
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Noriyuki Ogata | + 945 word(s) | 945 | 2021-11-22 03:25:07 | | | |
| 2 | Nora Tang | + 69 word(s) | 1014 | 2021-12-10 03:35:13 | | | | |
| 3 | Nora Tang | + 69 word(s) | 1014 | 2021-12-10 03:35:34 | | |
Video Upload Options
Image-enhanced endoscopy is useful for diagnosing and identifying lesions in the gastrointestinal tract. Recently, image-enhanced endoscopy has become a breakthrough technology that has attracted significant attention. This image enhancing technology is available for capsule endoscopy, which is an effective tool for small intestinal lesions and has been applied in flexible spectral color enhancement technology and in contrast capsule like narrow-band imaging.
1. Introduction
Capsule endoscopy (CE) was introduced in 2000 [1]. CE allows the visualization of the mucosa throughout the small intestine. Several studies have shown that CE is an effective means of detecting lesions in the small bowel, particularly sites of obscure gastrointestinal bleeding [2][3][4][5][6]. CE is also one of the standard modalities for monitoring Crohn’s disease [7][8][9][10][11][12][13]. Since 2004, image-enhanced endoscopy (IEE) has been reported to improve the detection and diagnosis of gastrointestinal lesions [14][15][16]. IEE techniques are useful for enhancing images of vasculature patterns, and for improving the visibility of surface patterns and color differences. Several IEE modalities are used in daily clinical practice, including narrow-band imaging (NBI, Olympus Corp., Tokyo, Japan), flexible spectral color enhancement (FICE, Fujifilm Corp., Tokyo, Japan), blue laser imaging (BLI, Fujifilm Corp., Tokyo, Japan), and linked color imaging (LCI, Fujifilm Corp., Tokyo, Japan) [17][18][19][20][21]. However, the diagnostic efficacy of CE is reduced when the identification of the mucosa is impaired due to the interference of bubbles, food residues, bile, and blood. Although the visibility might be improved by bowel preparation, there are limits to the effectiveness of bowel preparation for CE [22]. Therefore, IEE would be important for improving the identification of small bowel lesions in the presence of bile and blood. Furthermore, there is a problem with the diagnostic yield of CE because small lesions are difficult to detect and diagnose. Zheng et al. reported that the overall positive diagnostic yield of CE for small bowel disease remains at about 60% [23]. Thus, there is a need for IEE to enable the visualization of such lesions. A previous study reported that performing CE using a FICE digital processing system within a capsule workstation (Given Imaging, Yoqneam, Israel) is feasible [24]. Other reports have suggested that FICE may improve the visibility of small intestinal lesions [25][26]. Furthermore, a similar function for CE, developed by Olympus Inc., has shown promising results. The contrast capsule (CC) is an image-enhanced capsule endoscope (IECE) with blue-enhanced white light-emitting diodes (WL-LEDs) that allow high-contrast images to be obtained by selecting predominantly blue and green wavelengths of light [25].
This review aims to consolidate existing clinical data on the utility of IEE for improving the detection rate and characterization of small bowel pathological findings using CE, as compared to that of white light images (WLIs).
2. FICE
The FICE system was developed and introduced in 2005 as an image-processing tool for conventional video endoscopy. FICE is a digital processing method that uses WLIs and processes the images by emphasizing specific ranges of wavelengths. Three wavelengths (red, green, and blue) are selected and assigned to construct a complex enhanced image [26]. FICE has been hypothesized to enhance surface patterns and can improve the visualization and detection of lesions [27]. FICE is used in gastroscopy and colonoscopy to increase the detection rate of neoplastic lesions.
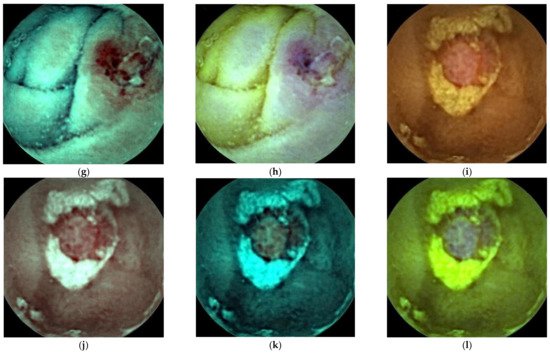
FICE is a digital image technology that uses the RAPID software (Given Imaging Ltd., Yoqneam, Israel), which enables the processing of regular images captured by normal video capsule devices ( Figure 1 ). The FICE wavelength settings are as follows: FICE 1 (red, 595 nm; green, 540 nm; blue, 535 nm); FICE 2 (red, 420 nm; green, 520 nm; blue 530 nm); and FICE 3 (red, 595 nm; green, 570 nm; blue, 415 nm). FICE 1 aims to reduce bile interference, FICE 2 aims to emphasize blood, and FICE 3 aims to emphasize the differences between bile and blood.
