
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Valeria Calcaterra | + 2005 word(s) | 2005 | 2021-10-26 04:41:36 | | | |
| 2 | Nora Tang | + 16 word(s) | 2021 | 2021-10-27 05:30:12 | | |
Video Upload Options
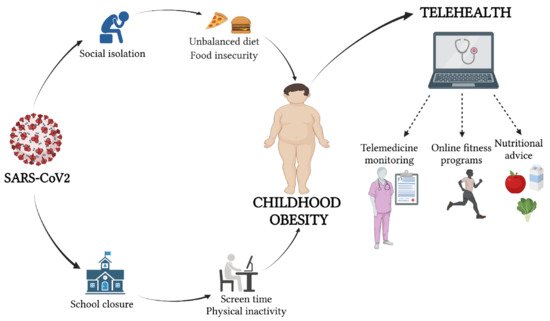
The COVID-19 pandemic has led to the implementation of policies that mandate various restrictions on daily life, including social distancing, the closure of public services and schools, and movement limitations. Even though these restrictive measures decreased the COVID-19 spread, they may have detrimental effects on various lifestyle components such as physical inactivity, sedentary behavior, and dietary habits, influencing the maintenance of weight and contributing to obesity among children and adolescents. The coexistence of childhood obesity and COVID-19 and changes in the bioecological environment have put children and adolescents at increased risk for developing obesity and exacerbating the severity of this disorder. The use of telehealth technology is a modern approach useful for the delivery of health care services by health care professionals, where distance is a critical factor. Telehealth is effective in promoting increased self-monitoring and behavioral change, and provides the opportunity to perform online nutritional support and exercise training programs to promote a healthy lifestyle and reduce sedentary behaviors in children and adolescents. Telehealth, including tele-exercise and tele-nutrition, has the potential to address many of the key challenges in providing health services, including in patients with obesity during the COVID-19 outbreak. This narrative review aims to describe the role of telehealth as an opportunity in the management of pediatric obesity in the COVID-19 era, and to deliver nutrition and exercise programs for the maintenance of health
1. Introduction
A global pandemic caused by the new coronavirus (COVID-19) has led to the implementation of policies that mandate various restrictions on daily life, including social distancing, the closure of public services and schools, and movement limitations [1]. Even though these restrictive measures decreased the COVID-19 spread, they may have detrimental effects on various lifestyle components and lead to physical inactivity, sedentary behaviors, and dietary habits, thereby influencing the maintenance of weight and contributing to obesity among children and adolescents [1][2][3]. Significant changes in dietary consumption patterns, frequency of meals, and skipping breakfast have been described [2][3]. Additionally, a decreased frequency of engaging in active transport, moderate or vigorous and high-intensity housework, physical activity (PA) during leisure time, and walking during leisure time, as well as increased sedentary, sleeping, and screen time, have been reported [4].
Telehealth is a set of services available to patients in specific geographic locations where the health care professional uses interactive audio and video telecommunication systems that permit asynchronous or real-time two-way communication between the patient and distant-site clinician [5]. The use of telehealth technology is a modern approach useful for the delivery of health care services by health care professionals where distance is a critical factor, using information and communication technologies (ICT) for the exchange of information [5]. As reported, telehealth and mobile health (mHealth) technologies are effective tools for obesity management [5].
Telehealth is effective in promoting increased self-monitoring, behavioral change, and weight reduction and it provides the opportunity to perform online nutritional support and exercise training programs to promote a healthy lifestyle and reduce sedentary behaviors in children and adolescents [6]. The WHO Regional Office for Europe has provided advice for health care providers on PA maintenance during isolation that includes the support of online resources [7].
Telehealth has the potential to address many of the key challenges in providing health services during the outbreak of COVID-19 in patients with obesity, too ( Figure 1 ).
2. Pediatric Obesity during the COVID-19 Era
Obesity and COVID-19 are pandemics that negatively affect the general health and well-being of children [8]. Firstly, childhood obesity is globally a major long-term public health [9] concern, which has dramatically increased over the past four decades, rising to pandemic levels in United States (U.S.) young people [8][10]. In 2020, the WHO has estimated the number of children under five years of age with overweight or obesity at 39 million [9]. In Italy, according to the latest “OKkio alla salute” report (2019), 20.4% of children are overweight and 9.4% are obese, and the prevalence of obesity is higher in southern regions than in the North [11]. Our country has the highest prevalence of obesity in all of Europe [11].
