
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Barthelemy TOSELLO | + 2878 word(s) | 2878 | 2021-10-25 10:33:27 | | | |
| 2 | Beatrix Zheng | + 1151 word(s) | 4029 | 2021-11-03 04:58:06 | | |
Video Upload Options
School-aged extremely preterm (EPT) children have multiple specific neurocognitive/behavioral disorders that are often associated with other disorders; this manifests a true neurobehavioral “phenotype” of prematurity. To determine a profile of cognitive/behavioral impairments in a population of school-aged EPT children (7–10 years-old) without major disabilities, a cross-sectional study was conducted in five medical centers. An algorithm distributed the study population according to four WISC-IV subtests, five NEPSY-2 subtests, and two variables of figure of Rey.
1. Introduction
There is a remarkable consistency in outcomes over time and between countries, cultures, and healthcare systems, which provides evidence for a universal “preterm phenotype” associated with the neurodevelopmental immaturity conferred by a VP birth [1]. Relative to those born at term, very preterm (VP) children are at an increased risk for cognitive impairments, attention deficits, and social–emotional problems. However, there is no increased risk for disruptive or oppositional behavioral problems [2]. Moreover, developmental coordination disorders (DCD) are associated with behavioral, cognitive, and/or attention disorders [3][4] in EPT school-aged children who are free from severe deficiencies. In addition, two meta-analyses confirm a high prevalence of psychiatric disorders in children and adults born prematurely as compared to a population born at term. These VP children have a high risk of attention disorders with or without hyperactivity, autism spectrum, and anxiety disorders [1][5]. However, these disorders are always accompanied by cognitive, neurological, and learning comorbidities [6].
As traditionally seen in the literature in cohort populations, the cognitive fate of premature children is usually classified into four groups: (1) absence of incapacity, (2) minor disability, (3) moderate disability, and (4) severe disability, based on data from the total Full Scale Intelligent Quotient (FSIQ) scores. A threshold of ≥89 is considered normal, which is a low average [4][7]. However, the performances observed with a total FSIQ are the result of a complex processes involving multiple intellectual and non-intellectual characteristics (attention, emotions, motivation, movement planning, etc.) [8]. Furthermore, for infants born prematurely, the FSIQ is most often calculated on a dissociated subtest value that is not necessarily reflective of the child’s cognitive function and thus constitutes a false methodology [8]. The analysis of the subtests’ dispersions aims to highlight those that deserve a thorough interpretation. Indeed, a child considered “normal” is likely to have impairments such as a dysexecutive syndrome and/or impaired behavior and/or DCD that could disrupt brain function.
Therefore, most longitudinal studies focus on general mental health classifications rather than individual clinical diagnostic criteria and comorbidity profiles (motor and behavior). Since some outcomes may be deteriorating rather than improving over time, knowledge of all comorbidities may be useful in improving an early identification of the highest risk children in order to address their clinical needs. Inclusion of behavioral difficulties and developmental coordination disorders with the definition of mild neurodevelopmental disabilities describes, in more depth, the complexity of those difficulties faced by these preterm children [9].
In fact, there have been few studies directed on individual clinical descriptions in which discrete or non-specific signs of psychiatric disorders and/or subtle impairments of executive functions occur together and/or are associated with cognitive and/or neurological impairments in school-aged VP children. To our knowledge, only one study of these children who share similar profiles within a group on measurements of intelligence and executive functions does not take into account behavior [8]. The assessment of a true neurobehavioral “phenotype” (NBP) of prematurity, which takes into account not only the FSIQ but also executive functions, neurologic examinations, and behavior should be a principal objective of epidemiological research on prematurity [8]. Finally, no studies have measured this neurobehavioral profile and its social consequences particularly on the QoL of these children.
