Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Piotr Malara | + 1703 word(s) | 1703 | 2021-12-07 03:29:07 | | | |
| 2 | Yvaine Wei | + 3 word(s) | 1706 | 2021-12-27 01:44:05 | | | | |
| 3 | Yvaine Wei | Meta information modification | 1706 | 2021-12-27 01:49:08 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Malara, P. Anterior Open Bite Treatment with Skeletal Anchorage. Encyclopedia. Available online: https://encyclopedia.pub/entry/17558 (accessed on 07 February 2026).
Malara P. Anterior Open Bite Treatment with Skeletal Anchorage. Encyclopedia. Available at: https://encyclopedia.pub/entry/17558. Accessed February 07, 2026.
Malara, Piotr. "Anterior Open Bite Treatment with Skeletal Anchorage" Encyclopedia, https://encyclopedia.pub/entry/17558 (accessed February 07, 2026).
Malara, P. (2021, December 25). Anterior Open Bite Treatment with Skeletal Anchorage. In Encyclopedia. https://encyclopedia.pub/entry/17558
Malara, Piotr. "Anterior Open Bite Treatment with Skeletal Anchorage." Encyclopedia. Web. 25 December, 2021.
Copy Citation
Anterior open bite (AOB) is still one of the most difficult and demanding clinical problems. This malocclusion relies on a reduction in the vertical relationship between the incisal edges of the upper and lower incisors.
anterior open bite
molar intrusion
skeletal anchorage
orthognathic surgery
1. Introduction
There are many etiological factors of Anterior open bite (AOB). These include genetic, skeletal, dental and functional factors; factors related to the morphology of soft tissues; and habits [1]. Accompanying symptoms of AOB include increased lower face height (LFH), short posterior face height (PFH), increased gonial and mandibular plane angles and higher maxillary molar dentoalveolar height [2]. AOB is very often associated with numerous dental abnormalities, including tooth crowding, followed by problems with chewing food and speech, as well as aesthetic defects. Moreover, AOB is accompanied by muscular and functional problems, such as incompetence of the lips and a convex facial profile [3]. The development of AOB is also associated with the existence of parafunctions, which include thumb sucking or tongue thrust [4].
The development of orthodontics has provided many varieties of treatment for both dental and skeletal forms of AOB. The proposed treatment methods include both functional appliances and fixed appliances. Orthognathic surgical procedures also play an important role in the treatment [3].
In children, it is relatively simple to control facial growth through a variety of functional therapies. In this way, blocking the growth of the lateral parts of the alveolar process and provoking the growth of the dentoalveolar complex in the anterior region provide treatment options for AOB [5]. The treatment of AOB in non-growing patients and adults is much more difficult due to the inability to influence the skeletal development of the facial part of the skull, as well as the high susceptibility to relapse after orthodontic intervention in the dentoalveolar complex.
Traditionally, in patients with accomplished musculoskeletal development, the gold standard of treatment of AOB is orthognathic surgery [6]. The surgical treatment of AOB includes solely LeFort I osteotomy (LIO) or in conjunction with bilateral sagittal split osteotomy (BSSO) procedures performed on the mandible [1][7][8][9]. Orthognathic surgery modalities offer the best possible three-dimensional correction of both the facial skeleton and the dentoalveolar complex. It should be emphasized that the diverse range of procedures on the maxilla and the mandible that are collectively described as orthognathic surgery procedures are recognized to be safe surgical interventions [10][11].
Among the methods of AOB treatment, the intrusion of molars with the use of temporary anchorage devices (TADs) has a unique value. Mini-implants, mini-screws or mini-plates can be used as temporary skeletal anchorage [12]. The objective of this treatment option is to intrude the molar teeth by exerting a force between the temporary anchorage placed on the bone and the orthodontic appliance. This procedure allows a positive overbite to be achieved on the incisors by the intrusion of molar teeth followed by auto-rotation of the mandible [13].
The aim of orthodontic and surgical-orthodontic treatment is to correct malocclusion and achieve stable long-term treatment results. AOB is among the dentoalveolar and skeletal problems characterized by a high relapse rate [14]. Therefore, it is important to critically evaluate the newly introduced methods of treatment in terms of the stability of the achieved treatment effects.
2. Results of AOB Treatment Assessed by Achieving Positive Overbite on the Incisors and Other Parameters of AFH
Regardless of the treatment option chosen, the primary outcome of AOB treatment is a positive overbite on incisors. Changing the value from negative to positive indicated the correct treatment outcome on incisors, regardless of whether the treatment was based on molar intrusion TADs or as a result of maxillary or bimaxillary orthognathic surgery.