3. Contrast Capsule
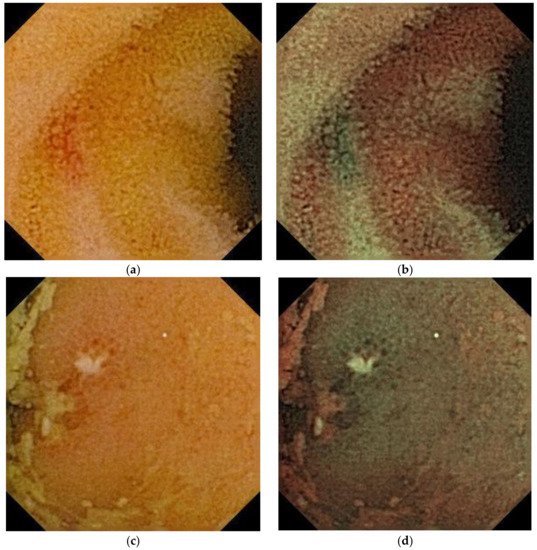
A CC is an image-enhanced CE. This is a normal capsule (EC type1, Olympus Corp.) equipped with a special WL-LED that was selected to increase the level of brightness in the blue wavelength range, which is appropriate for the visualization of hemoglobin. WLIs are generated using data from the three primary colors (red, green, and blue), conventionally obtained from a charge-coupled device. Contrast images (CIs) are generated from intentionally selecting the green and blue data ( Figure 2 ). This technology allows for stronger color contrast between hemoglobin and normal mucosa, potentially contributing to the detection of bleeding points. CC is classified as an optical-digital method, similar to NBI in the endoscopic imaging classification [28]. In 2011, Aihara et al. reported that CC visualized the color contrast between normal mucosa and small intestinal lesions, such as angioectasia, erosion/ulcer, and polyps [29].
4. Colon Capsule Endoscopy
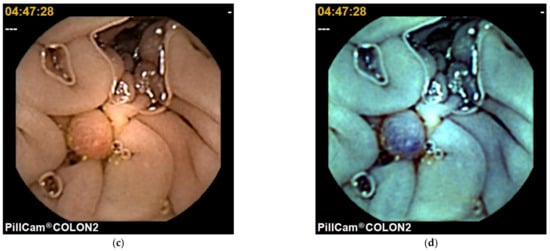
Colon CE (CCE) was introduced in 2006 [30]. A colonoscopy is a standard tool for colorectal examination. CCE is presented as a noninvasive alternative method for screening colon cancer [31]. In 2009, second generation CCE (CCE 2), which has improved sensitivity, was developed [32]. CCE 2 has good accuracy in the detection of polyps and colorectal cancer [33] and is useful for patients with Crohn’s disease and ulcerative colitis [34][35][36][37][38][39]. CCE 2 is equipped with a FICE system. In CCE 2, only the FICE 1 mode can be used ( Figure 3 ). Nakazawa et al. [40] showed that FICE 1 improved the ability to differentiate between adenomatous polyps and hyperplastic polyps compared to WLIs using the CIElab color space method. They investigated the ability of the ΔE to differentiate between adenomatous polyps and hyperplastic polyps. They reported that among 34 adenomatous polyps, the FICEΔE (39.2 ± 19.3) was significantly higher than the WLIΔE (14.9 ± 10.4) ( p < 0.001). In contrast, among 17 hyperplastic polyps, the FICEΔE (12.8 ± 10.4) was not significantly different from the WLIΔE (10.7 ± 6.8) ( p = 0.44). The FICEΔE of adenomatous polyps was 3.3 ± 1.8, which was significantly higher than the FICEΔE of hyperplastic polyps (1.3 ± 0.6; p < 0.001). Further large studies need to be conducted to confirm that FICE in CCE 2 is a highly useful modality for screening colon polyps.
References
- Iddan, G.; Meron, G.; Glukhovsky, A.; Swain, P. Wireless capsule endoscopy. Nature 2000, 405, 417.
- Apostolopoulos, P.; Liatsos, C.; Gralnek, I.M.; Kalantzis, C.; Giannakoulopoulou, E.; Alexandrakis, G.; Tsibouris, P.; Kalafatis, E.; Kalantzis, N. Evaluation of capsule endoscopy in active, mild-to-moderate, overt, obscure GI bleeding. Gastrointest. Endosc. 2007, 66, 1174–1181.
