1000/1000
Hot
Most Recent

| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Nipith Charoenngam | + 2222 word(s) | 2222 | 2021-10-13 09:00:39 | | | |
| 2 | Lindsay Dong | + 248 word(s) | 2470 | 2021-11-22 04:27:30 | | | | |
| 3 | Lindsay Dong | + 248 word(s) | 2470 | 2021-11-22 04:27:50 | | |
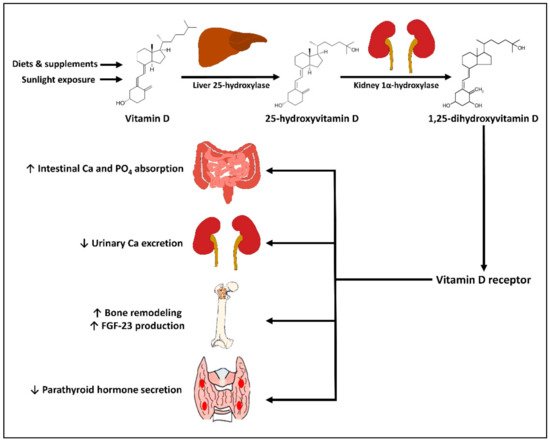
Vitamin D plays an important role in maintaining a healthy mineralized skeleton. It is also considered an immunomodulatory agent that regulates innate and adaptive immune systems. The aim of this narrative review is to provide general concepts of vitamin D for the skeletal and immune health, and to summarize the mechanistic, epidemiological, and clinical evidence on the relationship between vitamin D and rheumatic diseases. Multiple observational studies have demonstrated the association between a low level of serum 25-hydroxyvitamin D [25(OH)D] and the presence and severity of several rheumatic diseases, such as rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), spondyloarthropathies, and osteoarthritis (OA). Nevertheless, the specific benefits of vitamin D supplements for the treatment and prevention of rheumatic diseases are less accepted as the results from randomized clinical trials are inconsistent, although some conceivable benefits of vitamin D for the improvement of disease activity of RA, SLE, and OA have been demonstrated in meta-analyses. It is also possible that some individuals might benefit from vitamin D differently than others, as inter-individual difference in responsiveness to vitamin D supplementation has been observed in genomic studies. Although the optimal level of serum 25(OH)D is still debatable, it is advisable it is advisable that patients with rheumatic diseases should maintain a serum 25(OH)D level of at least 30 ng/mL (75 nmol/L) to prevent osteomalacia, secondary osteoporosis, and fracture, and possibly 40–60 ng/mL (100–150 nmol/L) to achieve maximal benefit from vitamin D for immune health and overall health.
Vitamin D is believed to play a role in modulating the pathogenesis and disease activity of RA, based on the actions of 1,25(OH)2D on the adaptive immune response that suppresses the proliferation and activity of TH1 and TH17 and enhances the Treg activity [12]. Furthermore, genomic studies have shown that certain polymorphisms of the gene encoding VDR and DBP are associated with susceptibility to RA, suggesting that the vitamin D signaling pathway may be involved in the pathogenesis of RA [13][14].
Multiple observational studies have shown the association of vitamin D status or intake with incidence and severity of RA [15]. For example, in a prospective cohort study by Merlino et al., women in the highest tertile of vitamin D intake had a lower risk for RA by 33% compared with those in the lowest tertile [16]. Moreover, a higher amount of ultraviolet B exposure was shown to be associated with a decreased risk of incident RA in the Nurse Health Study cohort of 106,368 women aged 30–55 years old [17]. This finding is in line with the evidence that the risks of some immune-mediated diseases (e.g., type 1 diabetes, multiple sclerosis, and RA) are higher in high-latitude regions where there is a relatively low amount of ultraviolet radiation and a high prevalence of vitamin D deficiency [18][19]. These observations, therefore, support that vitamin D obtained from either oral intake or sunlight exposure could possibly be protective against RA. In the COMOrbidities in Rheumatoid Arthritis (COMORA) study consisting of 1413 patients with RA from 15 countries, the serum level of 25(OH)D was inversely correlated with disease activity, as assessed by the Disease Activity Score-28 (DAS28) after adjusting for potential confounders [20].