2. Analysis on Research Results
2.1. Population
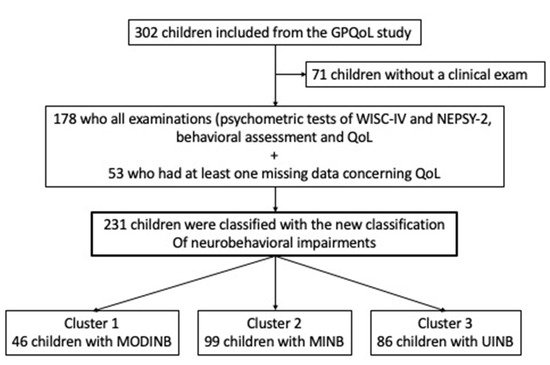
2.2. Cognitive/Behavioral Impairments Profiles from New Classification
-
Cluster 1 Moderate Impaired NeuroBehavior (MODINB) with multiple impairments and behavior troubles (n = 46 (20%));
-
Cluster 2 Minor Impaired NeuroBehavior (MINB) with less severe multiple impairments and behavioral troubles, (n = 99 (43%)); and
-
Cluster 3 (n = 86 (37%)), UnImpaired NeuroBehavior (UINB), with only slight emotional symptoms (mean score: 3.5 (SDs) = 2.56: slightly below average, therefore pathological), with a normal neurocognitive assessment outcome.
| Characteristics of Clustered Pooling (N = 231) | ||||||
|---|---|---|---|---|---|---|
| MODINB Cluster 1 (N = 46) |
MINB Cluster 2 (N = 99) |
UINB Cluster 3 (N = 86) |
P | |||
| Perinatal characteristics | ||||||
| GA in WA, mean (SD) | 26.13 (0.96) | 26.25 (0.82) | 26.29 (0.92) | 0.607 | ||
| Weight in grams, mean (SD) | 858.91 (181.77) | 878.77 (194.69) | 901.31 (171.47) | 0.430 | ||
| Male, n (%) | 20 (43.48) | 50 (51.02) | 38 (44.71) | 0.594 | ||
| SGA, n (%) | 5 (10.87) | 10 (10.10) | 1 (1.16) | 0.011 * | ||
| Multiple pregnancies, n (%) | 17 (36.96) | 30 (30.30) | 31 (36.05) | 0.625 | ||
| Severe BPD, n (%) | 25 (54.35) | 46 (47.92) | 47 (54.65) | 0.613 | ||
| Average age of child at the study inclusion, mean (SD) | 8.69 (0.65) | 8.43 (0.74) | 8.39 (0.72) | 0.056 | ||
| Parents’ educational level, professional activity, and socioeconomic status of family | ||||||
| Parents without higher education level, n (%) | 29 (74.36) | 46 (47.92) | 18 (21.43) | <0.001 * | ||
| Professional activity of parents, n (%) | 0.004 * | |||||
| Without professional activity | 8 (18.60) | 7 (7.14) | 3 (3.53) | |||
| Professional activity of one of two parents | 16 (37.21) | 37 (37.76) | 20 (23.53) | |||
| Professional activity of both parents | 19 (44.19) | 54 (55.10) | 62 (72.94) | |||
| Professional activity of mother, n (%) | 21 (48.84) | 63 (64.29) | 66 (79.52) | 0.002 | ||
| Professional activity of father, n (%) | 33 (82.50) | 82 (89.13) | 78 (92.86) | 0.243 | ||
| Elevated FAS Score, n (%) | 21 (45.65) | 57 (58.76) | 57 (67.06) | 0.059 | ||
| Quality of life 1, mean (SD) | ||||||
| VSP-Ae global index (evaluation by the child) | 64.38 (12.55) | 70.30 (13.07) | 70.16 (13.06) | 0.029 * | ||
| VSP-Ap global index (evaluation by the parents) | 64.38 (12.35) | 70.66 (10.51) | 71.25 (10.61) | 0.008 * | ||
