
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Paolo Visconti | + 1615 word(s) | 1615 | 2021-08-13 11:05:40 | | | |
| 2 | Catherine Yang | -3 word(s) | 1612 | 2021-08-13 11:48:11 | | |
Video Upload Options
Wearable devices are powerful tools for supporting IoT systems because of their sensing, processing, and communication capability. The term wearable devices cover a wide range of products integrated into clothing and accessories worn by the user and constantly connected to other intelligent electronic systems and the Internet network, allowing the detection, storage, and exchange of data in real-time and without human intervention. Particularly, they allow detection of patients’ vital parameters (e.g., heart rate (HR), oxygen saturation- (SpO2), body temperature, blood pressure (BP), etc.)
1. Introduction
The rapid evolution of technology in recent decades has led to availability in the market of ICT (Information and Communications Technology) devices that feature increasingly cutting-edge performance, allowing for a significant improvement in daily activities [1][2][3]. Due to the COVID-19 emergency, a further boost occurred in the digitization process, encouraging the collaboration between medicine and technology to implement increasingly accurate health services and allowing a significant technological development in the health sector and the culture of prevention [4][5][6]. In this area, interest has grown to design new devices and systems constantly available and wearable, thanks to new solutions increasingly comfortable and smaller [7]. Internet of Medical Things (IoMT) platforms are revolutionizing the health systems, opening new frontiers in home medical care, allowing integrated, capillary, and precise monitoring of the patients’ conditions, reduction of management costs, better diagnosis, earlier prevention, continuous tracking, and more rapid intervention [8][9][10]. These platforms aim to provide a secure connection to source devices for collecting data, processing them to extract helpful information, and securely storing them. Several technologies can be exploited and combined in the IoT (Internet of Things) platforms, such as advanced sensing, wearable devices, cloud and fog computing, and predictive and inferring techniques [11][12].
Wearable devices are powerful tools for supporting IoT systems because of their sensing, processing, and communication capability [13][14]. The term wearable devices cover a wide range of products integrated into clothing and accessories worn by the user and constantly connected to other intelligent electronic systems and the Internet network, allowing the detection, storage, and exchange of data in real-time and without human intervention [15][16]. Particularly, they allow detection of patients’ vital parameters (e.g., heart rate (HR), oxygen saturation- (SpO 2), body temperature, blood pressure (BP), etc.) through advanced sensors positioned in direct contact with the skin, enabling several advantages such as continuous monitoring, reduced health costs and hospitalization times, and more straightforward prescription of preventive care, crucial for elderly people and infants [17][18]. Moreover, the development of advanced sensing devices for monitoring biophysical and environmental parameters, with features including small sizes, reduced power consumption, non-invasiveness [19], and flexibility [20][21], is fundamental for developing the next generation of wearable devices.
The main contributions of the proposed review work are: A comprehensive overview of recent advances in sensing technologies to monitor the biophysical parameters suitable for integration into wearable and portable devices; specifically, we focused on advanced techniques for monitoring HR, BP, respiration rate (RR), blood glucose level and others, in a non-invasive or even contactless way. In addition, wearable applications involving Galvanic Skin Response (GSR) measurements are discussed, a standard indicator of the physical or psychological conditions, for predicting epileptic seizures [22], diagnosing bipolar dysfunction [23], and detecting sleepiness [24]. We investigated the application of sweat sensors for rapid and non-invasive detection of toxins, drugs, hormones, alcohol, and glucose level [25]. An overview of the IoT systems for health monitoring applications, focusing on the different IoT architectures and supported services. Analyzed systems make heavy use of wearable devices for high-resolution detection of the patient parameters, along with edge/fog computing to limit their requirements in terms of computational resources, power consumption, and energy autonomy [26]. Furthermore, cloud computing allows integrated management, and processing and storing of acquired data can be carried out. Artificial Intelligence (AI) and Machine Learning (ML) techniques can be integrated into their supported services to simplify the handling of a massive data amount and to infer useful information from them [27]. Finally, IoT frameworks for gait and life-quality monitoring are discussed, focusing on IoT systems for remote fall detection, based on wearable devices and ML techniques [28].
