
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Artur Stolarczyk | + 1689 word(s) | 1689 | 2021-08-17 10:08:22 | | | |
| 2 | Enzi Gong | Meta information modification | 1689 | 2021-08-24 02:42:29 | | |
Video Upload Options
Osteoarthritis (OA) affects one in three people over the age of 65, and it is more common among women than men. This multifactorial disease leads to structural changes of the joint, and it is connected to chronic conditions. OA is characterized by pain, stiffness, and decreased range of motion (ROM). These factors lead to poor quality of life—insomnia, depression, lack of confidence, and limitations in daily activities, work, or hobbies. OA causes very serious problems for patients and significant social and economic costs.
1. Overview
Worldwide tendencies to perform large numbers of total hip arthroplasties in the treatment of osteoarthritis are observable over a long period of time. Every year, there is an observable increase in the number of these procedures performed. The outcomes are good but not ideal, especially in groups of patients with spine problems. In recent years, a growing interest in this field may be observed, since spinopelvic alignment seems to have a significant impact on total hip replacement (THR) results. The aim of this study is to describe relations between spine and pelvic alignment and provide practical information about its impact on total hip replacement. The authors performed a literature review based on PubMed, Embase, and Medline and provide practical guidelines based on them and their own experience.
2. Osteoarthritis
3. What May Influence the Spinopelvic Alignment?
4. Problems Associated with Improper Spinopelvic Mobility and THR
5. Anatomy and Imaging
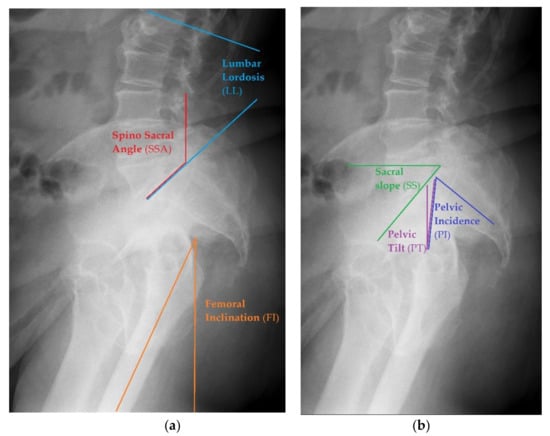
Radiographic Measurements
-
Pelvic Tilt (PT)—an angle between the reference vertical line and the line joining the middle of S1 upper endplate and the center of the femoral head. The normal value ranges from 7 to 19° [31].
-
Pelvic Incidence (PI)— the angle between the line that is formed by connecting the upper endplate of S1 (at its midpoint) to the femoral head axis. The normal value ranges from 38 to 56° [31].
-
Pelvic Femoral Angle (PFA)—the position of the femur in relation to the pelvis. It is the angle centered at the femoral head, between the mid sacral base and down femoral shaft. The normal value ranges from 1 to 17° [31].
-
Lumbar Lordosis (LL)—the segmental angle of spinal segment in lordosis, measured between the line on the upper endplate of L1 and the line on the upper endplate of S1(L1 -L5). The normal value ranges from 40 to 58° [31].
-
Femoral Inclination (FI)—the angle between a vertical reference line and the axis of the femur. The normal value ranges from 0 to 8° [31].
-
Sacro Femoral Angle (SFA)—the angle between the line of the upper endplate of S1 and the axis of the femur. The normal value ranges from 43 to 61° [31]
-
Spino Sacral Angle (SSA)—the angle between the line of the upper endplate of S1 and a reference vertical line. The normal value ranges from 119 to 133° [31].
References
- Wareńczak, A.; Lisiński, P. Does total hip replacement impact on postural stability? BMC Musculoskelet. Disord. 2019, 20, 229.
- Tsinaslanidis, G.; Tsinaslanidis, P.; Mahajan, R.H. Perioperative Pain Management in Patients Undergoing Total Hip Arthroplasty: Where Do We Currently Stand? Cureus 2020, 12, e9049.
- Law, W.A. Post-operative study of vitallium mould arthroplasty of the hip. J. Bone Jt. Surg Br. 1948, 30, 76–83.
- Learmonth, I.D.; Young, C.; Rorabeck, C. The operation of the century: Total hip replacement. Lancet 2007, 370, 1508–1519.
- Kase, M.; O’Loughlin, P.F.; Aït-Si-Selmi, T.; Pagenstert, G.; Langlois, J.; Bothorel, H.; Bonnin, M.P. Pre-operative templating in THA. Part I: A classification of architectural hip deformities. Arch. Orthop. Trauma Surg. 2019, 140, 129–137.
- Wainwright, T.W.; Gill, M.; McDonald, D.A.; Middleton, R.G.; Reed, M.; Sahota, O.; Yates, P.; Ljungqvist, O. Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Acta Orthop. 2020, 91, 3–19.
- Darrith, B.; Courtney, P.M.; Della Valle, C.J. Outcomes of dual mobility components in total hip arthroplasty. Bone Jt. J. 2018, 100-B, 11–19.
- Mohanty, S.S.; Mohan, H.; Rathod, T.N.; Kamble, P. Patient satisfaction related outcome after total hip arthroplasty; does bearing surface play a role? J. Clin. Orthop. Trauma 2020, 11 (Suppl. 2), S196–S200.
- Bourne, R.B.; Chesworth, B.; Davis, A.; Mahomed, N.; Charron, K. Comparing Patient Outcomes After THA and TKA: Is There a Difference? Clin. Orthop. Relat. Res. 2009, 468, 542–546.