| Kidscreen global index (evaluation by the child) | 68.43 (16.65) | 73.26 (17.43) | 71.91 (17.30) | 0.293 | ||
| Kidscreen global index (evaluation by the parents) | 62.52 (16.54) | 70.16 (14.50) | 71.33 (13.39) | 0.003 * | ||
| Neurocognitive assessment 2 | ||||||
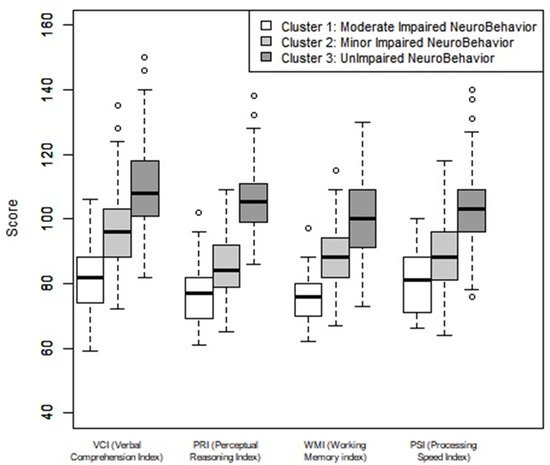
| WISC-IV 2a, mean (SD) | ||||||
| VCI (Verbal comprehension index) | 80.93 (9.46) | 96.56 (11.75) | 109.51 (12.74) | <0.001 * | ||
| PRI (Perceptional reasoning index) | 77.26 (8.99) | 85.41 (9.24) | 106.73 (9.94) | <0.001 * | ||
| WMI (Working memory index) | 74.93 (11.07) | 88.85 (9.38) | 101.15 (11.41) | <0.001 * | ||
| PSI (Processing speed index) | 80.15 (8.96) | 88.49 (10.75) | 102.90 (12.61) | <0.001 * | ||
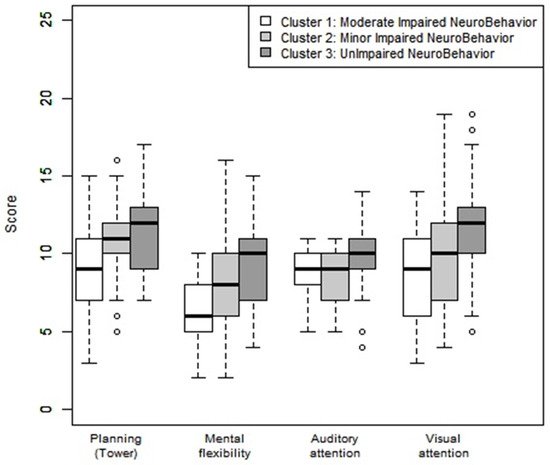
| NEPSY-2 2b, mean (SD) | ||||||
| Planification score (Tower) | 8.80 (3.04) | 10.81 (2.33) | 11.52 (2.43) | <0.001 * | ||
| Mental flexibility score | 6.50 (2.27) | 7.76 (2.72) | 9.48 (2.68) | <0.001 * | ||
| Auditive attention score | 8.61 (1.34) | 8.45 (1.51) | 9.66 (1.73) | <0.001 * | ||
| Visual attention score | 8.98 (2.73) | 9.78 (3.47) | 11.64 (3.03) | <0.001 * | ||
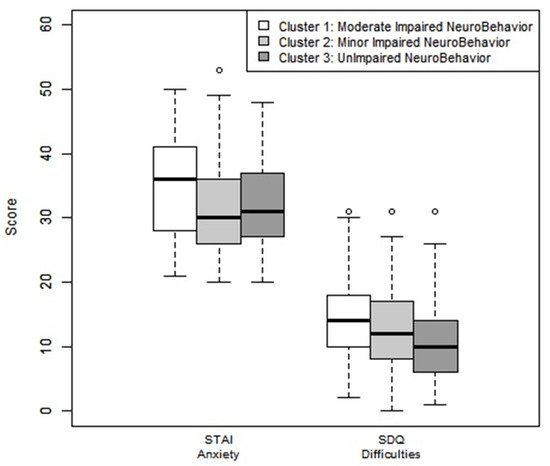
| Goodman-SDQ-parents 3, mean (SD) | ||||||
| Emotional symptoms | 4.05 (2.62) | 3.64 (2.37) | 3.15 (2.56) | 0.136 | ||
| Behavioral problems | 2.52 (1.99) | 1.94 (1.93) | 1.64 (1.73) | 0.040 * | ||
| Hyperactivity/Inattention | 5.32 (2.45) | 4.89 (2.56) | 3.93 (2.74) | 0.007 * | ||
| Relationship problems with others | 2.23 (1.92) | 2.17 (1.98) | 1.55 (1.77) | 0.051 | ||
| Prosocial behaviors | 8.59 (1.59) | 8.61 (1.70) | 8.89 (1.42) | 0.412 | ||
| Total difficulty scores | 14.11 (6.39) | 12.64 (6.63) | 10.27 (5.78) | 0.002 * | ||
| Anxiety, mean (SD) | ||||||
| Spielberg Index (STAIC) 4 | 35.30 (8.28) | 31.90 (7.71) | 32.25 (6.89) | 0.035 * | ||
| Impairment 5 | ||||||
| Language delay 5a, n (%) | 30 (65.22) | 16 (16.16) | 1 (1.16) | <0.001 * | ||
| Delay in visuospatial integration 5b, n (%) | 17 (36.96) | 18 (18.18) | 0 (0.00) | <0.001 * | ||
| Attention deficit disorder 5c, n (%) | 15 (32.61) | 19 (19.19) | 2 (2.33) | <0.001 * | ||
| Dysexecutive disorder 5d, n (%) | 44 (95.65) | 67 (67.68) | 26 (30.23) | <0.001 * | ||
| Ideomotor dyspraxia 5e, n (%) | 14 (30.43) | 10 (10.10) | 0 (0.00) | <0.001 * | ||
2.3. Neurobehavioral Impairment Profiles: Behavioral and Neurocognitive Comorbidities
2.4. Neurobehavioral Cognitive Assessment by Cluster