In all cases, AOB treatment resulted in a reduction in the measurements of AFH, understood as the linear distance between N and Me, and a decrease in LFH, defined as the linear distance between the anterior nasal spine (ANS) and Me or ANS-Me distance.
The values of overbite measured before and after AOB treatment using molar intrusion with skeletal anchorage alongside the calculated change in the vertical relationship between the incisal edges of U1 and L1 are summarized in Table 1, while the values of change in the distance of the mesial buccal cusp from PP are shown in Figure 1.
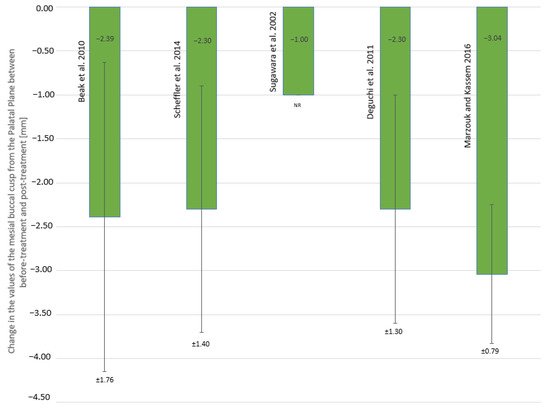
Figure 1. Change in the values of the distance of the mesial buccal cusp of the first upper molar from the palatal plane (mm); NR—not reported.
Table 1. The change in overbite measured on the incisors as a result of anterior open bite treatment by molar intrusion using skeletal anchorage (mm).
| Study | Pre-Treatment Mean (SD) |
Post-Treatment Mean (SD) |
Change in Mean (SD) |
|---|---|---|---|
| Baek et al. 2010 | −3.91 (1.65) | 1.65 (0.82) | 5.56 (1.94) * |
| Scheffler et al. 2014 | −1.2 (1.7) | 1.0 (NR) | 2.2 (1.6) SNR |
| Sugawara et al. 2002 | −2.8 (1.8) | 2.1 (0.8) | 4.9 (NR) SNR |
| Deguchi et al. 2011 | −4.4 (1.2) | 1.8 (1.1) | 6.2 (1.7) * |
| Marzouk and Kassem 2016 | −4.7 (2.3) | 2.18 (0.48) | 6.93 (1.99) ** |
NR—not reported; SD—standard deviation; * significant difference compared with pre-treatment (p < 0.05); ** significant difference compared with pre-treatment (p < 0.01); SNR—significance not reported.
The results of AOB treatment using orthognathic surgery techniques assessed on the basis of overbite are summarized in Table 2. The greatest overbite change was found in patients subjected to bimaxillary surgery in the studies by Ding et al. [9] (3.8 mm). It should be noted that in these studies there was also the highest negative overbite value on central incisors before surgery, amounting to -3.2 mm. After bimaxillary surgical treatment, the highest overbite of 1.3 ± 1.1 mm was obtained in the article by Fisher et al. [15]. In studies analyzing the results of AOB treatment with the division into maxillary and bimaxillary surgery, a greater value of overbite change was obtained in the group of patients who underwent maxillary surgery (3.78 mm) than in the group who underwent bimaxillary surgery (3.17 mm) [6]. At the same time, in the same studies, the highest value of overbite after surgery was obtained in the group of patients treated with LIO only (1.23 ± 1.05 mm).
Table 2. The change in overbite measured on the incisors as a result of orthognathic surgery (mm).
| Study | Pre-Treatment Mean (SD) |
Pre-Surgery Mean (SD) |
Post-Surgery Mean (SD) |
Change in Mean (SD) |
|---|---|---|---|---|
| Ding et al. 2007 | −3.2 (NR) | −3.2 (NR) | 0.6 (NR) | 3.8 (NR) |
| Teittinen et al. 2021 | NR NR |
−2.55 (1.41) M −2.19 (1.44) B |
1.23 (1.05) M 0.98 (1.53) B |
3.78 (NR) M 3.17 (NR) B |
| Swinnen et al. 2001 | −0.7 MI −2.1 ME |
−0.6 MI −1.9 ME |
1.3 MI 0.2 ME |
1.9 MI 2.1 ME |
| Fischer et al. 2000 | NR | −0.9 (2.6) | 1.3 (1.1) | 2.2 (2.4) |
| Proffit et al. 2000 | NR | NR | NR | NR |
NR—not reported; SD—standard deviation; M—maxillary group; B—bimaxillary group; MI—maxillary intrusion; ME—maxillary extrusion.
3. AOB Treatment with Molar Intrusion
With the advent of skeletal anchorage methods, molar intrusion has become an effective alternative to surgical-orthodontic complex treatment of AOB [7]. Orthodontic molar intrusion is a method that does not require patient cooperation, and the placement of TADs is a much less invasive procedure than orthognathic surgery [16].