- Tang, H.; Du, H.; Tang, Q.; Yang, D.; Shao, H.; Zhou, Y. Chinese patients’ satisfaction with total hip arthroplasty: What is important and dissatisfactory? J. Arthroplast. 2014, 29, 2245–2250.
- Glassman, A.H. Preoperative planning for primarytotal hip arthroplasty. Oper. Tech. Orthop. 1995, 5, 296–305.
- Shemesh, S.S.; Robinson, J.; Keswani, A.; Bronson, M.J.; Moucha, C.S.; Chen, D. The Accuracy of Digital Templating for Primary Total Hip Arthroplasty: Is There a Difference Between Direct Anterior and Posterior Approaches? J. Arthroplast. 2017, 32, 1884–1889.
- Liebs, T.; Nasser, L.; Herzberg, W.; Ruther, W.; Hassenpflug, J. The influence of femoral offset on health-related quality of life after total hip replacement. Bone Jt. J. 2014, 96, 36–42.
- Rondon, A.; Sariali, E.; Vallet, Q.; Grimal, Q. Modal analysis for the assessment of cementless hip stem primary stability in preoperative THA planning. Med. Eng. Phys. 2017, 49, 79–88.
- Lazennec, J.-Y.; Brusson, A.; Rousseau, M.-A. Hip–spine relations and sagittal balance clinical consequences. Eur. Spine J. 2011, 20, 686–698.
- Lewinnek, G.E.; Lewis, J.L.; Tarr, R.; Compere, C.L.; Zimmerman, J.R. Dislocations after total hip-replacement arthroplasties. J. Bone Jt. Surg Am. 1978, 60, 120–217.
- Barrey, C.; Roussouly, P.; Le Huec, J.-C.; D’Acunzi, G.; Perrin, G. Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur. Spine J. 2013, 22, S834–S841.
- Lee, S.H.; Lim, C.W.; Choi, K.Y.; Jo, S. Effect of Spine-Pelvis Relationship in Total Hip Arthroplasty. Hip Pelvis 2019, 31, 4–10.
- Barrey, C.; Jund, J.; Noseda, O.; Roussouly, P. Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur. Spine J. 2007, 16, 1459–1467.
- Pizones, J.; García-Rey, E. Pelvic motion the key to understanding spine–hip interaction. EFORT Open Rev. 2020, 5, 522–533.
- Dargel, J.; Oppermann, J.; Brüggemann, G.-P.; Eysel, P. Dislocation Following Total Hip Replacement. Dtsch. Aerzteblatt Online 2014, 111, 884–890.
- Fackler, C.D.; Poss, R. Dislocation in total hip arthroplasties. Clin. Orthop. Relat. Res. 1980, 151, 169–178.
- Paterno, S.A.; Lachiewicz, P.F.; Kelley, S.S. The influence of patient-related factors and position of the acetabular component on the rate of dislocation after total hip replacement. J. Bone Jt. Surg. 1997, 79, 1202.
- Khatod, M.; Barber, T.; Paxton, E.; Namba, R.; Fithian, D. An Analysis of the Risk of Hip Dislocation with a Contemporary Total Joint Registry. Clin. Orthop. Relat. Res. 2006, 447, 19–23.
- Masonis, J.L.; Bourne, R.B. Surgical Approach, Abductor Function, and Total Hip Arthroplasty Dislocation. Clin. Orthop. Relat. Res. 2002, 405, 46–53.
- Howie, D.W.; Holubowycz, O.T.; Middleton, R. Large femoral heads decrease the incidence of dislocation after total hip arthroplasty: A randomized controlled trial. J. Bone Jt. Surg. 2012, 94, 1095–1102.
- Abdel, M.P.; von Roth, P.; Jennings, M.T.; Hanssen, A.D.; Pagnano, M.W. What Safe Zone? The Vast Majority of Dislocated THAs Are Within the Lewinnek Safe Zone for Acetabular Component Position. Clin. Orthop. Relat. Res. 2016, 474, 386–391.
- DelSole, E.M.; Vigdorchik, J.; Schwarzkopf, R.; Errico, T.; Buckland, A. Total Hip Arthroplasty in the Spinal Deformity Population: Does Degree of Sagittal Deformity Affect Rates of Safe Zone Placement, Instability, or Revision? J. Arthroplast. 2017, 32, 1910–1917.
- Roussouly, P.; Nnadi, C. Sagittal plane deformity: An overview of interpretation and management. Eur. Spine J. 2010, 19, 1824–1836.
- Imai, N.; Suzuki, H.; Sakagami, A.; Hirano, Y.; Endo, N. Correlation of the anatomical sacral slope with pelvic incidence in female patients with developmental hip dysplasia: A retrospective cross-sectional study. J. Orthop. Surg. Res. 2020, 15, 1–6.
- Wang, W.J.; Liu, F.; Zhu, Y.; Sun, M.; Qiu, Y.; Weng, W.J. Sagittal alignment of the spine-pelvis-lower extremity axis in patients with severe knee osteoarthritis. Bone Jt. Res. 2016, 5, 198–205.
- Suzuki, H.; Endo, K.; Sawaji, Y.; Matsuoka, Y.; Nishimura, H.; Takamatsu, T.; Murata, K.; Seki, T.; Konishi, T.; Aihara, T.; et al. Radiographic Assessment of Spinopelvic Sagittal Alignment from Sitting to Standing Position. Spine Surg. Relat. Res. 2018, 2, 290–293.




