al. [58] |
| Non-IgE-mediated CMA | Allergic vs. healthy infants (unrestricted conventional diet) | Milk exclusion diet for six months:
|
EHF, SPBF & HRF: ↑ Families Lachnospiraceae and Coriobacteriaceae ↓ Genus Bacteroides HRF: ↓ Genus Bifidobacteria |
↑ Isobutyric and isovaleric acids = Acetic, propionic, and butyric acids | Díaz et al. [64] |
| Non-IgE-mediated CMA | Allergic with test formula vs. allergic with control formula vs. HBI at week 8 | Amino acid-based formula for 8 weeks:
|
Bifidobacteria: HBI > test formula > control formula Eubacterium rectale/Clostridium coccoides: HBI < test formula < control formula |
- | Candy et al. [65] |
| Non-IgE-mediated CMA | Allergic with test formula vs. allergic with control formula at week 26 | Formula for 26 weeks:
|
Bifidobacteria: test formula > control formula Eubacterium rectale/Clostridium coccoides: test formula < control formula |
- | Fox et al. [66] |
| Non-IgE-mediated CMA | Allergic with test formula vs. allergic with control formula vs. HBI | Amino acid-based formula:
|
Test vs. control: ↑ Species of Bifidobacterium and Veillonella families ↓ Species of Lachnospiraceae family and Ruminococcus and Alistipes genera HBI vs. test formula: ≈ Bifidobacterium spp. and Lachnospiraceae spp. |
Test vs. control: ↑ L-lactate ↓ Valeric and isobutyric acids = Acetate, propionate, butyrate, iso-valerate, and D-lactate |
Wopereis et al. [67] |
| Non-IgE-mediated CMA | Allergic children before and after milk challenges | Hypoallergenic hydrolyzed formulas | ↑ Lactic acid bacteria (genus Lactobacillus) ↓ Bacterial groups of Lachnospiraceae and Ruminococcaceae families |
↑ Skatole ↓ p-cresol and BCFAs = Acetic, propionic, and butyric acids |
Guadamuro et al. [68] |
| Gastrointestinal disorders | Colic vs. non-IgE-mediated CMA vs. proctocolitis vs. healthy controls | Exclusive breastfeeding | Fecal microbiota in non-IgE-mediated CMA: ↑ Families Eggerthellaceae, Lachnospiraceae, and Peptostreptococcaceae ↑ Genera Intestinibacter (more increased in proctocolitis) and Rothia↓ Genera Erysipelatoclostridium (higher in controls) and Bifidobacterium Breast milk: ↑ Family Eggerthellaceae in non-IgE-mediated CMA ↑ Family Prolixibacteraceae in proctocolitis |
- | Aparicio et al. [69] |
Footnote. CMA: cow’s milk allergy; EHF: extensively hydrolyzed formula; SPBF: soy protein-based formula; HRF: hydrolyzed rice formula; HBI: healthy breastfed infants; AAF: amino acid-based formula; CMF: cow’s milk formula; BCFAs: branched-chain fatty acids. Arrow ↑ stands for increased levels of microbial communities and/or metabolites. Arrow ↓ stands for decreased levels of microbial communities and/or metabolites.
2.3. Fecal Biomarkers. Protein Analysis
The attempts to evaluate the use of fecal biomarkers for the diagnosis of non-IgE FAs have been reviewed recently [16]. The main candidates are fecal calprotectin (FC), α-1 antitrypsin, β-defensin, tumor necrosis factor-α (TNF-α), fecal IgA, eosinophil-derived neurotoxin (EDN), and eosinophilic cationic protein (ECP). From these, FC has been the most discussed, and it has been the subject of a recent systematic review for its use as a biomarker for CMA, including IgE- and non-IgE-mediated forms [70].