- Pennazio, M.; Santucci, R.; Rondonotti, E.; Abbiati, C.; Beccari, G.; Rossini, F.P.; De Franchis, R. Outcome of patients with obscure gastrointestinal bleeding after capsule endoscopy: Report of 100 consecutive cases. Gastroenterology 2004, 126, 643–653.
- Triester, S.L.; Leighton, J.A.; Leontiadis, G.I.; Fleischer, D.E.; Hara, A.K.; Heigh, R.I.; Shiff, A.D.; Sharma, V.K. A meta-analysis of the yield of capsule endoscopy compared to other diagnostic modalities in patients with obscure gastrointestinal bleeding. Am. J. Gastroenterol. 2005, 100, 2407–2418.
- Raju, G.S.; Gerson, L.; Das, A.; Lewis, B.; American Gastroenterological Association. American Gastroenterological Association (AGA) Institute medical position statement on obscure gastrointestinal bleeding. Gastroenterology 2007, 133, 1694–1696.
- Enns, R.A.; Hookey, L.; Armstrong, D.; Bernstein, C.N.; Heitman, S.J.; Teshima, C.; Leontiadis, G.I.; Tse, F.; Sadowski, D. Clinical Practice Guidelines for the Use of Video Capsule Endoscopy. Gastroenterology 2017, 152, 497–514.
- Choi, M.; Lim, S.; Choi, M.G.; Shim, K.N.; Lee, S.H. Effectiveness of Capsule Endoscopy Compared with Other Diagnostic Modalities in Patients with Small Bowel Crohn’s Disease: A Meta-Analysis. Gut Liver 2017, 11, 62–72.
- Han, Z.M.; Qiao, W.G.; Ai, X.Y.; Li, A.M.; Chen, Z.Y.; Feng, X.C.; Zhang, J.; Wan, T.M.; Xu, Z.M.; Bai, Y.; et al. Impact of capsule endoscopy on prevention of postoperative recurrence of Crohn’s disease. Gastrointest. Endosc. 2018, 87, 1489–1498.
- Melmed, G.Y.; Dubinsky, M.C.; Rubin, D.T.; Fleisher, M.; Pasha, S.F.; Sakuraba, A.; Tiongco, F.; Shafran, I.; Fernandez-Urien, I.; Rosa, B.; et al. Utility of video capsule endoscopy for longitudinal monitoring of Crohn’s disease activity in the small bowel: A prospective study. Gastrointest. Endosc. 2018, 88, 947–955.
- Hansel, S.L.; McCurdy, J.D.; Barlow, J.M.; Fidler, J.; Fletcher, J.G.; Becker, B.; Prabhu, N.C.; Faubion, W.A.; Hanson, K.A.; Kane, S.V.; et al. Clinical Benefit of Capsule Endoscopy in Crohn’s Disease: Impact on Patient Management and Prevalence of Proximal Small Bowel Involvement. Inflamm. Bowel Dis. 2018, 24, 1582–1588.
- Spiceland, C.M.; Lodhia, N. Endoscopy in inflammatory bowel disease: Role in diagnosis, management, and treatment. World J. Gastroenterol. 2018, 24, 4014–4020.
- Le Berre, C.; Trang-Poisson, C.; Bourreille, A. Small bowel capsule endoscopy and treat-to-target in Crohn’s disease: A systematic review. World J. Gastroenterol. 2019, 25, 4534–4554.
- Esaki, M.; Matsumoto, T.; Ohmiya, N.; Washio, E.; Morishita, T.; Sakamoto, K.; Abe, H.; Yamamoto, S.; Kinjo, T.; Togashi, K.; et al. Capsule endoscopy findings for the diagnosis of Crohn’s disease: A nationwide case-control study. J. Gastroenterol. 2019, 54, 249–260.
- Gono, K.; Obi, T.; Yamaguchi, M.; Ohyama, N.; Machida, H.; Sano, Y.; Yoshida, S.; Hamamoto, Y.; Endo, T. Appearance of enhanced tissue features in narrow-band endoscopic imaging. J. Biomed. Opt. 2004, 9, 568–577.
- Pohl, J.; May, A.; Rabenstein Pech, O.; Ell, C. Computed virtual chromoendoscopy: A new tool for enhancing tissue surface structures. Endoscopy 2007, 39, 80–83.