Obesity is a chronic disease influenced by genetic, environmental, and psychosocial factors [8]. Underlying the development of obesity is the breakdown of the body’s energy regulatory system (ERS). The most common cause of obesity in children is an excess of caloric intake in comparison with caloric expenditure, combined with a genetic predisposition. Childhood obesity is associated with various comorbidities involving multiple organs and systems, including type 2 diabetes mellitus, hypertension, nonalcoholic fatty liver disease, obstructive sleep apnea, and dyslipidemia [12].
An intervention with physical and nutrition education is needed to promote a healthy lifestyle among children with obesity during the COVID-19 pandemic, in order to mitigate its negative impact on unhealthy weight gain and childhood obesity [13].
Besides the well-known clinical burden, the COVID-19 pandemic has also resulted in socioeconomic changes that may have major repercussions for childhood obesity, especially among the poorest [14][15][16]. On that basis, a major study projected the impact of the COVID-19 pandemic on the prevalence of childhood obesity in the United States by proposing several scenarios that include school closures for several months and reductions in physical activity practiced by children and adolescents; both of these items, as has been observed, negatively affect the prevalence of obesity, mutually influencing each other so that the prevalence of obesity increases exponentially [13]. During COVID-19, job losses and layoffs increased, limiting financial resources [8]. At the same time, many communities saw significant increases in food costs [17]. According to the data collected, many households have predominantly purchased long-life, ultra-processed, high-calorie foods that are low-priced, highly palatable, and usable as a comfort item [18][19]. Higher-calorie foods can negatively impact all children, putting them at risk for weight gain [8].
3. Tele-Nutrition in Pediatric Obesity
The use of telemedicine even in urban areas has shown beneficial effects on obesity with evidence of stabilization or a decrease in BMI z-score. Families showed satisfaction and found their tele-visits to be more convenient than going to the main urban hospital. Although there was no control group for comparison, this study demonstrated the success of implementing telemedicine even in an urban environment [20].
The available evidence highlights the efficacy of these tools in improving weight loss, behavioral change, and drop-out rate [21][22][23][24][25]. On the other hand, the results from Davis et al. [26] should be interpreted carefully given the small sample size and lower frequency of counseling sessions compared with the clinical guideline recommendations. Patients and parents showed satisfaction with lifestyle changes, great enthusiasm about nutrition programs, and increased motivation [27][28]. This was reflected in increased adherence to family obesity treatment, particularly among the rural population, and in family involvement in nutrition programs [29][30].
During the current COVID-19 pandemic, both health care professionals and patients have been much more accepting of telehealth services, owing to the high risk of the spread of infection among patients and health care professionals at care sites, limited availability of adequate personal protective equipment (PPE), travel restrictions, limited access to hospitals, and interruption of most clinical activities.
In pediatric obesity, nutrition education for the whole family is the first treatment. Telemedicine visits are a great opportunity to get the whole family involved. Using a computer, tablet, or text messages, educational material can be shared and explained during the visit to encourage the patient and all stakeholders to be more active. Another potential benefit of telehealth nutrition care is that it increases access to medical nutrition therapy (MNT) by removing barriers related to limited finances, travel, time, and physical function, especially during COVID-19 [31].
4. Tele-Exercise in Pediatric Obesity
During the last two decades, thanks to the improvement of electronic devices and the spread of online technologies, training and exercise practice was implemented through applications, web channels, and online platforms and specific active videogames (called exergames) were also developed to bring exercise training closer to online technologies [32][33]. Before the COVID-19 pandemic, the use of tele-exercise and exergames as home training was high, especially among children with diseases, such as cerebral palsy, bone cancer, and cystic fibrosis, and aimed to limit public exposure, risk of infections, and transport barriers [34][35][36]. In a study conducted among children with cerebral palsy, during an online individualized training program, specialists deduced that virtual reality was effective in cognitive function improvement through levels of attention and increased concentration [34]. In addition, other studies in patients with spastic hemiplegic cerebral palsy showed an improvement in upper limb motor function and an increase in manual strength [37]. Chen et al. [35] proposed an interactive tele-exercise program with wearable devices in children with cystic fibrosis, suggesting that the streaming of sessions is a viable and convenient method to encourage PA practice without cross-infection risks associated with in-person group activity. Finally, Cosano et al. [36] reported benefits on bone health in pediatric cancer survivors through a supervised online training program.