Calprotectin is an immunomodulatory, antimicrobial, and antiproliferative protein that is present in the cytoplasm of neutrophils, in the membranes of macrophages, in activated monocytes, and in mucosal epithelial cells [71]. The measurement of FC has been evaluated as a non-invasive marker of gastrointestinal inflammation, as it is known that its concentrations are correlated with the level of intestinal mucosal inflammation [72]. Based on this fact, it has been used for the monitoring of intestinal conditions such as inflammatory bowel disease (IBD) [16][73] and distinguishing it from irritable bowel syndrome (IBS) [74]. As for its measurement for CMA, a remarkable example is the study by Beşer and collaborators, which analyzed children with CMA (24 IgE-mediated, 8 non-IgE-mediated) and compared them to 39 controls of the same age range, before and after an elimination diet [75]. These authors found that FC levels were highest in children with non-IgE-mediated CMA, from which they suggest its use as a biomarker. However, the evidence is conflicting, since other authors found no significant differences [64][76]. Systematic reviews have concluded that the available evidence is not enough to encourage its use as a biomarker for monitoring CMA, neither IgE- nor non-IgE-mediated [16][70]. Altogether, authors agree that more well-defined studies are needed, and stress the need for establishing the exact cut-off values of FC in different groups taking into account factors such as age, feeding patterns, clinical symptoms, and immune mechanism type [70].
On the other hand, α-1 antitrypsin is an inhibitor of serine proteases present in serum which is synthesized in the liver [77]. It can be measured to assess the excessive GI protein losses in patients with protein-losing enteropathy (PLE) [78][79]. It should be noted that PLE must not be confused with α-1 antitrypsin deficiency, a separate condition, as has sometimes been reported in the literature [79]. In the case of CMA, there is very little data: to the best of our knowledge, only one paper reports its measurement in a study of CMA, alongside a panel of other markers, and did not find significant differences for this protein [80].
References
- Boyce, J.A.; Assa’ad, A.; Burks, A.W.; Jones, S.M.; Sampson, H.A.; Wood, R.A.; Plaut, M.; Cooper, S.F.; Fenton, M.J.; NIAID-Sponsored Expert Panel; et al. Guidelines for the Diagnosis and Management of Food Allergy in the United States: Report of the NIAID-Sponsored Expert Panel. J. Allergy Clin. Immunol. 2010, 126, S1–S58.
- Nowak-Węgrzyn, A. Food Protein-Induced Enterocolitis Syndrome and Allergic Proctocolitis. Allergy Asthma Proc. 2015, 36, 172–184.
- Lake, A.M. Food-Induced Eosinophilic Proctocolitis. J. Pediatr. Gastroenterol. Nutr. 2000, 30, S58–S60.
- Lake, A.M.; Whitington, P.F.; Hamilton, S.R. Dietary Protein-Induced Colitis in Breast-Fed Infants. J. Pediatr. 1982, 101, 906–910.
- Fagundes-Neto, U.; Ganc, A.J. Allergic Proctocolitis: The Clinical Evolution of a Transitory Disease with a Familial Trend. Case Reports. Einstein 2013, 11, 229–233.
- Chung, H.L.; Hwang, J.B.; Park, J.J.; Kim, S.G. Expression of Transforming Growth Factor Beta1, Transforming Growth Factor Type I and II Receptors, and TNF-Alpha in the Mucosa of the Small Intestine in Infants with Food Protein-Induced Enterocolitis Syndrome. J. Allergy Clin. Immunol. 2002, 109, 150–154.
- Sampson, H.A.; Anderson, J.A. Summary and Recommendations: Classification of Gastrointestinal Manifestations Due to Immunologic Reactions to Foods in Infants and Young Children. J. Pediatr. Gastroenterol. Nutr. 2000, 30, S87–S94.
- Liacouras, C.A. Food Protein-Induced Allergic Proctocolitis of Infancy—UpToDate. Available online: https://www.uptodate.com/contents/food-protein-induced-allergic-proctocolitis-of-infancy (accessed on 8 April 2021).
