
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Iole Vozza | + 1749 word(s) | 1749 | 2021-09-13 08:09:39 |
Video Upload Options
Cleft lip and palate (CLP) are craniofacial dysmorphisms that fall within the anomalies of the developmental jaws as they are congenital malformations characterized by the arrested development of the homonymous regions of the maxillofacial district. Orofacial clefts occur due to failure of migration or fusion in the embryonic period of intrauterine life; craniofacial skeletal structures, hard and soft tissues of the oral cavity are particularly involved. The cause of cleft lip and/or palate (CLP) is thought to be multifactorial, namely through genetic or environmental factors.
1. Introduction
In literature, recent studies express consensus about the prevalence at birth of CLP, which on average is around 1 over 500 live births in eastern countries and decreases to 1 over 1000 live births in western countries [1][2][3][4][5][6][7].
1.1. Cleft Lip and Palate-Related Orodental Issues in the Pediatric Age
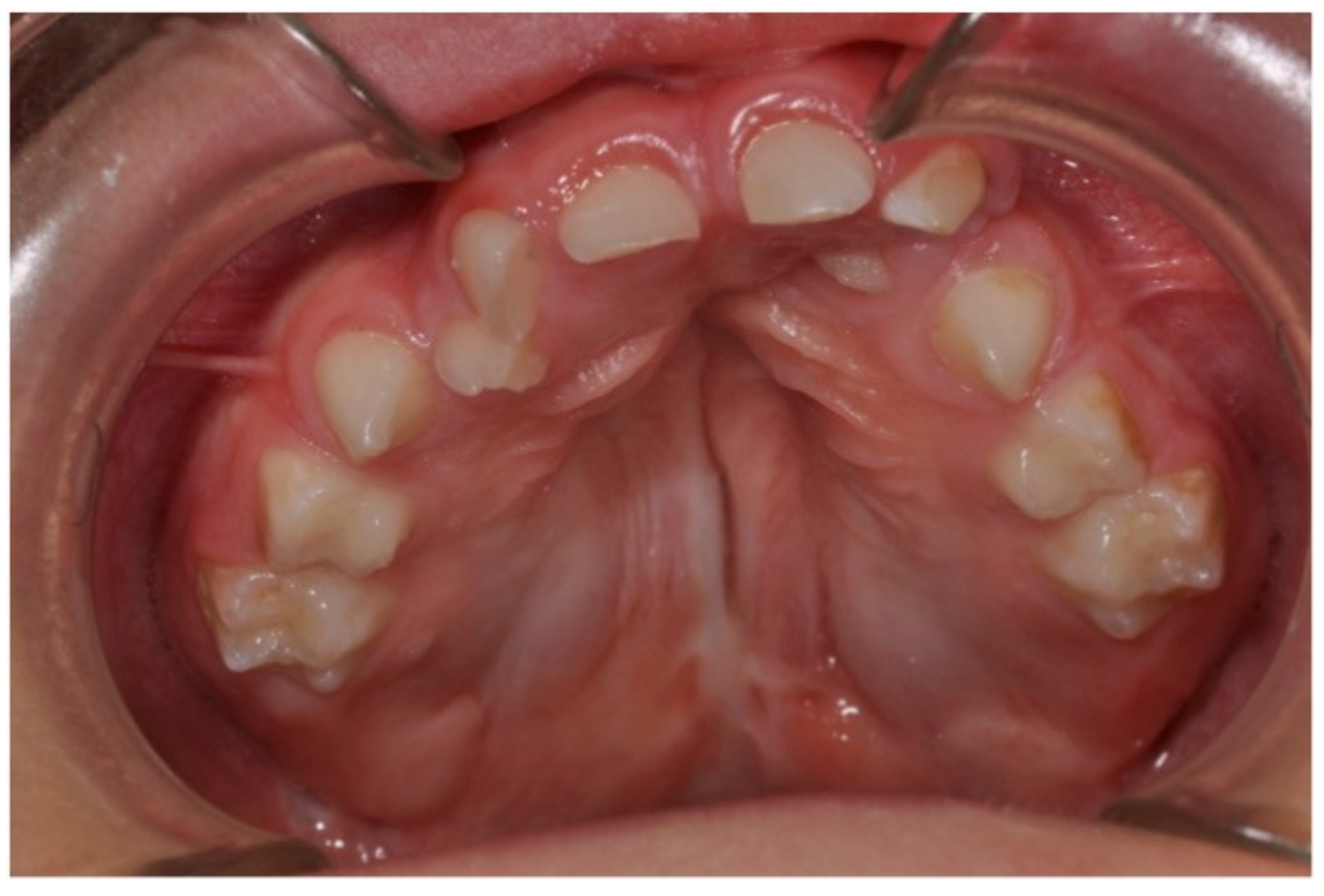
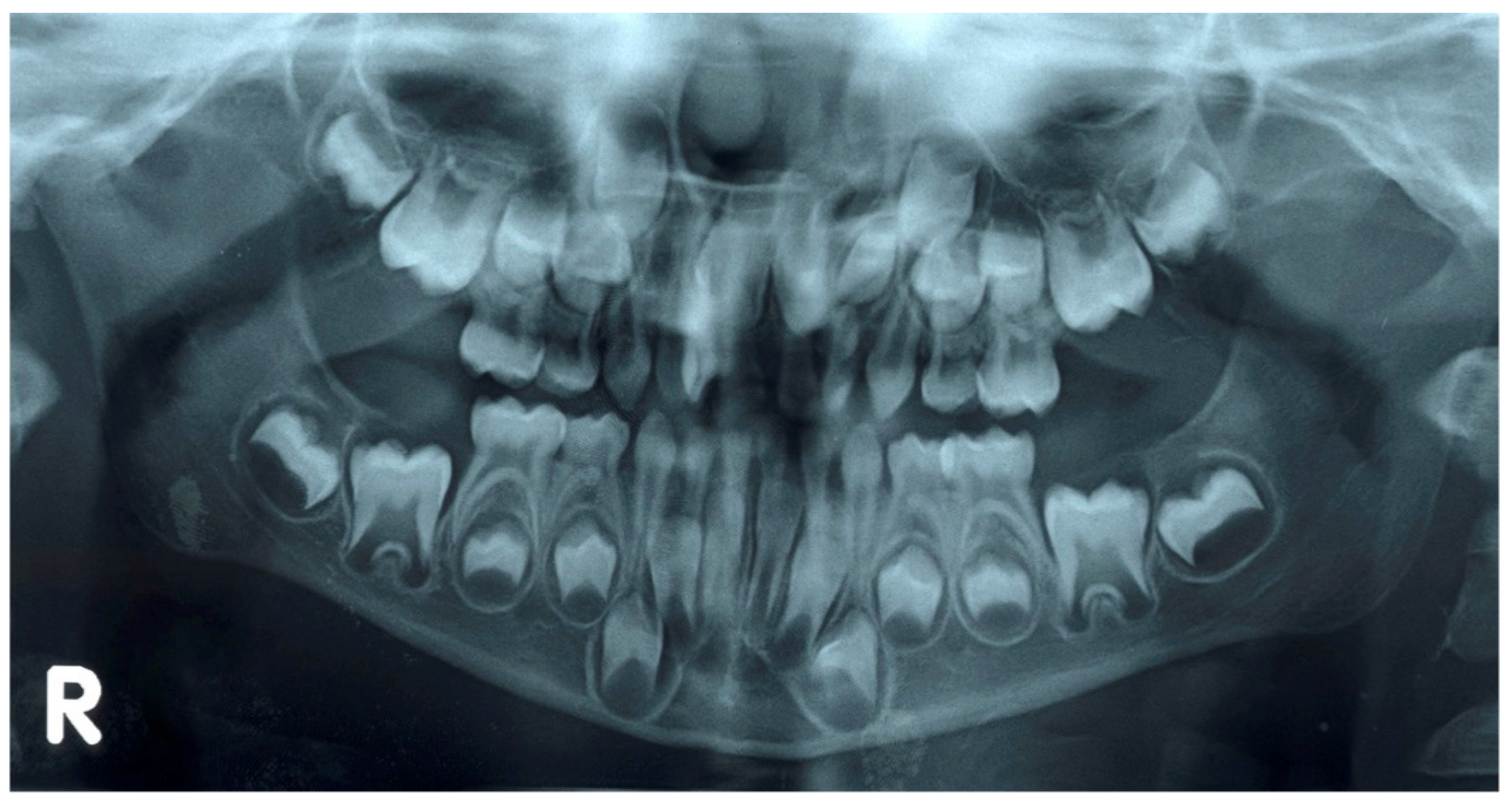
Oral problems occurring in the pediatric age in subjects affected by cleft lip and palate are characterized by both dental anomalies and oral health problems. The latter are linked not only to oral anomalies, but also to the presence of cicatricial results from early maxillary orthopedics and surgery which interfere with adequate oral hygiene maneuvers and consequentially increase the risk of tooth decay and gingivitis [8][9]. The several orodental problems that might affect pediatric CLP patients are: anomalies of number (excess and defect), anomalies of shape, anomalies of volume, anomalies of seat, anomalies of structure, eruption anomalies, maxillary bones growth deficit, poor oral hygiene and related risk of gingivitis and dental caries [10][11].