In children with obesity, exergames have been proposed to reduce sedentary behaviors, improve sport participation, and reduce the risk of respiratory and cardiovascular diseases, generally as a tool to increase PA [38].
In children with type 1 diabetes, during the COVID-19 lockdown, Calcaterra et al. [39] proposed “CoVidentary”, an online exercise training program to reduce sedentary behaviors. The outcomes obtained by the exercise sessions showed that it is possible to reduce a sedentary lifestyle, but not to achieve the optimal level of recommended PA for children. In particular, this study concluded that a short duration training session developed through an online platform is more effective to encourage participation in a self- administrated exercise. Furthermore, a reduction in PA and exercise practice was shown in obese children, as well as augmented time spent on television and mobile phones. For these reasons, the tele-exercise and exergaming interventions could be important tools to reduce sedentary behavior and maintain an active lifestyle. Calcaterra et al. [40] proposed a different modality of exercise such as active breaks, playing with pets, balloon games, cleaning races, and music parties that could be performed at home and without specific equipment in safe conditions and without the risk of infections. Moreover, Staiano et al. [6] proposed the GameSquad intervention, a 24-week home-based exergaming intervention tailored for children and adolescents with obesity to investigate adherence, promote self-efficacy, and reduce perceived barriers. This study reported a reduction in BMI z-score and an improvement in cardiometabolic health (systolic and diastolic BP, total cholesterol, and LDL-cholesterol) among children with overweight and obesity. These results expand upon a home-based exergaming trial that effectively reduced BMI z-score and body fat over a 6-month period [41]. Furthermore, the GameSquad intervention obtained excellent adherence for children’s exergaming (94% over 24 weeks) by employing social support, including regular video chats with fitness coaches and a gaming curriculum and step tracker to motivate children’s PA. Telehealth directly involves the child in communicating, monitoring, and counselling on exercise.
To limit the spread of pediatric obesity, curricular sport and physical education in schools typically had a fundamental role and represents the largest and effective youth PA intervention worldwide [42]. Although regular in-person physical education programming is not without challenges [43], school closures due to COVID-19 created a new host of obstacles, especially in the obese population. In many countries, physical education shifted to virtual learning platforms [44], and physical education teachers and administrators were swiftly required to deliver robust virtual programs without adequate training and provision of appropriate teaching and learning resources. Online learning could produce bias, especially in youths owing to the unequal access to technology, adult supervision, and support, as well as lack of sports equipment and physical space to participate in online physical education [45]. Additional inequities are presented for youth with obesity who are particularly dependent on school physical education for PA engagement, and face barriers to being physically active in home environments [46]. Despite all these factors, if designed appropriately, online physical education may have the potential to reduce health disparities related to inequitable opportunities for PA engagement [47], reducing the distance between children with obesity and sport facilities, transport barriers, as well as the cost and the risk of contagiousness. For these reasons, tele-exercise surely needs further improvements, but becomes a valid tool in this unique period to help children with obesity to maintain an active lifestyle, participate in adapted activities, and share time and experience with their peers in a protective environment.
References
- Gontariuk, M.; Krafft, T.; Rehbock, C.; Townend, D.; Van der Auwermeulen, L.; Pilot, E. The European Union and Public Health Emergencies: Expert Opinions on the Management of the First Wave of the COVID-19 Pandemic and Suggestions for Future Emergencies. Front. Public Health 2021, 9, 698995.
- Tornaghi, M.; Lovecchio, N.; Vandoni, M.; Chirico, A.; Codella, R. Physical Activity Levels across COVID-19 Outbreak in Youngsters of Northwestern Lombardy. J. Sports Med. Phys. Fitness 2021, 61, 971–976.