It is emphasized that both orthodontic and surgical-orthodontic treatment modalities are associated with a high relapse rate [17]. Historically, many methods of purely orthodontic treatment of AOB have been used. In the case of orthodontic treatments of AOB with extractions, the relapse rate could be as high as 25.8% [14]. An even higher relapse rate of up to 38.1% was found in cases of traditional non-extraction AOB treatment [18].
In all articles on AOB treatment with molar intrusion, a positive overbite was achieved as a result of shortening the distance between the mesial buccal cusp of the first molar and PP. Another consequence of molar intrusion is the shortening of AFH affecting the facial appearance. The consequence of this phenomenon is also the CCW rotation of the mandible. The use of mini-plates fixed with bone screws at a zygomatic buttress significantly accelerated the pace of molar intrusion, made it possible to use greater orthodontic forces and reduced the risk of loosening of the anchoring elements [7][16].
It should be noted that prior to the introduction of TADs, traditional orthodontic treatment did not allow for a change in the occlusal plane of the maxilla through the intrusion of the molars, and thus did not allow for CCW rotation of the mandible [18]. Moreover, extrusion of incisors, which was possible without the use of TADs, was at risk of a much higher rate of relapse [14].
In the case of surgical-orthodontic treatment of AOB, significant differences in the change in AFH should be taken into account due to the different methods of surgical treatment used. The changes in AFH ranged from −0.8 mm in the case of surgical procedures with maxillary extrusion to as high as −5.5 mm in the case of surgical procedures with maxillary intrusion [19]. It appears that surgical methods of AOB could make major changes in AFH compared to AOB treated with molar teeth intrusion. It should be emphasized that, as a result of the surgical treatment of AOB with the use of BSSO, an increase in PFH can be achieved, which, according to some authors, is associated with a higher risk of relapse of AOB [20][21].
One of the effects of AOB treatment, regardless of the treatment method used, is the angular change in the position of the mandible. In the case of AOB treatment by molar intrusion, the position of the mandible changes as a result of mandibular autorotation. The same mechanism is the reason for changing the position of the mandible as a result of LIO orthognathic surgery.
Orthognathic surgery offers the possibility of changing the angular values of the position of not only the mandible but also the maxilla. The result of these procedures may be a positive change in the angle of PP to MP with slight negative changes in the angle of MP to the skull base. Therefore, in the group of patients with AOB treated with bimaxillary orthognathic surgery, slight negative changes in MP-SN of −1.3 degrees were obtained, accompanied by the largest changes of −6.1 degrees in MP-PP, resulting in significant changes of 3.8 mm in the mean overbite [9].
The treatment of AOB by molar intrusion allows a larger positive overbite on incisors than surgical treatment immediately after surgery, but a smaller range of changes in AFH or LFH, to be obtained. Molar intrusion in AOB treatment causes a greater CCW rotation of the mandible than AOB treatment with BSSO or bimaxillary surgery, but less than with LIO alone.
Since the treatment of AOB remains a demanding clinical problem for both orthodontists and maxillofacial surgeons, any attempt to introduce new treatments for this problem becomes extremely valuable, especially if the new treatment method is less invasive and remains at least comparably effective. In orthodontic and surgical treatment of malocclusion, it is extremely important to maintain stable treatment results and prevent complications.
References
- Baek, M.-S.; Choi, Y.-J.; Yu, H.-S.; Lee, K.-J.; Kwak, J.; Park, Y.-C. Long-Term Stability of Anterior Open-Bite Treatment by Intrusion of Maxillary Posterior Teeth. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 396.e1–396.e9.
- Lopez-Gavito, G.; Wallen, T.R.; Little, R.M.; Joondeph, D.R. Anterior Open-Bite Malocclusion: A Longitudinal 10-Year Postretention Evaluation of Orthodontically Treated Patients. Am. J. Orthod. 1985, 87, 175–186.
- Sandler, P.J.; Madahar, A.K.; Murray, A. Anterior Open Bite: Aetiology and Management. Dent. Update 2011, 38, 522–524, 527–528, 531–532.
- Leite, J.S.; Matiussi, L.B.; Salem, A.C.; Provenzano, M.G.A.; Ramos, A.L. Effects of Palatal Crib and Bonded Spurs in Early Treatment of Anterior Open Bite: A Prospective Randomized Clinical Study. Angle Orthod. 2016, 86, 734–739.
- Kim, Y.H.; Han, U.K.; Lim, D.D.; Serraon, M.L. Stability of Anterior Openbite Correction with Multiloop Edgewise Archwire Therapy: A Cephalometric Follow-up Study. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 43–54.