Recent epidemiological studies aimed at evaluating the prevalence of pediatric dentistry problems associated with CLP. A very recent case-control study [12] was conducted on Columbian pediatric patients with non-syndromic CLP aged between 5 and 12 years. The sample consisted of 210 CLP subjects and 210 healthy subjects. Only dental anomalies affecting permanent teeth were considered. CLP patients presented a significantly greater risk (p < 0.0001) of developing agenesis of the maxillary lateral incisors, supernumerary teeth, microdontia of the maxillary lateral incisors, and rotation of the maxillary central incisor adjacent to the cleft. Most anomalies were located in the cleft area. In particular, the highest prevalence was found for the microdontia of the lateral maxillary incisors, followed by rotations of the central maxillary incisors, agenesis of the lateral maxillary incisors, and supernumerary teeth.
A Japanese longitudinal study from 2017 [11] studied a large sample of CLP patients in the period from 1970 to 2009 with the aim of collecting data on dental anomalies. The study examined the medical records of 1724 CLP subjects, distributed in different phases of dentition, assessing the presence of dental anomalies in association to the single dental element, to the type of cleft, to the gender, and to the location of the anomaly in relation to the skeletal area of the cleft. In relation to hypodontia of the maxillary arch, the study found that the most affected dental elements were the lateral incisors, both primary and permanent, and the second permanent premolar. The overall prevalence of hypodontia was 16.2% in primary dentition and 52.7% in permanent dentition. In both cases, the prevalence increased with the severity and extension of the defect and therefore of the cleft. Furthermore, in primary dentition, the prevalence was higher on the cleft side than on the contralateral side. In both dentitions, there were no differences between males and females and between the right and left sides. Microdontia mainly affected the permanent maxillary lateral incisors. Dental fusions were more frequent in primary than in permanent dentition and the main affected teeth were the primary upper central and lateral incisors, the corresponding lower central and lateral incisors, and the primary lower canines. The prevalence of supernumeraries was 17.7% in primary dentition and 5.7% in permanent dentition. The maxillary lateral incisors were mainly affected [11].
1.2. Multidisciplinary Approach in the Management of CLP Patients
2. The Role of the Pediatric Dentist in the Multidisciplinary Management of the Cleft Lip Palate Patient



3. Conclusions
The management of CLP patients in pediatric dentistry must always be based on the choice of therapeutic solutions related to the level of severity of the risk and on the recognition of the determining role of the compliance of the little patient.
The role of the pediatric dentist in pediatric dental care for the patient with a cleft lip and palate extends from birth through to adolescence and young adulthood and also plays a vital role in CLP multispecialty team. Apart from this, the pediatric dentist can also play a crucial role in communicating with the rest of the team. For the parents of babies with a cleft, the stages of cleft surgery are major landmarks: the dentist needs to understand the surgical procedures and their timing so that dental care can be integrated sensitively within the overall treatment plan. Two-way communication helps to achieve the most effective treatment plan for the individual.
References
- Yang, Y.; Liu, H.; Ma, R.; Jin, L. Prevalence of Cleft Lip/Palate in the Fangshan District of Beijing, 2006–2012. Cleft Palate Craniofacial J. 2018, 55, 1296–1301.
- Chincharadze, S.; Vadachkoria, Z.; Mchedlishvili, I. Prevalence of cleft lip and palate in Georgia. Georgian Med. News 2017, 262, 24–28.