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating Habits and Lifestyle Changes during COVID-19 Lockdown: An Italian Survey. J. Transl. Med. 2020, 18, 229.
- Vancini, R.L.; Andrade, M.S.; Viana, R.B.; Nikolaidis, P.T.; Knechtle, B.; Campanharo, C.R.V.; de Almeida, A.A.; Gentil, P.; de Lira, C.A.B. Physical Exercise and COVID-19 Pandemic in PubMed: Two Months of Dynamics and One Year of Original Scientific Production. Sports Med. Health Sci. 2021, 3, 80–92.
- WHO Global Observatory for eHealth Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on EHealth. Available online: https://apps.who.int/iris/handle/10665/44497 (accessed on 16 October 2021).
- Staiano, A.E.; Beyl, R.A.; Guan, W.; Hendrick, C.A.; Hsia, D.S.; Newton, R.L. Home-Based Exergaming among Children with Overweight and Obesity: A Randomized Clinical Trial. Pediatr Obes. 2018, 13, 724–733.
- Infection Prevention and Control during Health Care When Coronavirus Disease (COVID-19) Is Suspected or Confirmed. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-IPC-2021.1 (accessed on 16 October 2021).
- Browne, N.T.; Snethen, J.A.; Greenberg, C.S.; Frenn, M.; Kilanowski, J.F.; Gance-Cleveland, B.; Burke, P.J.; Lewandowski, L. When Pandemics Collide: The Impact of COVID-19 on Childhood Obesity. J. Pediatr. Nurs. 2021, 56, 90–98.
- The Lancet Public Health, null Childhood Obesity beyond COVID-19. Lancet Public Health 2021, 6, e534.
- Skinner, A.C.; Ravanbakht, S.N.; Skelton, J.A.; Perrin, E.M.; Armstrong, S.C. Prevalence of Obesity and Severe Obesity in US Children, 1999-2016. Pediatrics 2018, 141, e20173459.
- Lauria, L.; Spinelli, A.; Buoncristiano, M.; Nardone, P. Decline of Childhood Overweight and Obesity in Italy from 2008 to 2016: Results from 5 Rounds of the Population-Based Surveillance System. BMC Public Health 2019, 19, 618.
- Kumar, S.; Kelly, A.S. Review of Childhood Obesity: From Epidemiology, Etiology, and Comorbidities to Clinical Assessment and Treatment. Mayo Clin. Proc. 2017, 92, 251–265.
- An, R. Projecting the Impact of the Coronavirus Disease-2019 Pandemic on Childhood Obesity in the United States: A Microsimulation Model. J. Sport Health Sci. 2020, 9, 302–312.
- Nogueira-de-Almeida, C.A.; Del Ciampo, L.A.; Ferraz, I.S.; Del Ciampo, I.R.L.; Contini, A.A.; Ued, F.d.V. COVID-19 and Obesity in Childhood and Adolescence: A Clinical Review. J. Pediatr. 2020, 96, 546–558.
- Woo Baidal, J.A.; Chang, J.; Hulse, E.; Turetsky, R.; Parkinson, K.; Rausch, J.C. Zooming Toward a Telehealth Solution for Vulnerable Children with Obesity During Coronavirus Disease 2019. Obesity 2020, 28, 1184–1186.
- Dooley, D.G.; Bandealy, A.; Tschudy, M.M. Low-Income Children and Coronavirus Disease 2019 (COVID-19) in the US. JAMA Pediatr. 2020, 174, 922–923.
- Fore, H.H. A Wake-up Call: COVID-19 and Its Impact on Children’s Health and Wellbeing. Lancet Glob. Health 2020, 8, e861–e862.
- Almandoz, J.P.; Xie, L.; Schellinger, J.N.; Mathew, M.S.; Gazda, C.; Ofori, A.; Kukreja, S.; Messiah, S.E. Impact of COVID-19 Stay-at-Home Orders on Weight-Related Behaviours among Patients with Obesity. Clin. Obes. 2020, 10, e12386.
- Rundle, A.G.; Park, Y.; Herbstman, J.B.; Kinsey, E.W.; Wang, Y.C. COVID-19-Related School Closings and Risk of Weight Gain Among Children. Obesity 2020, 28, 1008–1009.