- Elizur, A.; Cohen, M.; Goldberg, M.R.; Rajuan, N.; Cohen, A.; Leshno, M.; Katz, Y. Cow’s Milk Associated Rectal Bleeding: A Population Based Prospective Study. Pediatr. Allergy Immunol. 2012, 23, 766–770.
- Arvola, T.; Ruuska, T.; Keränen, J.; Hyöty, H.; Salminen, S.; Isolauri, E. Rectal Bleeding in Infancy: Clinical, Allergological, and Microbiological Examination. Pediatrics 2006, 117, e760–e768.
- Caubet, J.-C.; Szajewska, H.; Shamir, R.; Nowak-Węgrzyn, A. Non-IgE-Mediated Gastrointestinal Food Allergies in Children. Pediatr. Allergy Immunol. 2017, 28, 6–17.
- Connors, L.; O’Keefe, A.; Rosenfield, L.; Kim, H. Non-IgE-Mediated Food Hypersensitivity. Allergy Asthma Clin. Immunol. 2018, 14, 56.
- Odze, R.D.; Bines, J.; Leichtner, A.M.; Goldman, H.; Antonioli, D.A. Allergic Proctocolitis in Infants: A Prospective Clinicopathologic Biopsy Study. Hum. Pathol. 1993, 24, 668–674.
- Hwang, J.-B.; Hong, J. Food Protein-Induced Proctocolitis: Is This Allergic Disorder a Reality or a Phantom in Neonates? Korean J. Pediatr. 2013, 56, 514–518.
- Xanthakos, S.A.; Schwimmer, J.B.; Melin-Aldana, H.; Rothenberg, M.E.; Witte, D.P.; Cohen, M.B. Prevalence and Outcome of Allergic Colitis in Healthy Infants with Rectal Bleeding: A Prospective Cohort Study. J. Pediatr. Gastroenterol. Nutr. 2005, 41, 16–22.
- Calvani, M.; Anania, C.; Cuomo, B.; D’Auria, E.; Decimo, F.; Indirli, G.C.; Marseglia, G.; Mastrorilli, V.; Sartorio, M.U.A.; Santoro, A.; et al. Non–IgE- or Mixed IgE/Non–IgE-Mediated Gastrointestinal Food Allergies in the First Years of Life: Old and New Tools for Diagnosis. Nutrients 2021, 13, 226.
- Su, K.-W.; Shreffler, W.G.; Yuan, Q. Gastrointestinal Immunopathology of Food Protein–Induced Enterocolitis Syndrome and Other Non-Immunoglobulin E–Mediated Food Allergic Diseases. Ann. Allergy Asthma Immunol. 2021, 126, 516–523.
- Cianferoni, A. Food Protein-Induced Enterocolitis Syndrome Epidemiology. Ann. Allergy Asthma Immunol. 2021, 126, 469–477.
- Hoffmann, N.V.; Ahmed, A.; Fortunato, J.E. Food Protein-Induced Enterocolitis Syndrome (FPIES): Dynamic Relationship among Gastrointestinal Symptoms, Immune Response and the Autonomic Nervous System. Ann. Allergy Asthma Immunol. 2021, 126, 498–505.
- Nowak-Węgrzyn, A.; Chehade, M.; Groetch, M.E.; Spergel, J.M.; Wood, R.A.; Allen, K.; Atkins, D.; Bahna, S.; Barad, A.V.; Berin, C.; et al. International Consensus Guidelines for the Diagnosis and Management of Food Protein–Induced Enterocolitis Syndrome: Executive Summary—Workgroup Report of the Adverse Reactions to Foods Committee, American Academy of Allergy, Asthma & Immunology. J. Allergy Clin. Immunol. 2017, 139, 1111–1126.e4.