2.5. Correlation of Population Study and Quality of Life
| Quality of Life between Study Population vs. Reference Population | Quality of Life between Three Clusters | Quality of Life between Cluster 3 vs. Reference Population | ||||||||||||||||||||||
| Study Population (n = 178) |
Reference Population a | Difference | p | Effect Size 3 (Ranking) | Cluster 1 b (n = 32) |
Cluster 2 c (n = 79) |
Cluster 3 d (n = 67) |
p | Reference Population | Difference | p | Effect Size 3 (Ranking) | ||||||||||||
| Mean | SD | Expected Mean | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Expected Mean | Mean | SD | |||||||||||
| VSP-A ENFANT 1 | ||||||||||||||||||||||||
| Vitality | 77.50 | 19.90 | 82.46 | −4.95 | 19.96 | 0.001 * | −0.25 | 77.03 | 20.90 | 77.22 | 19.77 | 78.06 | 0.958 | 82.31 | −4.25 | 19.77 | 0.083 | −0.22 | ||||||
| General well- being | 72.61 | 17.93 | 78.38 | −5.77 | 18.02 | <0.001 * | −0.32 | 68.15 | 17.56 | 74.33 | 17.23 | 72.72 | 18.79 | 0.259 | 78.42 | −5.70 | 18.73 | 0.015 * | −0.3 | 3 | ||||
| Relationship with friends | 46.89 | 28.11 | 58.91 | −12.02 | 28.17 | <0.001 * | −0.43 | 2 | 43.29 | 24.81 | 46.70 | 28.66 | 48.82 | 29.14 | 0.659 | 58.89 | −10.07 | 29.37 | 0.006 * | −0.34 | 1 | |||
| Leisure | 62.86 | 20.52 | 69.63 | −6.77 | 20.57 | <0.001 * | −0.33 | 3 | 60.16 | 18.21 | 63.96 | 20.81 | 62.85 | 21.37 | 0.679 | 69.39 | −6.54 | 21 | 0.013 * | −0.31 | 2 | |||
| Relationship with family | 74.10 | 19.05 | 73.19 | 0.91 | 19.10 | 0.528 | 0.05 | 74.38 | 17.33 | 74.97 | 18.55 | 72.94 | 20.58 | 0.813 | 73.00 | −0.06 | 20.77 | 0.981 | 0 | |||||
| School work | 76.19 | 23.50 | 82.08 | −5.88 | 23.45 | 0.001 * | −0.25 | 60.94 | 24.75 | 78.8 | 21.87 | 80.41 | 22.11 | <0.001 * | 82.16 | −1.75 | 21.98 | 0.518 | −0.08 | |||||
| Self esteem | 74.20 | 21.33 | 84.61 | −10.41 | 21.42 | <0.001 * | −0.49 | 1 | 63.54 | 22.71 | 74.74 | 21.39 | 78.67 | 19.00 | 0.004 * | 84.49 | −5.82 | 19.25 | 0.016 * | −0.3 | ||||
| Total index | 69.19 | 13.56 | 75.59 | −6.40 | 13.65 | <0.001 * | −0.47 | 63.93 | 11.5 | 70.1 | 13.35 | 70.64 | 14.27 | 0.050 | 75.51 | −4.87 | 14.31 | 0.007 * | −0.34 | |||||
| VSP-PARENTS 1 | ||||||||||||||||||||||||
| Vitality | 69.92 | 16.15 | 77.38 | −7.46 | 16.26 | <0.001 * | −0.46 | 65.23 | 16.43 | 69.86 | 16.14 | 72.23 | 15.77 | 0.131 | 77.36 | −5.13 | 15.66 | 0.009 * | −0.33 | 3 | ||||
| Psychological well-being | 70.19 | 20.43 | 81.34 | −11.15 | 20.50 | <0.001 * | −0.54 | 1 | 70.23 | 25.58 | 70.46 | 19.08 | 69.85 | 19.53 | 0.984 | 81.19 | −11.34 | 19.57 | <0.001 * | −0.58 | 1 | |||