- Slusser, W.; Whitley, M.; Izadpanah, N.; Kim, S.L.; Ponturo, D. Multidisciplinary Pediatric Obesity Clinic via Telemedicine Within the Los Angeles Metropolitan Area: Lessons Learned. Clin. Pediatr. 2016, 55, 251–259.
- Rhodes, E.T.; Vernacchio, L.; Mitchell, A.A.; Fischer, C.; Giacalone, P.; Ludwig, D.S.; Ebbeling, C.B. A Telephone Intervention to Achieve Differentiation in Dietary Intake: A Randomized Trial in Paediatric Primary Care. Pediatr. Obes. 2017, 12, 494–501.
- Shaikh, U.; Nettiksimmons, J.; Romano, P. Pediatric Obesity Management in Rural Clinics in California and the Role of Telehealth in Distance Education. J. Rural. Health 2011, 27, 263–269.
- Johansson, L.; Hagman, E.; Danielsson, P. A Novel Interactive Mobile Health Support System for Pediatric Obesity Treatment: A Randomized Controlled Feasibility Trial. BMC Pediatr. 2020, 20, 447.
- Vidmar, A.P.; Pretlow, R.; Borzutzky, C.; Wee, C.P.; Fox, D.S.; Fink, C.; Mittelman, S.D. An Addiction Model-Based Mobile Health Weight Loss Intervention in Adolescents with Obesity. Pediatr. Obes. 2019, 14, e12464.
- Sharifi, M.; Dryden, E.M.; Horan, C.M.; Price, S.; Marshall, R.; Hacker, K.; Finkelstein, J.A.; Taveras, E.M. Leveraging Text Messaging and Mobile Technology to Support Pediatric Obesity-Related Behavior Change: A Qualitative Study Using Parent Focus Groups and Interviews. J. Med. Internet Res. 2013, 15, e272.
- Davis, A.M.; James, R.L.; Boles, R.E.; Goetz, J.R.; Belmont, J.; Malone, B. The Use of TeleMedicine in the Treatment of Paediatric Obesity: Feasibility and Acceptability. Matern Child Nutr. 2011, 7, 71–79.
- Fleischman, A.; Hourigan, S.E.; Lyon, H.N.; Landry, M.G.; Reynolds, J.; Steltz, S.K.; Robinson, L.; Keating, S.; Feldman, H.A.; Antonelli, R.C.; et al. Creating an Integrated Care Model for Childhood Obesity: A Randomized Pilot Study Utilizing Telehealth in a Community Primary Care Setting. Clin. Obes. 2016, 6, 380–388.
- Siegel, R.M.; Haemer, M.; Kharofa, R.Y.; Christison, A.L.; Hampl, S.E.; Tinajero-Deck, L.; Lockhart, M.K.; Reich, S.; Pont, S.J.; Stratbucker, W.; et al. Community Healthcare and Technology to Enhance Communication in Pediatric Obesity Care. Child Obes. 2018, 14, 453–460.
- Walters, J.; Johnson, T.; DeBlasio, D.; Klein, M.; Sikora, K.; Reilly, K.; Hutzel-Dunham, E.; White, C.; Xu, Y.; Burkhardt, M.C. Integration and Impact of Telemedicine in Underserved Pediatric Primary Care. Clin. Pediatr. 2021, 60, 452–458.
- Smith, A.J.; Skow, Á.; Bodurtha, J.; Kinra, S. Health Information Technology in Screening and Treatment of Child Obesity: A Systematic Review. Pediatrics 2013, 131, e894–e902.
- Cueto, V.; Sanders, L.M. Telehealth Opportunities and Challenges for Managing Pediatric Obesity. Pediatr. Clin. N. Am. 2020, 67, 647–654.
- Stella, A.B.; Ajčević, M.; Furlanis, G.; Cillotto, T.; Menichelli, A.; Accardo, A.; Manganotti, P. Smart Technology for Physical Activity and Health Assessment during COVID-19 Lockdown. J. Sports Med. Phys. Fit. 2021, 61, 9.