- Caubet, J.C.; Ford, L.S.; Sickles, L.; Järvinen, K.M.; Sicherer, S.H.; Sampson, H.A.; Nowak-Węgrzyn, A. Clinical Features and Resolution of Food Protein–Induced Enterocolitis Syndrome: 10-Year Experience. J. Allergy Clin. Immunol. 2014, 134, 382–389.e4.
- Agyemang, A.; Nowak-Wegrzyn, A. Food Protein-Induced Enterocolitis Syndrome: A Comprehensive Review. Clin. Rev. Allerg Immunol. 2019, 57, 261–271.
- Ishige, T.; Yagi, H.; Tatsuki, M.; Hatori, R.; Nishida, Y.; Takizawa, T.; Arakawa, H. Endoscopic Findings in the Acute Phase of Food Protein-Induced Enterocolitis Syndromae. Pediatr. Allergy Immunol. 2015, 26, 90–91.
- Hwang, J.-B.; Sohn, S.M.; Kim, A.S. Prospective Follow-up Oral Food Challenge in Food Protein-Induced Enterocolitis Syndrome. Arch. Dis. Child. 2009, 94, 425–428.
- Katz, Y.; Goldberg, M.R.; Rajuan, N.; Cohen, A.; Leshno, M. The Prevalence and Natural Course of Food Protein–Induced Enterocolitis Syndrome to Cow’s Milk: A Large-Scale, Prospective Population-Based Study. J. Allergy Clin. Immunol. 2011, 127, 647–653.e3.
- Ruffner, M.A.; Ruymann, K.; Barni, S.; Cianferoni, A.; Brown-Whitehorn, T.; Spergel, J.M. Food Protein-Induced Enterocolitis Syndrome: Insights from Review of a Large Referral Population. J. Allergy Clin. Immunol. Pract. 2013, 1, 343–349.
- Infante, S.; Cabrera-Freitag, P.; Morales-Cabeza, C.; Alvarez-Perea, A. Geographical Variations in Food Protein-Induced Enterocolitis Syndrome. Curr. Treat. Options Allergy 2019, 6, 309–321.
- Bird, J.A.; Barni, S.; Brown-Whitehorn, T.F.; du Toit, G.; Infante, S.; Nowak-Wegrzyn, A. FPIES Oral Food Challenge: Time for a Change? Ann. Allergy Asthma Immunol. 2021, 126, 506–515.
- Infante, S.; Marco-Martín, G.; Sánchez-Domínguez, M.; Rodríguez-Fernández, A.; Fuentes-Aparicio, V.; Alvarez-Perea, A.; Cabrera-Freitag, P.; Morales-Cabeza, C.; Zubeldia, J.M.; Zapatero, L. Food Protein-Induced Enterocolitis Syndrome by Fish: Not Necessarily a Restricted Diet. Allergy 2018, 73, 728–732.
- Infante, S.; Marco-Martín, G.; Zubeldia, J.M.; Fuentes-Aparicio, V.; Alvarez-Perea, A.; Cabrera-Freitag, P.; Morales-Cabeza, C.; Zapatero, L. Oral Food Challenge in Food Protein-Induced Enterocolitis Syndrome by Fish: Is There Any Room for Improvement? Int. Arch. Allergy Immunol. 2019, 179, 215–220.
- Mehr, S.; Campbell, D.E. Food Protein-induced Enterocolitis Syndrome: Guidelines Summary and Practice Recommendations. Med. J. Aust. 2019, 210, 94–99.
- Barni, S.; Vazquez-Ortiz, M.; Giovannini, M.; Liccioli, G.; Sarti, L.; Cianferoni, A.; Mori, F. Diagnosing Food Protein-induced Enterocolitis Syndrome. Clin. Exp. Allergy 2021, 51, 14–28.
- Zubeldia-Varela, E.; Barber, D.; Barbas, C.; Perez-Gordo, M.; Rojo, D. Sample Pre-Treatment Procedures for the Omics Analysis of Human Gut Microbiota: Turning Points, Tips and Tricks for Gene Sequencing and Metabolomics. J. Pharm. Biomed. Anal. 2020, 191, 113592.