| Relationship with friends | 59.18 | 20.04 | 64.53 | −5.36 | 20.15 | <0.001 * | −0.27 | 53.45 | 20.28 | 59.49 | 21.28 | 61.54 | 18.08 | 0.169 | 64.71 | −3.17 | 18.43 | 0.163 | −0.17 | |||||
| Leisure | 52.41 | 18.32 | 57.01 | −4.60 | 18.30 | 0.001 * | −0.25 | 50.13 | 17.53 | 54.11 | 19.03 | 51.49 | 17.91 | 0.512 | 57.85 | −5.36 | 17.85 | 0.017 * | −0.3 | |||||
| Relationship with family | 77.21 | 13.65 | 78.62 | −1.41 | 13.69 | 0.172 | −0.10 | 75.91 | 16.08 | 78.80 | 13.63 | 75.96 | 12.39 | 0.386 | 78.51 | −2.55 | 12.32 | 0.095 | −0.21 | |||||
| Physical well being | 75.78 | 16.18 | 78.60 | −2.82 | 16.19 | 0.021 * | −0.17 | 74.28 | 16.32 | 76.58 | 17.03 | 75.56 | 15.26 | 0.789 | 78.38 | −2.82 | 15 | 0.129 | −0.19 | |||||
| Relationship with teacher | 73.17 | 18.46 | 75.16 | −1.99 | 18.67 | 0.157 | −0.11 | 70.31 | 19.28 | 74.26 | 17.05 | 73.26 | 19.76 | 0.596 | 75.32 | −2.06 | 19.78 | 0.398 | −0.1 | |||||
| School work | 69.66 | 20.14 | 79.80 | −10.14 | 20.18 | <0.001 * | −0.50 | 2 | 60.94 | 22.17 | 67.41 | 18.17 | 76.49 | 19.40 | 0.001 * | 79.92 | −3.43 | 19.67 | 0.158 | −0.17 | ||||
| Self esteem | 78.93 | 27.33 | 88.44 | −9.50 | 27.43 | <0.001 * | −0.35 | 62.11 | 32.14 | 81.17 | 24.59 | 84.33 | 25.13 | <0.001 * | 88.09 | −3.76 | 25.71 | 0.236 | −0.15 | |||||
| General well- being | 72.72 | 15.81 | 80.12 | −7.41 | 15.89 | <0.001 * | −0.47 | 3 | 72.19 | 18.24 | 73.20 | 15.28 | 72.40 | 15.42 | 0.935 | 79.94 | −7.54 | 15.38 | <0.001 * | −0.49 | 2 | |||
| Total Index | 69.61 | 11.17 | 75.96 | −6.36 | 11.23 | <0.001 * | −0.57 | 64.73 | 12.38 | 70.24 | 10.59 | 71.19 | 10.75 | 0.021 * | 75.89 | −4.69 | 10.81 | 0.001 * | −0.43 | |||||
| KIDSCREEN-ENFANT 2 | ||||||||||||||||||||||||
| Total index | 72.23 | 17.63 | 76.87 | −4.65 | 17.74 | 0.001 * | −0.26 | 67.39 | 17.7 | 73.82 | 17.26 | 72.66 | 17.89 | 0.213 | 76.78 | −4.12 | 17.92 | 0.064 | −0.23 | |||||
| KIDSCREEN-PARENTS 2 | ||||||||||||||||||||||||
| Total index | 69.61 | 14.83 | 71.84 | −2.23 | 14.83 | 0.046 * | −0.15 | 64.91 | 16.16 | 70.01 | 14.94 | 71.37 | 13.74 | 0.121 | 71.84 | −0.47 | 13.74 | 0.781 | −0.03 | |||||
2.5.1. Quality of Life Comparisons between the Neurobehavior Impairment Clusters
2.5.2. Quality of Life in Cluster 3
3. Current Insights
References
- Johnson, S.; Marlow, N. Preterm Birth and Childhood Psychiatric Disorders. Pediatr. Res. 2011, 69, 11R–18R.