2. Overview of Innovative Sensing Systems and Algorithms for Monitoring Biophysical Parameters
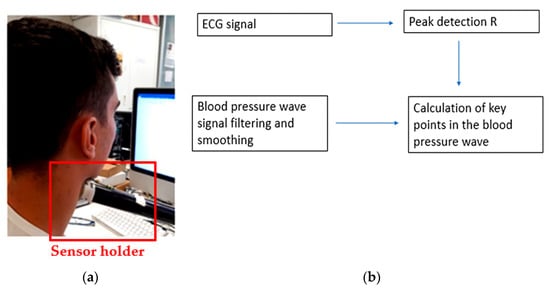
The holder was positioned and regulated before each test, during which the user approached the device until it touched the neck, as shown in Figure 1a. An algorithm was developed to identify diastolic points (minimum pressure signal), systolic points (maximum pressure signal), and dicrotic notches (aortic pressure transients). The employed algorithm, shown in Figure 1b, calculated the so-called R-points of the electrocardiogram (ECG) wave (systolic points corresponding to the heart contraction phase), thus obtaining the maximum pressure points of the blood pressure wave.
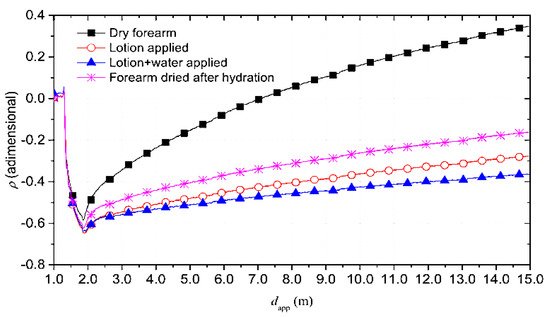
The reflectograms for the four conditions previously mentioned are reported in Figure 2 .
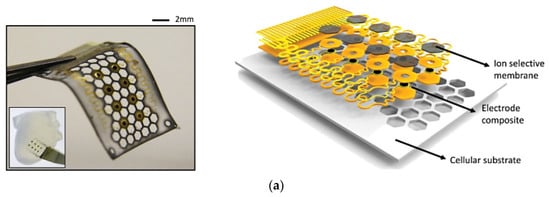
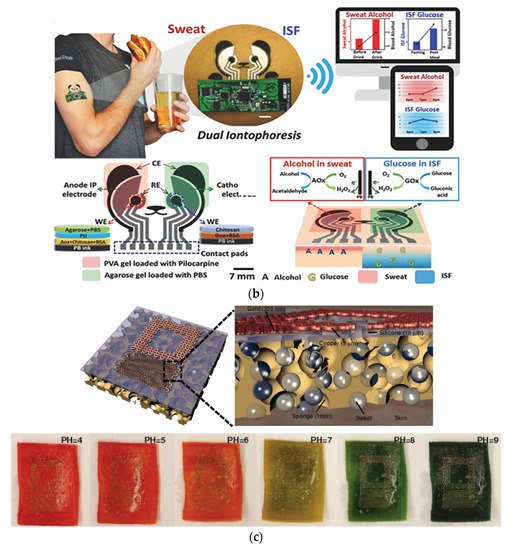
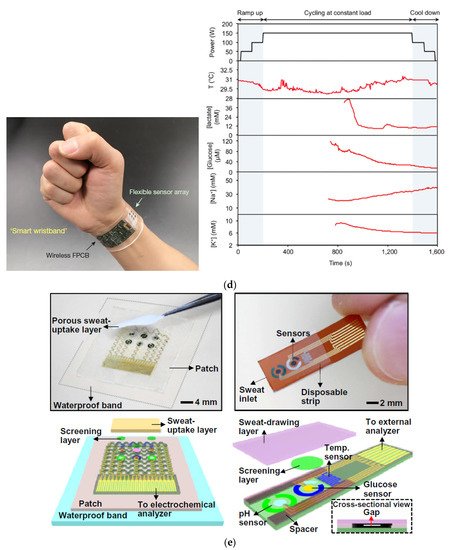
Cell substrate pores improved the flow of sweat accumulated under the sensor, improving perspiration ( Figure 3a) [31]. Figure 3b shows a “panda-like” tattoo platform including different hydrogels on the electrodes for efficient sampling and storage of biofluids [32]. Instead, Figure 3c illustrates a wireless extensible sensor for sweat detection on the skin’s surface, consisting of an inductive coil and a planar capacitor [33]. Figure 3d shows a thin rayon pad between the skin and the sensor array, which completely absorbed sweat [34]. In Figure 3e, an ultra-thin and stretchable, and miniaturized patch is depicted, applicable as a disposable strip [35].