- Eguiluz-Gracia, I.; Tay, T.R.; Hew, M.; Escribese, M.M.; Barber, D.; O’Hehir, R.E.; Torres, M.J. Recent Developments and Highlights in Biomarkers in Allergic Diseases and Asthma. Allergy 2018, 73, 2290–2305.
- Fritsché, R. Animal Models in Food Allergy: Assessment of Allergenicity and Preventive Activity of Infant Formulas. Toxicol. Lett. 2003, 140, 303–309.
- Schülke, S.; Albrecht, M. Mouse Models for Food Allergies: Where Do We Stand? Cells 2019, 8, 546.
- Burggraf, M.; Nakajima-Adachi, H.; Hachimura, S.; Ilchmann, A.; Pemberton, A.D.; Kiyono, H.; Vieths, S.; Toda, M. Oral Tolerance Induction Does Not Resolve Gastrointestinal Inflammation in a Mouse Model of Food Allergy. Mol. Nutr. Food Res. 2011, 55, 1475–1483.
- Mishra, A.; Hogan, S.P.; Brandt, E.B.; Rothenberg, M.E. An Etiological Role for Aeroallergens and Eosinophils in Experimental Esophagitis. J. Clin. Investig. 2001, 107, 83–90.
- Mishra, A.; Hogan, S.P.; Brandt, E.B.; Rothenberg, M.E. IL-5 Promotes Eosinophil Trafficking to the Esophagus. J. Immunol. 2002, 168, 2464–2469.
- Hogan, S.P.; Mishra, A.; Brandt, E.B.; Royalty, M.P.; Pope, S.M.; Zimmermann, N.; Foster, P.S.; Rothenberg, M.E. A Pathological Function for Eotaxin and Eosinophils in Eosinophilic Gastrointestinal Inflammation. Nat. Immunol. 2001, 2, 353–360.
- Gonipeta, B.; Kim, E.; Gangur, V. Mouse Models of Food Allergy: How Well Do They Simulate the Human Disorder? Crit. Rev. Food Sci. Nutr. 2015, 55, 437–452.
- Helm, R.M. Food Allergy Animal Models: An Overview. Ann. N. Y. Acad. Sci. 2002, 964, 139–150.
- Kanagaratham, C.; Sallis, B.F.; Fiebiger, E. Experimental Models for Studying Food Allergy. Cell. Mol. Gastroenterol. Hepatol. 2018, 6, 356–369.e1.
- Liu, T.; Navarro, S.; Lopata, A.L. Current Advances of Murine Models for Food Allergy. Mol. Immunol. 2016, 70, 104–117.
- Huang, J.; Liu, C.; Wang, Y.; Wang, C.; Xie, M.; Qian, Y.; Fu, L. Application of in Vitro and in Vivo Models in the Study of Food Allergy. Food Sci. Hum. Wellness 2018, 7, 235–243.
- Blanco-Pérez, F.; Kato, Y.; Gonzalez-Menendez, I.; Laiño, J.; Ohbayashi, M.; Burggraf, M.; Krause, M.; Kirberg, J.; Iwakura, Y.; Martella, M.; et al. CCR8 Leads to Eosinophil Migration and Regulates Neutrophil Migration in Murine Allergic Enteritis. Sci. Rep. 2019, 9, 9608.
- iHMP Consortium. The Integrative HMP (iHMP) Research Network Consortium The Integrative Human Microbiome Project. Nature 2019, 569, 641–648.
- Falony, G.; Joossens, M.; Vieira-Silva, S.; Wang, J.; Darzi, Y.; Faust, K.; Kurilshikov, A.; Bonder, M.J.; Valles-Colomer, M.; Vandeputte, D.; et al. Population-Level Analysis of Gut Microbiome Variation. Science 2016, 352, 560–564.