- Anderson, P.J. Neuropsychological Outcomes of Children Born Very Preterm. Semin. Fetal Neonatal Med. 2014, 19, 90–96.
- Bolk, J.; Farooqi, A.; Hafström, M.; Åden, U.; Serenius, F. Developmental Coordination Disorder and Its Association with Developmental Comorbidities at 6.5 Years in Apparently Healthy Children Born Extremely Preterm. JAMA Pediatr. 2018, 172, 765–774.
- Bolk, J.; Fredriksson Kaul, Y.; Hellström-Westas, L.; Stjernqvist, K.; Padilla, N.; Serenius, F.; Hellgren, K.; Åden, U. National Population-Based Cohort Study Found that Visual-Motor Integration Was Commonly Affected in Extremely Preterm Born Children at Six-and-a-Half Years. Acta Paediatr. 2018, 107, 831–837.
- Mathewson, K.J.; Chow, C.H.T.; Dobson, K.G.; Pope, E.I.; Schmidt, L.A.; Van Lieshout, R.J. Mental Health of Extremely Low Birth Weight Survivors: A Systematic Review and Meta-Analysis. Psychol. Bull. 2017, 143, 347–383.
- Fitzallen, G.C.; Taylor, H.G.; Bora, S. What do We Know about the Preterm Behavioral Phenotype? A Narrative Review. Front. Psychiatry 2020, 11, 154.
- Korkman, M.; Mikkola, K.; Ritari, N.; Tommiska, V.; Salokorpi, T.; Haataja, L.; Tammela, O.; Pääkkönen, L.; Olsén, P.; Fellman, V. Neurocognitive Test Profiles of Extremely Low Birth Weight Five-Year-Old Children Differ according to Neuromotor Status. Dev. Neuropsychol. 2008, 33, 637–655.
- Heeren, T.; Joseph, R.M.; Allred, E.N.; O’Shea, T.M.; Leviton, A.; Kuban, K.C.K. Cognitive Functioning at the Age of 10 Years among Children Born Extremely Preterm: A Latent Profile Approach. Pediatr. Res. 2017, 82, 614–619.
- Pierrat, V.; Marchand-Martin, L.; Marret, S.; Arnaud, C.; Benhammou, V.; Cambonie, G.; Debillon, T.; Dufourg, M.-N.; Gire, C.; Goffinet, F.; et al. Neurodevelopmental Outcomes at Age 5 among Children Born Preterm: EPIPAGE-2 Cohort Study. BMJ 2021, 373, n741.
- Gire, C.; Resseguier, N.; Brévaut-Malaty, V.; Marret, S.; Cambonie, G.; Souksi-Medioni, I.; Müller, J.-B.; Garcia, P.; Berbis, J.; Tosello, B.; et al. Quality of Life of Extremely Preterm School-Age Children without Major Handicap: A Cross-Sectional Observational Study. Arch. Dis. Child. 2019, 104, 333–339.
- Gire, C.; Tosello, B.; Marret, S.; Cambonie, G.; Souksi-Medioni, I.; Müller, J.-B.; Garcia, P.; Berbis, J.; Auquier, P.; Brévaut-Malaty, V.; et al. Specific Cognitive Correlates of the Quality of Life of Extremely Preterm School-Aged Children without Major Neurodevelopmental Disability. Pediatr. Res. 2020, 88, 642–652.
- Johnson, S.; Wolke, D. Behavioural Outcomes and Psychopathology during Adolescence. Early Hum. Dev. 2013, 89, 199–207.