3. Overview on IoT Systems for Health Monitoring Applications: Architecture Point of View and Supported Services
Moustafa et al. proposed an alternative IoT architecture for remotely controlling patients and managing different medical devices and sensors using Web Real-Time Communication (WebRTC) for supporting the communication between remote users and medical infrastructure [36]. An edge cloud architecture was applied to spare network bandwidth, guaranteeing real-time control of medical devices, using a central communication hub to supply an abstraction layer and aggregate videos and data from different source devices. Moreover, the edge cloud provided storage infrastructure and efficient communication for sensors and devices and acted as a proxy server. Indeed, the IoT gateways worked both as communication and aggregation hubs for videos and data storage, processing, and analytics. The edge cloud also offered push-mode remote monitoring for transmitting warning and alerts messages to the remote user when an anomaly was detected or pull-mode remote monitoring remote users to request specific past data and video, guaranteeing an improved privacy policy for stored data.
Farahani et al. stressed the relevance of fog computing as an intermediate layer between devices and the cloud to achieve greater speed, variety, and better latency when analyzing complex data from a patient-centric IoT healthcare system [37]. The proposed system comprised three main layers, viz. IoT eHealth Device Layer , IoT eHealth Fog Layer, and IoT eHealth Cloud Layer. The Device Layer included the medical devices used to monitor users’ health conditions, synchronizing collected data with the cloud layer. These devices can be divided into two main categories: (1) Physical sensors that are any medical devices with a wireless connection used to monitor patients’ health; (2) Virtual sensors that use mobile applications, software, and eHealth services to collect patient’s and environment data. As close as possible to the source devices, the proposed framework employed fog nodes to analyze and compress the acquired data and sent them to the cloud layer. The cloud layer connected the fog nodes and the health devices; also, it integrated the data from different devices, stored them, and made them accessible anytime to patients and doctors. This layer also analyzed the data to generate appropriate alarms and notifications for patients and physicians.
The mobile health (m-health) systems, as discussed by Almotiri et al., would bring many benefits such as rapid diagnosis, home rehabilitation, and remote monitoring [38]. The word m-health identifies the utilization of mobile devices, featured by compactness, low power consumption, IP connectivity, and security, to collect the health data, like blood pressure and blood sugar level, of a patient in real-time. The data were collected using several medical gadgets, such as wearable devices, saving them on network servers connected to the Internet. Thus, the system architecture was a component of the IoT architecture, constituted by multiple layers, namely a data collection layer, a data processing layer, and a data storage layer, as shown in Figure 4 .
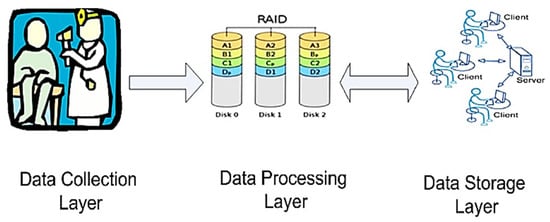
Each layer was based on several servers placed in different locations; the data processing layer analyzed the data stored in the storage layer; it comprised IoT servers, allowing the data to be available anywhere. The Health Insurance Portability and Accountability Act (HIPAA) defined the measure to adopt to achieve confidentiality, security, and privacy for the stored health data.
4. Conclusions
Information and communication technologies offer seamless opportunities to connect people and objects, simplifying and enriching our lives. Due to the widespread use of IoT platforms promoting advanced sensing systems and intelligent inferring methodologies, health systems are undergoing a true technical revolution, fundamentally transforming the way medical services are delivered.
References
- Chan, M.; Estève, D.; Fourniols, J.-Y.; Escriba, C.; Campo, E. Smart Wearable Systems: Current Status and Future Challenges. Artif. Intell. Med. 2012, 56, 137–156.
- Frischer, R.; Krejcar, O.; Maresova, P.; Fadeyi, O.; Selamat, A.; Kuca, K.; Tomsone, S.; Teixeira, J.P.; Madureira, J.; Melero, F.J. Commercial ICT Smart Solutions for the Elderly: State of the Art and Future Challenges in the Smart Furniture Sector. Electronics 2020, 9, 149.
- Lobaccaro, G.; Carlucci, S.; Löfström, E. A Review of Systems and Technologies for Smart Homes and Smart Grids. Energies 2016, 9, 348.
- de Fazio, R.; Sponziello, A.; Cafagna, D.; Velazquez, R.; Visconti, P. An Overview on Technologies and Devices against Covid-19 Pandemic Diffusion: Virus Detection and Monitoring Solutions. Int. J. Smart Sens. Intell. Syst. 2021, 14, 1–28.
- Latifi, R. Current Principles and Practices of Telemedicine and e-Health, 1st ed.; Ios Press, Inc.: Amsterdam, The Netherlands; Washington, DC, USA, 2008; ISBN 978-1-58603-806-9.