- Goodacre, R. Metabolomics of a Superorganism. J. Nutr. 2007, 137, 259S–266S.
- Yatsunenko, T.; Rey, F.E.; Manary, M.J.; Trehan, I.; Dominguez-Bello, M.G.; Contreras, M.; Magris, M.; Hidalgo, G.; Baldassano, R.N.; Anokhin, A.P.; et al. Human Gut Microbiome Viewed across Age and Geography. Nature 2012, 486, 222–227.
- Rojo, D.; Méndez-García, C.; Raczkowska, B.A.; Bargiela, R.; Moya, A.; Ferrer, M.; Barbas, C. Exploring the Human Microbiome from Multiple Perspectives: Factors Altering Its Composition and Function. FEMS Microbiol. Rev. 2017, 41, 453–478.
- Ruiz-Ruiz, S.; Sanchez-Carrillo, S.; Ciordia, S.; Mena, M.C.; Méndez-García, C.; Rojo, D.; Bargiela, R.; Zubeldia-Varela, E.; Martínez-Martínez, M.; Barbas, C.; et al. Functional Microbiome Deficits Associated with Ageing: Chronological Age Threshold. Aging Cell 2020, 19, e13063.
- Cseh, A.; Molnár, K.; Pintér, P.; Szalay, B.; Szebeni, B.; Treszl, A.; Arató, A.; Vásárhelyi, B.; Veres, G. Regulatory T Cells and T Helper Subsets in Breast-Fed Infants with Hematochezia Caused by Allergic Colitis. J. Pediatr. Gastroenterol. Nutr. 2010, 51, 675–677.
- Tan, J.; McKenzie, C.; Vuillermin, P.J.; Goverse, G.; Vinuesa, C.G.; Mebius, R.E.; Macia, L.; Mackay, C.R. Dietary Fiber and Bacterial SCFA Enhance Oral Tolerance and Protect against Food Allergy through Diverse Cellular Pathways. Cell Rep. 2016, 15, 2809–2824.
- Pascal, M.; Perez-Gordo, M.; Caballero, T.; Escribese, M.M.; Lopez Longo, M.N.; Luengo, O.; Manso, L.; Matheu, V.; Seoane, E.; Zamorano, M.; et al. Microbiome and Allergic Diseases. Front. Immunol. 2018, 9, 1584.
- Bunyavanich, S.; Shen, N.; Grishin, A.; Wood, R.; Burks, W.; Dawson, P.; Jones, S.M.; Leung, D.Y.M.; Sampson, H.; Sicherer, S.; et al. Early-Life Gut Microbiome Composition and Milk Allergy Resolution. J. Allergy Clin. Immunol. 2016, 138, 1122–1130.
- Fazlollahi, M.; Chun, Y.; Grishin, A.; Wood, R.A.; Burks, A.W.; Dawson, P.; Jones, S.M.; Leung, D.Y.M.; Sampson, H.A.; Sicherer, S.H.; et al. Early-Life Gut Microbiome and Egg Allergy. Allergy 2018, 73, 1515–1524.
- Berni Canani, R.; De Filippis, F.; Nocerino, R.; Paparo, L.; Di Scala, C.; Cosenza, L.; Della Gatta, G.; Calignano, A.; De Caro, C.; Laiola, M.; et al. Gut Microbiota Composition and Butyrate Production in Children Affected by Non-IgE-Mediated Cow’s Milk Allergy. Sci. Rep. 2018, 8, 12500.
- Pannaraj, P.S.; Li, F.; Cerini, C.; Bender, J.M.; Yang, S.; Rollie, A.; Adisetiyo, H.; Zabih, S.; Lincez, P.J.; Bittinger, K.; et al. Association Between Breast Milk Bacterial Communities and Establishment and Development of the Infant Gut Microbiome. JAMA Pediatr. 2017, 171, 647–654.