- Samuelsson, M.; Holsti, A.; Adamsson, M.; Serenius, F.; Hägglöf, B.; Farooqi, A. Behavioral Patterns in Adolescents Born at 23 to 25 Weeks of Gestation. Pediatrics 2017, 140, e20170199.
- Taylor, H.G.; Margevicius, S.; Schluchter, M.; Andreias, L.; Hack, M. Persisting Behavior Problems in Extremely Low Birth Weight Adolescents. J. Dev. Behav. Pediatr. 2015, 36, 178–187.
- Burnett, A.C.; Anderson, P.J.; Cheong, J.; Doyle, L.W.; Davey, C.G.; Wood, S.J. Prevalence of Psychiatric Diagnoses in Preterm and Full-Term Children, Adolescents and Young Adults: A Meta-Analysis. Psychol. Med. 2011, 41, 2463–2474.
- Burnett, A.C.; Youssef, G.; Anderson, P.J.; Duff, J.; Doyle, L.W.; Cheong, J.L.Y.; Victorian Infant Collaborative Study Group. Exploring the “Preterm Behavioral Phenotype” in Children Born Extremely Preterm. J. Dev. Behav. Pediatr. 2019, 40, 200–207.
- Korzeniewski, S.J.; Joseph, R.M.; Kim, S.H.; Allred, E.N.; O’Shea, T.M.; Leviton, A.; Kuban, K.C.K.; ELGAN Study Investigators. Social Responsiveness Scale Assessment of the Preterm Behavioral Phenotype in 10-Year-Olds Born Extremely Preterm. J. Dev. Behav. Pediatr. 2017, 38, 697–705.
- Mulder, H.; Pitchford, N.J.; Marlow, N. Processing Speed and Working Memory Underlie Academic Attainment in Very Preterm Children. Arch. Dis. Child. Fetal Neonatal Ed. 2010, 95, F267–F272.
- Aarnoudse-Moens, C.S.H.; Weisglas-Kuperus, N.; van Goudoever, J.B.; Oosterlaan, J. Meta-Analysis of Neurobehavioral Outcomes in Very Preterm and/or Very Low Birth Weight Children. Pediatrics 2009, 124, 717–728.
- Mulder, H.; Pitchford, N.J.; Marlow, N. Processing Speed Mediates Executive Function Difficulties in Very Preterm Children in Middle Childhood. J. Int. Neuropsychol. Soc. 2011, 17, 445–454.
- Omizzolo, C.; Scratch, S.E.; Stargatt, R.; Kidokoro, H.; Thompson, D.K.; Lee, K.J.; Cheong, J.; Neil, J.; Inder, T.E.; Doyle, L.W.; et al. Neonatal Brain Abnormalities and Memory and Learning Outcomes at 7 Years in Children Born Very Preterm. Memory 2014, 22, 605–615.
- Hutchinson, E.A.; De Luca, C.R.; Doyle, L.W.; Roberts, G.; Anderson, P.J.; Victorian Infant Collaborative Study Group. School-Age Outcomes of Extremely Preterm or Extremely Low Birth Weight Children. Pediatrics 2013, 131, e1053–e1061.
- Mulder, H.; Pitchford, N.J.; Hagger, M.S.; Marlow, N. Development of Executive Function and Attention in Preterm Children: A Systematic Review. Dev. Neuropsychol. 2009, 34, 393–421.
- Ritchie, K.; Bora, S.; Woodward, L.J. Social Development of Children Born Very Preterm: A Systematic Review. Dev. Med. Child Neurol. 2015, 57, 899–918.
- Conti, E.; Calderoni, S.; Marchi, V.; Muratori, F.; Cioni, G.; Guzzetta, A. The First 1000 Days of the Autistic Brain: A Systematic Review of Diffusion Imaging Studies. Front. Hum. Neurosci. 2015, 9, 159.
- Tymofiyeva, O.; Gano, D.; Trevino, R.J.; Glass, H.C.; Flynn, T.; Lundy, S.M.; McQuillen, P.S.; Ferriero, D.M.; Barkovich, A.J.; Xu, D. Aberrant Structural Brain Connectivity in Adolescents with Attentional Problems Who Were Born Prematurely. AJNR Am. J. Neuroradiol. 2018, 39, 2140–2147.