- Pohl, J.; May, A.; Rabenstein TPech, O.; Nguyen-Tat, M.; Fissler-Eckhoff, A.; Ell, C. Comparison of computed virtual chromoendoscopy and conventional chromoendoscopy with acetic acid for detection of neoplasia in Barrett’s esophagus. Endoscopy 2007, 39, 594–598.
- East, J.E.; Vleugels, J.L.; Roelandt, P.; Bhandari, P.; Bisschops, R.; Dekker, E.; Hassan, C.; Horgan, G.; Kiesslich, R.; Longcroft-Wheaton, G.; et al. Advanced endoscopic imaging: European Society of Gastrointestinal Endoscopy (ESGE) Technology Review. Endoscopy 2016, 48, 1029–1045.
- Ho, S.H.; Uedo, N.; Aso, A.; Shimizu, S.; Saito, Y.; Yao, K.; Goh, K.L. Development of Image-enhanced Endoscopy of the Gastrointestinal Tract: A Review of History and Current Evidences. J. Clin. Gastroenterol. 2018, 52, 295–306.
- Chiu, P.W.Y.; Uedo, N.; Singh, R.; Gotoda, T.; Ng, E.K.W.; Yao, K.; Ang, T.L.; Ho, S.H.; Kikuchi, D.; Yao, F.; et al. An Asian consensus on standards of diagnostic upper endoscopy for neoplasia. Gut 2019, 68, 186–197.
- Yoshida, N.; Hisabe, T.; Ikematsu, H.; Ishihara, H.; Terasawa, M.; Inaba, A.; Sato, D.; Cho, H.; Ego, M.; Tanaka, Y.; et al. Comparison Between Linked Color Imaging and Blue Laser Imaging for Improving the Visibility of Flat Colorectal Polyps: A Multicenter Pilot Study. Dig. Dis. Sci. 2020, 65, 2054–2062.
- Ono, S.; Kawada, K.; Dohi, O.; Kitamura, S.; Koike, T.; Hori, S.; Kanzaki, H.; Murao, T.; Yagi, N.; Sasaki, F.; et al. Linked Color Imaging Focused on Neoplasm Detection in the Upper Gastrointestinal Tract: A Randomized Trial. Ann. Intern. Med. 2021, 174, 18–24.
- Viazis, N.; Sgouros, S.; Papaxoinis, K.; Vlachogiannakos, J.; Bergele, C.; Sklavus, P.; Panari, A.; Avgerinos, A. Bowel preparation increases the diagnostic yield of capsule endoscopy: A prospective, randomized, controlled study. Gastrointest. Endosc. 2004, 60, 534–538.
- Zheng, Y.H.; Hawkins, L.; Wolff, J.; Goloubeva, O.; Goldberg, E. Detection of lesions during capsule endoscopy: Physician performance is disappointing. Am. J. Gastroenterol. 2012, 107, 554–560.
- Pohl, J.; Aschmoneit, I.; Schuhmann, S.; Ell, C. Computed image modification for enhancement of small-bowel surface structures at video capsule endoscopy. Endoscopy 2010, 42, 490–492.
- Ogata, N.; Ohtsuka, K.; Sasanuma, Y.; Ogawa, M.; Maeda, Y.; Ichimasa, K.; Mori, Y.; Misawa, M.; Kudo, T.; Hisayuki, T.; et al. White light-emitting contrast image capsule endoscopy for visualization of small intestine lesions: A pilot study. Endosc. Int. Open 2018, 6, E315–E321.
- ASGE Technology Committee; Manfredi, M.A.; Abu Dayyeh, B.K.; Bhat, Y.M.; Chauhan, S.S.; Gottlieb, K.T.; Hwang, J.H.; Komanduri, S.; Konda, V.; Lo, S.K.; et al. Electronic chromoendoscopy. Gastrointest. Endosc. 2015, 81, 249–261.
- Mishkin, D.S.; Chuttani, R.; Croffie, J.; Disario, J.; Liu, J.; Shah, R.; Somogyi, L.; Tierney, W.; Song, L.M.; Petersen, B.T. Technology Assessment Committee, American Society for Gastrointestinal Endoscopy. ASGE Technology Status Evaluation Report: Wireless capsule endoscopy. Gastrointest Endosc. 2006, 63, 539–545.
- Tajiri, H.; Niwa, H. Proposal for a consensus terminology in endoscopy: How should different endoscopic imaging techniques be grouped and defined? Endoscopy 2008, 40, 775–778.