- Wen, H.J.; Tan, J. The Evolving Face of Telemedicine E-Health: Opening Doors and Closing Gaps in e-Health Services Opportunities Challenges. In Proceedings of the 36th Annual Hawaii International Conference on System Sciences, Big Island, HI, USA, 6–9 January 2003; pp. 1–12.
- Surantha, N.; Atmaja, P.; David; Wicaksono, M. A Review of Wearable Internet-of-Things Device for Healthcare. Procedia Comput. Sci. 2021, 179, 936–943.
- Nasajpour, M.; Pouriyeh, S.; Parizi, R.M.; Dorodchi, M.; Valero, M.; Arabnia, H.R. Internet of Things for Current COVID-19 and Future Pandemics: An Exploratory Study. J. Healthc. Inf. Res. 2020, 4, 325–364.
- Singh, R.P.; Javaid, M.; Haleem, A.; Suman, R. Internet of Things (IoT) Applications to Fight against COVID-19 Pandemic. Diabetes Metab. Syndr. 2020, 14, 521–524.
- Dong, Y.; Yao, Y.-D. IoT Platform for COVID-19 Prevention and Control: A Survey. IEEE Access 2021, 9, 49929–49941.
- Kadhim, K.T.; Alsahlany, A.M.; Wadi, S.M.; Kadhum, H.T. An Overview of Patient’s Health Status Monitoring System Based on Internet of Things (IoT). Wirel. Pers. Commun. 2020, 114, 2235–2262.
- Ennafiri, M.; Mazri, T. Internet of Things for Smart Healthcare: A Review on a Potential IOT Based System and Technologies to Control COVID-19 Pandemic. Innov. Smart Cities Appl. 4 2020, 183, 1256–1269.
- Zhang, L.; Yang, L.; Wang, Z.; Yan, D. Sports Wearable Device Design and Health Data Monitoring Based on Wireless Internet of Things. Microprocess. Microsyst. 2020, 103423, 1–7.
- Putri, A.; Ali, M.; Abdulmajid, M.S.; Hidayat, S.S. Wearable Sensor and Internet of Things Technology for Better Medical Science: A Review. Int. J. Emerg. Technol. Learn. (IJET) 2019, 7, 1–4.
- Burmaoglu, S.; Trajkovik, V.; Tutukalo, T.L.; Yalcin, H.; Caulfield, B. Chapter 14—Evolution Map of Wearable Technology Patents for Healthcare Field. In Wearable Technology in Medicine and Health Care; Tong, R.K.-Y., Ed.; Academic Press: Cambridge, MA, USA, 2018; pp. 275–290. ISBN 978-0-12-811810-8.
- Honarvar, M.G.; Latifi, M. Overview of Wearable Electronics and Smart Textiles. J. Text. Inst. 2017, 108, 631–652.
- Stavropoulos, T.G.; Papastergiou, A.; Mpaltadoros, L.; Nikolopoulos, S.; Kompatsiaris, I. IoT Wearable Sensors and Devices in Elderly Care: A Literature Review. Sensors 2020, 20, 2826.
- de Fazio, R.; Cafagna, D.; Marcuccio, G.; Minerba, A.; Visconti, P. A Multi-Source Harvesting System Applied to Sensor-Based Smart Garments for Monitoring Workers’ Bio-Physical Parameters in Harsh Environments. Energies 2020, 13, 2161.
- Jayathilaka, W.A.D.M.; Qi, K.; Qin, Y.; Chinnappan, A.; Serrano-García, W.; Baskar, C.; Wang, H.; He, J.; Cui, S.; Thomas, S.W.; et al. Significance of Nanomaterials in Wearables: A Review on Wearable Actuators and Sensors. Adv. Mater. 2019, 31, 1–21.
- Wang, C.; Xia, K.; Wang, H.; Liang, X.; Yin, Z.; Zhang, Y. Advanced Carbon for Flexible and Wearable Electronics. Adv. Mater. 2019, 31, 1–37.
- Lim, H.-R.; Kim, H.S.; Qazi, R.; Kwon, Y.-T.; Jeong, J.-W.; Yeo, W.-H. Advanced Soft Materials, Sensor Integrations, and Applications of Wearable Flexible Hybrid Electronics in Healthcare, Energy, and Environment. Adv. Mater. 2020, 32, 1–43.
- Nagai, Y.; Jones, C.I.; Sen, A. Galvanic Skin Response (GSR)/Electrodermal/Skin Conductance Biofeedback on Epilepsy: A Systematic Review and Meta-Analysis. Front. Neurol. 2019, 10, 1–8.
- Anwar, Y.; Khan, A.A. Assistive Technologies for Bipolar Disorder: A Survey. Int. J. Adv. Comput. Sci. Appl. 2019, 10, 490–499.