- Teittinen, M.; Tuovinen, V.; Tammela, L.; Schätzle, M.; Peltomäki, T. Long-Term Stability of Anterior Open Bite Closure Corrected by Surgical-Orthodontic Treatment. Eur. J. Orthod. 2012, 34, 238–243.
- Sugawara, J.; Baik, U.B.; Umemori, M.; Takahashi, I.; Nagasaka, H.; Kawamura, H.; Mitani, H. Treatment and Posttreatment Dentoalveolar Changes Following Intrusion of Mandibular Molars with Application of a Skeletal Anchorage System (SAS) for Open Bite Correction. Int. J. Adult Orthodon. Orthognath. Surg. 2002, 17, 243–253.
- Deguchi, T.; Kurosaka, H.; Oikawa, H.; Kuroda, S.; Takahashi, I.; Yamashiro, T.; Takano-Yamamoto, T. Comparison of Orthodontic Treatment Outcomes in Adults with Skeletal Open Bite between Conventional Edgewise Treatment and Implant-Anchored Orthodontics. Am. J. Orthod. Dentofac. Orthop. 2011, 139, S60–S68.
- Ding, Y.; Xu, T.-M.; Lohrmann, B.; Gellrich, N.-C.; Schwestka-Polly, R. Stability Following Combined Orthodontic-Surgical Treatment for Skeletal Anterior Open Bite—A Cephalometric 15-Year Follow-Up Study. J. Orofac. Orthop. 2007, 68, 245–256.
- Chow, L.K.; Singh, B.; Chiu, W.K.; Samman, N. Prevalence of Postoperative Complications after Orthognathic Surgery: A 15-Year Review. J. Oral Maxillofac. Surg. 2007, 65, 984–992.
- Panula, K.; Finne, K.; Oikarinen, K. Incidence of Complications and Problems Related to Orthognathic Surgery: A Review of 655 Patients. J. Oral Maxillofac. Surg. 2001, 59, 1128–1136; discussion 1137.
- Park, H.-S.; Kwon, O.-W.; Sung, J.-H. Nonextraction Treatment of an Open Bite with Microscrew Implant Anchorage. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 391–402.
- Erverdi, N.; Keles, A.; Nanda, R. The Use of Skeletal Anchorage in Open Bite Treatment: A Cephalometric Evaluation. Angle Orthod. 2004, 74, 381–390.
- Freitas, K.M.S.; de Freitas, M.R.; Henriques, J.F.C.; Pinzan, A.; Janson, G. Postretention Relapse of Mandibular Anterior Crowding in Patients Treated without Mandibular Premolar Extraction. Am. J. Orthod. Dentofac. Orthop. 2004, 125, 480–487.
- Fischer, K.; von Konow, L.; Brattström, V. Open Bite: Stability after Bimaxillary Surgery--2-Year Treatment Outcomes in 58 Patients. Eur. J. Orthod. 2000, 22, 711–718.
- Marzouk, E.S.; Kassem, H.E. Evaluation of Long-Term Stability of Skeletal Anterior Open Bite Correction in Adults Treated with Maxillary Posterior Segment Intrusion Using Zygomatic Miniplates. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 78–88.
- Proffit, W.R.; Bailey, L.J.; Phillips, C.; Turvey, T.A. Long-Term Stability of Surgical Open-Bite Correction by Le Fort I Osteotomy. Angle Orthod. 2000, 70, 112–117.
- Zuroff, J.P.; Chen, S.-H.; Shapiro, P.A.; Little, R.M.; Joondeph, D.R.; Huang, G.J. Orthodontic Treatment of Anterior Open-Bite Malocclusion: Stability 10 Years Postretention. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 302.e1–302.e8.
- Swinnen, K.; Politis, C.; Willems, G.; De Bruyne, I.; Fieuws, S.; Heidbuchel, K.; van Erum, R.; Verdonck, A.; Carels, C. Skeletal and Dento-Alveolar Stability after Surgical-Orthodontic Treatment of Anterior Open Bite: A Retrospective Study. Eur. J. Orthod. 2001, 23, 547–557.
- Proffit, W.R.; Bailey, L.J.; Phillips, C.; Turvey, T.A. Long-Term Stability of Surgical Open-Bite Correction by Le Fort I Osteotomy. Angle Orthod. 2000, 70, 112–117.
- Reyneke, J.P.; Ferretti, C. Anterior Open Bite Correction by Le Fort I or Bilateral Sagittal Split Osteotomy. Oral Maxillofac. Surg. Clin. N. Am. 2007, 19, 321–338.
More
Information
Subjects:
Dentistry, Oral Surgery & Medicine
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.1K
Revisions:
3 times
(View History)
Update Date:
29 Dec 2021
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