- Aihara, H.; Ikeda, K.; Tajiri, H. Image-enhanced capsule endoscopy based on the diagnosis of vascularity when using a new type of capsule. Gastrointest. Endosc. 2011, 73, 1274–1279.
- Eliakim, R.; Fireman, Z.; Gralnek, I.M.; Yassin, K.; Waterman, M.; Kopelman, Y.; Lachter, J.; Koslowsky, B.; Adler, S.N. Evaluation of the PillCam Colon capsule in the detection of colonic pathology: Results of the first multicenter, prospective, comparative study. Endoscopy 2006, 38, 963–970.
- Van Gossum, A.; Munoz-Navas, M.; Fernandez-Urien, I.; Carretero, C.; Gay, G.; Delvaux, M.; Lapalus, M.G.; Ponchon, T.; Neuhaus, H.; Philipper, M.; et al. Capsule endoscopy versus colonoscopy for the detection of polyps and cancer. N. Engl. J. Med. 2009, 361, 264–270.
- Eliakim, R.; Yassin, K.; Niv, Y.; Metzger, Y.; Lachter, J.; Gal, E.; Sapoznikov, B.; Konikoff, F.; Leichtmann, G.; Fireman, Z.; et al. Prospective multicenter performance evaluation of the second-generation colon capsule compared with colonoscopy. Endoscopy 2009, 41, 1026–1031.
- Spada, C.; Pasha, S.F.; Gross, S.A.; Leighton, J.A.; Schnoll-Sussman, F.; Correale, L.; González Suárez, B.; Costamagna, G.; Hassan, C. Accuracy of First- and Second-Generation Colon Capsules in Endoscopic Detection of Colorectal Polyps: A Systematic Review and Meta-analysis. Clin. Gastroenterol. Hepatol. 2016, 14, 1533–1543.
- D’Haens, G.; Löwenberg, M.; Samaan, M.A.; Franchimont, D.; Ponsioen, C.; van den Brink, G.R.; Fockens, P.; Bossuyt, P.; Amininejad, L.; Rajamannar, G.; et al. Safety and Feasibility of Using the Second-Generation Pillcam Colon Capsule to Assess Active Colonic Crohn’s Disease. Clin. Gastroenterol. Hepatol. 2015, 13, 1480–1486.
- Oliva, S.; Cucchiara, S.; Civitelli, F.; Casciani, E.; Di Nardo, G.; Hassan, C.; Papoff, P.; Cohen, S.A. Colon capsule endoscopy compared with other modalities in the evaluation of pediatric Crohn’s disease of the small bowel and colon. Gastrointest. Endosc. 2016, 83, 975–983.
- Oliva, S.; Aloi, M.; Viola, F.; Mallardo, S.; Civitelli, F.; Maccioni, F.; Hassan, C.; Papoff, P.; Cucchiara, S.; Cohen, S.A. A Treat to Target Strategy Using Panenteric Capsule Endoscopy in Pediatric Patients With Crohn’s Disease. Clin. Gastroenterol. Hepatol. 2019, 17, 2060–2067.
- Sung, J.; Ho, K.Y.; Chiu, H.M.; Ching, J.; Travis, S.; Peled, R. The use of Pillcam Colon in assessing mucosal inflammation in ulcerative colitis: A multicenter study. Endoscopy 2012, 44, 754–758.
- Shi, H.Y.; Chan, F.K.L.; Higashimori, A.; Kyaw, M.; Ching, J.Y.L.; Chan, H.C.H.; Chan, J.C.H.; Chan, A.W.H.; Lam, K.L.Y.; Tang, R.S.Y.; et al. A prospective study on second-generation colon capsule endoscopy to detect mucosal lesions and disease activity in ulcerative colitis (with video). Gastrointest. Endosc. 2017, 86, 1139–1146.
- Hosoe, N.; Nakano, M.; Takeuchi, K.; Endo, Y.; Matsuoka, K.; Abe, T.; Omori, T.; Hayashida, M.; Kobayashi, T.; Yoshida, A.; et al. Establishment of a Novel Scoring System for Colon Capsule Endoscopy to Assess the Severity of Ulcerative Colitis-Capsule Scoring of Ulcerative Colitis. Inflamm. Bowel Dis. 2018, 24, 2641–2647.
- Nakazawa, K.; Nouda, S.; Kakimoto, K.; Kinoshita, N.; Tanaka, Y.; Tawa, H.; Koshiba, R.; Naka, Y.; Hirata, Y.; Ota, K.; et al. The Differential Diagnosis of Colorectal Polyps Using Colon Capsule Endoscopy. Intern. Med. 2021, 60, 1805–1812.