- Impellizzeri, A.; Giannantoni, I.; Polimeni, A.; Barbato, E.; Galluccio, G. Epidemiological characteristic of Orofacial clefts and its associated congenital anomalies: Retrospective study. BMC Oral Health 2019, 19, 290.
- Alonso, R.R.H.; Brigetty, G.P.S. Analysis of the Prevalence and Incidence of Cleft Lip and Palate in Colombia. Cleft Palate Craniofacial J. 2019, 57, 552–559.
- Elahi, M.M.; Jackson, I.T.; Elahi, O.; Khan, A.H.; Mubarak, F.; Tariq, G.B.; Mitra, A. Epidemiology of cleft lip and cleft palate in Pakistan. Plast. Reconstr. Surg. 2004, 113, 1548–1555.
- Hlongwa, P.; Levin, J.; Rispel, L.C. Epidemiology and clinical profile of individuals with cleft lip and palate utilising specialised academic treatment centres in South Africa. PLoS ONE 2019, 14, e0215931.
- Imai, Y.; Sanada, T.; Tachi, M. The Birth Prevalence of Cleft Lip and/or Cleft Palate After the 2011 Tōhoku Earthquake and Tsunami. Cleft Palate Craniofacial J. 2019, 56, 1133–1138.
- Van Dyck, J.; de Llano-Perula, M.C.; Willems, G.; Verdonck, A. Dental development in cleft lip and palate patients: A systematic review. Forensic Sci. Int. 2019, 300, 63–74.
- Luzzi, V.; Ierardo, G.; Corridore, D.; Di Carlo, G.; Di Giorgio, G.; Leonardi, E.; Campus, G.G.; Vozza, I.; Polimeni, A.; Bossù, M. Evaluation of the orthodontic treatment need in a paediatric sample from Southern Italy and its importance among paediatricians for improving oral health in pediatric dentistry. J. Clin. Exp. Dent. 2017, 9, e995–e1001.
- Freitas, J.A.; Garib, D.G.; Oliveira, M.; Lauris Rde, C.; Almeida, A.L.; Neves, L.T.; Trindade-Suedam, I.K.; Yaedú, R.Y.; Soares, S.; Pinto, J.H. Rehabilitative treatment of cleft lip and palate: Experience of the Hospital for Rehabilitation of Craniofacial Anomalies-USP (HRAC-USP)—Part 2: Pediatric dentistry and orthodontics. J. Appl. Oral Sci. 2012, 20, 268–281.
- Suzuki, A.; Nakano, M.; Yoshizaki, K.; Yasunaga, A.; Haruyama, N.; Takahashi, I. A Longitudinal Study of the Presence of Dental Anomalies in the Primary and Permanent Dentitions of Cleft Lip and/or Palate Patients. Cleft Palate Craniofacial J. 2017, 54, 309–320.
- Yezioro-Rubinsky, S.; Eslava-Schmalbach, J.H.; Otero, L.; Rodriguez-Aguirre, S.A.; Duque, A.M.; Campos, F.M.; Gomez, J.P.; Gomez-Arango, S.; Posso-Moreno, S.L.; Rojas, N.E.; et al. Dental Anomalies in Permanent Teeth Associated With Nonsyndromic Cleft Lip and Palate in a Group of Colombian Children. Cleft Palate Craniofacial J. 2020, 57, 73–79.
- Rodrigues, R.; Fernandes, M.H.; Bessa Monteiro, A.; Furfuro, R.; Carvalho Silva, C.; Vardasca, R.; Mendes, J.; Manso, M.C. Are there any solutions for improving the cleft area hygiene in patients with cleft lip and palate? A systematic review. Int. J. Dent. Hyg. 2019, 17, 130–141.
- Veiga, K.A.; Porto, A.N.; Matos, F.Z.; de Brito, P.C.B.; Borges, A.H.; Volpato, L.E.R.; Aranha, A.M.F. Caries Experience and Periodontal Status in Children and Adolescents with Cleft Lip and Palate. Pediatric Dent. 2017, 39, 139–144.
- Nirmala, S.V.S.G.; Saikrishna, D. Dental concerns of children with cleft lip and palate—A review. J. Pediatric Neonatal Care 2018, 8, 172–178.
- Udin, R.D. The pediatric dentist and the craniofacial anomalies team. Ear Nose Throat J. 1986, 65, 305–310.