- Azad, M.B.; Konya, T.; Guttman, D.S.; Field, C.J.; Sears, M.R.; HayGlass, K.T.; Mandhane, P.J.; Turvey, S.E.; Subbarao, P.; Becker, A.B.; et al. Infant Gut Microbiota and Food Sensitization: Associations in the First Year of Life. Clin. Exp. Allergy 2015, 45, 632–643.
- Trompette, A.; Gollwitzer, E.S.; Yadava, K.; Sichelstiel, A.K.; Sprenger, N.; Ngom-Bru, C.; Blanchard, C.; Junt, T.; Nicod, L.P.; Harris, N.L.; et al. Gut Microbiota Metabolism of Dietary Fiber Influences Allergic Airway Disease and Hematopoiesis. Nat. Med. 2014, 20, 159–166.
- Obeso, D.; Mera-Berriatua, L.; Rodríguez-Coira, J.; Rosace, D.; Fernández, P.; Martín-Antoniano, I.A.; Santaolalla, M.; Marco Martín, G.; Chivato, T.; Fernández-Rivas, M.; et al. Multi-Omics Analysis Points to Altered Platelet Functions in Severe Food-Associated Respiratory Allergy. Allergy 2018, 73, 2137–2149.
- Wörheide, M.A.; Krumsiek, J.; Kastenmüller, G.; Arnold, M. Multi-Omics Integration in Biomedical Research—A Metabolomics-Centric Review. Anal. Chim. Acta 2021, 1141, 144–162.
- Díaz, M.; Guadamuro, L.; Espinosa-Martos, I.; Mancabelli, L.; Jiménez, S.; Molinos-Norniella, C.; Pérez-Solis, D.; Milani, C.; Rodríguez, J.M.; Ventura, M.; et al. Microbiota and Derived Parameters in Fecal Samples of Infants with Non-IgE Cow’s Milk Protein Allergy under a Restricted Diet. Nutrients 2018, 10, 1481.
- Candy, D.C.A.; Van Ampting, M.T.J.; Nijhuis, M.M.O.; Wopereis, H.; Butt, A.M.; Peroni, D.G.; Vandenplas, Y.; Fox, A.T.; Shah, N.; West, C.E.; et al. A Synbiotic-Containing Amino-Acid-Based Formula Improves Gut Microbiota in Non-IgE-Mediated Allergic Infants. Pediatr. Res. 2018, 83, 677–686.
- Fox, A.T.; Wopereis, H.; Van Ampting, M.T.J.; Nijhuis, M.M.O.; Butt, A.M.; Peroni, D.G.; Vandenplas, Y.; Candy, D.C.A.; Shah, N.; West, C.E.; et al. A Specific Synbiotic-Containing Amino Acid-Based Formula in Dietary Management of Cow’s Milk Allergy: A Randomized Controlled Trial. Clin. Transl. Allergy 2019, 9, 5.
- Wopereis, H.; van Ampting, M.T.J.; Cetinyurek-Yavuz, A.; Slump, R.; Candy, D.C.A.; Butt, A.M.; Peroni, D.G.; Vandenplas, Y.; Fox, A.T.; Shah, N.; et al. A Specific Synbiotic-Containing Amino Acid-Based Formula Restores Gut Microbiota in Non-IgE Mediated Cow’s Milk Allergic Infants: A Randomized Controlled Trial. Clin. Transl. Allergy 2019, 9, 27.
- Guadamuro, L.; Diaz, M.; Jimenez, S.; Molinos-Norniella, C.; Perez-Solis, D.; Miguel Rodriguez, J.; Bousono, C.; Gueimonde, M.; Margolies, A.; Delgado, S.; et al. Fecal Changes Following Introduction of Milk in Infants With Outgrowing Non-IgE Cow’s Milk Protein Allergy Are Influenced by Previous Consumption of the Probiotic LGG. Front. Immunol. 2019, 10, 1819.