- Liang, Y.; Lau, P.W.C.; Jiang, Y.; Maddison, R. Getting Active with Active Video Games: A Quasi-Experimental Study. Int. J. Environ. Res. Public Health 2020, 17, 7984.
- Johnson, R.W.; Williams, S.A.; Gucciardi, D.F.; Bear, N.; Gibson, N. Evaluating the Effectiveness of Home Exercise Programmes Using an Online Exercise Prescription Tool in Children with Cerebral Palsy: Protocol for a Randomised Controlled Trial. BMJ Open 2018, 8, e018316.
- Gil-Cosano, J.J.; Ubago-Guisado, E.; Sánchez, M.J.; Ortega-Acosta, M.J.; Mateos, M.E.; Benito-Bernal, A.I.; Llorente-Cantarero, F.J.; Ortega, F.B.; Ruiz, J.R.; Labayen, I.; et al. The Effect of an Online Exercise Programme on Bone Health in Paediatric Cancer Survivors (IBoneFIT): Study Protocol of a Multi-Centre Randomized Controlled Trial. BMC Public Health 2020, 20, 1520.
- Chen, J.J. Tele-Exercise as a Promising Tool to Promote Exercise in Children With Cystic Fibrosis. Front. Public Health 2018, 6, 5.
- Johnson, R.W.; Williams, S.A.; Gucciardi, D.F.; Bear, N.; Gibson, N. Can an Online Exercise Prescription Tool Improve Adherence to Home Exercise Programmes in Children with Cerebral Palsy and Other Neurodevelopmental Disabilities? A Randomised Controlled Trial. Randomized Control. Trial 2020, 10, e040108.
- Chen, H.; Sun, H. Effects of Active Videogame and Sports, Play, and Active Recreation for Kids Physical Education on Children’s Health-Related Fitness and Enjoyment. Games Health J. 2017, 6, 312–318.
- Calcaterra, V.; Iafusco, D.; Pellino, V.C.; Mameli, C.; Tornese, G.; Chianese, A.; Cascella, C.; Macedoni, M.; Redaelli, F.; Zuccotti, G.; et al. “CoVidentary”: An Online Exercise Training Program to Reduce Sedentary Behaviours in Children with Type 1 Diabetes during the COVID-19 Pandemic. J. Clin. Transl. Endocrinol. 2021, 25, 100261.
- Calcaterra, V.; Vandoni, M.; Pellino, V.C.; Cena, H. Special Attention to Diet and Physical Activity in Children and Adolescents With Obesity During the Coronavirus Disease-2019 Pandemic. Front. Pediatr. 2020, 8, 407.
- Maddison, R.; Foley, L.; Ni Mhurchu, C.; Jiang, Y.; Jull, A.; Prapavessis, H.; Hohepa, M.; Rodgers, A. Effects of Active Video Games on Body Composition: A Randomized Controlled Trial. Am. J. Clin. Nutr. 2011, 94, 156–163.
- D’Agostino, E.M.; Urtel, M.; Webster, C.A.; McMullen, J.; Culp, B. Virtual Physical Education During COVID-19: Exploring Future Directions for Equitable Online Learning Tools. Front. Sports Act. Living 2021, 3, 716566.
- Hardman, K. Physical Education in Schools: A Global Perspective. Kinesiology 2008, 40, 5–28.
- Webster, C.; D’Agostino, E.; Urtel, M.; Mcmullen, J.; Culp, B.; Loiacono, C.; Killian, C. Physical Education in the COVID Era: Considerations for Online Program Delivery Using the Comprehensive School Physical Activity Program Framework. J. Teach. Phys. Educ. 2021, 40, 327–336.
- Daum, D.N. Thinking about Hybrid or Online Learning in Physical Education? Start Here! Null 2020, 91, 42–44.
- Esentürk, O. Parents’ Perceptions on Physical Activity for Their Children with Autism Spectrum Disorders during the Novel Coronavirus Outbreak. Int. J. Dev. Disabil. 2020, 1–12.
- Draper, C.E.; Milton, K.; Schipperijn, J. COVID-19 and Physical Activity: How Can We Build Back Better? J. Phys. Act. Health 2021, 18, 149–150.