- Aparicio, M.; Alba, C.; Rodríguez, J.M.; Fernández, L.; Proctocolitis Study Group of CAM Public Health Area 6. Microbiological and Immunological Markers in Milk and Infant Feces for Common Gastrointestinal Disorders: A Pilot Study. Nutrients 2020, 12, 634.
- Xiong, L.-J.; Xie, X.-L.; Li, Y.; Deng, X.-Z. Current Status of Fecal Calprotectin as a Diagnostic or Monitoring Biomarker for Cow’s Milk Protein Allergy in Children: A Scoping Review. World J. Pediatr. 2021, 17, 63–70.
- Stríz, I.; Trebichavský, I. Calprotectin—A Pleiotropic Molecule in Acute and Chronic Inflammation. Physiol. Res. 2004, 53, 245–253.
- Berni Canani, R.; Rapacciuolo, L.; Romano, M.T.; de Horatio, L.T.; Terrin, G.; Manguso, F.; Cirillo, P.; Paparo, F.; Troncone, R. Diagnostic Value of Faecal Calprotectin in Paediatric Gastroenterology Clinical Practice. Dig. Liver Dis. 2004, 36, 467–470.
- Bunn, S.K.; Bisset, W.M.; Main, M.J.C.; Golden, B.E. Fecal Calprotectin as a Measure of Disease Activity in Childhood Inflammatory Bowel Disease. J. Pediatric Gastroenterol. Nutr. 2001, 32, 171–177.
- Chang, M.-H.; Chou, J.-W.; Chen, S.-M.; Tsai, M.-C.; Sun, Y.-S.; Lin, C.-C.; Lin, C.-P. Faecal Calprotectin as a Novel Biomarker for Differentiating between Inflammatory Bowel Disease and Irritable Bowel Syndrome. Mol. Med. Rep. 2014, 10, 522–526.
- Beşer, Ö.F.; Sancak, S.; Erkan, T.; Kutlu, T.; Çokuğraş, H.; Çokuğraş, F.Ç. Can Fecal Calprotectin Level Be Used as a Markers of Inflammation in the Diagnosis and Follow-Up of Cow’s Milk Protein Allergy? Allergy Asthma Immunol. Res. 2014, 6, 33–38.
- Ataee, P.; Zoghali, M.; Nikkhoo, B.; Ghaderi, E.; Mansouri, M.; Nasiri, R.; Eftekhari, K. Diagnostic Value of Fecal Calprotectin in Response to Mother’s Diet in Breast-Fed Infants with Cow’s Milk Allergy Colitis. Iran. J. Pediatr. 2018, 28, e66172.
- Carrell, R.W.; Jeppsson, J.-O.; Laurell, C.-B.; Brennan, S.O.; Owen, M.C.; Vaughan, L.; Boswell, D.R. Structure and Variation of Human α 1-Antitrypsin. Nature 1982, 298, 329–334.
- Elli, L.; Topa, M.; Rimondi, A. Protein-Losing Enteropathy. Curr. Opin. Gastroenterol. 2020, 36, 238–244.
- Singer, A.A.M. Food Protein–Induced Enterocolitis and Alpha-1-Antitrypsin Deficiency. J. Allergy Clin. Immunol. 2020, 145, 444.
- Kalach, N.; Kapel, N.; Waligora-Dupriet, A.-J.; Castelain, M.-C.; Cousin, M.O.; Sauvage, C.; Ba, F.; Nicolis, I.; Campeotto, F.; Butel, M.J.; et al. Intestinal Permeability and Fecal Eosinophil-Derived Neurotoxin Are the Best Diagnosis Tools for Digestive Non-IgE-Mediated Cow’s Milk Allergy in Toddlers. Clin. Chem. Lab. Med. 2013, 51, 351–361.
More
Information
Subjects:
Allergy
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.2K
Revisions:
2 times
(View History)
Update Date:
27 Dec 2021
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