- Malathi, D.; Jayaseeli, J.D.; Madhuri, S.; Senthilkumar, K. Electrodermal Activity Based Wearable Device for Drowsy Drivers. J. Phys. Conf. Ser. 2018, 1000, 1–11.
- Chung, M.; Fortunato, G.; Radacsi, N. Wearable Flexible Sweat Sensors for Healthcare Monitoring: A Review. J. R. Soc. Interface 2019, 16, 1–15.
- Paul, A.; Pinjari, H.; Hong, W.-H.; Seo, H.C.; Rho, S. Fog Computing-Based IoT for Health Monitoring System. J. Sens. 2018, 2018, 1–8.
- Aldahiri, A.; Alrashed, B.; Hussain, W. Trends in Using IoT with Machine Learning in Health Prediction System. Forecasting 2021, 3, 181–206.
- Vallabh, P.; Malekian, R.; Ye, N.; Bogatinoska, D.C. Fall Detection Using Machine Learning Algorithms. In Proceedings of the 2016 24th International Conference on Software, Telecommunications and Computer Networks (SoftCOM), Split, Croatia, 22–24 September 2016; pp. 1–9.
- Zambrana-Vinaroz, D.; Vicente-Samper, J.M.; Juan, C.G.; Esteve-Sala, V.; Sabater-Navarro, J.M. Non-Invasive Device for Blood Pressure Wave Acquisition by Means of Mechanical Transducer. Sensors 2019, 19, 4311.
- Schiavoni, R.; Monti, G.; Piuzzi, E.; Tarricone, L.; Tedesco, A.; De Benedetto, E.; Cataldo, A. Feasibility of a Wearable Reflectometric System for Sensing Skin Hydration. Sensors 2020, 20, 2833.
- Lee, Y.K.; Jang, K.-I.; Ma, Y.; Koh, A.; Chen, H.; Jung, H.N.; Kim, Y.; Kwak, J.W.; Wang, L.; Xue, Y.; et al. Chemical Sensing Systems That Utilize Soft Electronics on Thin Elastomeric Substrates with Open Cellular Designs. Adv. Funct. Mater. 2017, 27, 1–8.
- Kim, J.; Sempionatto, J.R.; Imani, S.; Hartel, M.C.; Barfidokht, A.; Tang, G.; Campbell, A.S.; Mercier, P.P.; Wang, J. Simultaneous Monitoring of Sweat and Interstitial Fluid Using a Single Wearable Biosensor Platform. Adv. Sci. 2018, 5, 1–11.
- Huang, X.; Huang, X.; Liu, Y.; Chen, K.; Shin, W.-J.; Lu, C.-J.; Kong, G.-W.; Patnaik, D.; Lee, S.-H.; Cortes, J.F.; et al. Stretchable, Wireless Sensors and Functional Substrates for Epidermal Characterization of Sweat. Nano Micro Small 2014, 10, 3083–3090.
- Gao, W.; Emaminejad, S.; Nyein, H.Y.Y.; Challa, S.; Chen, K.; Peck, A.; Fahad, H.M.; Ota, H.; Shiraki, H.; Kiriya, D.; et al. Fully Integrated Wearable Sensor Arrays for Multiplexed in Situ Perspiration Analysis. Nature 2016, 529, 509–514.
- Lee, H.; Song, C.; Hong, Y.S.; Kim, M.S.; Cho, H.R.; Kang, T.; Shin, K.; Choi, S.H.; Hyeon, T.; Kim, D.-H. Wearable/Disposable Sweat-Based Glucose Monitoring Device with Multistage Transdermal Drug Delivery Module. Sci. Adv. 2017, 3, 1–9.
- Moustafa, H.; Schooler, E.M.; Shen, G.; Kamath, S. Remote Monitoring and Medical Devices Control in EHealth. In Proceedings of the 2016 IEEE 12th International Conference on Wireless and Mobile Computing, Networking and Communications (WiMob), New York, NY, USA, 17 October 2016; pp. 1–8.
- Farahani, B.; Firouzi, F.; Chang, V.; Badaroglu, M.; Constant, N.; Mankodiya, K. Towards Fog-Driven IoT EHealth: Promises and Challenges of IoT in Medicine and Healthcare. Future Gener. Comput. Syst. 2018, 78, 659–676.
- Almotiri, S.H.; Khan, M.A.; Alghamdi, M.A. Mobile Health (m-Health) System in the Context of IoT. In Proceedings of the 2016 IEEE 4th International Conference on Future Internet of Things and Cloud Workshops (FiCloudW), Vienna, Austria, 22 August 2016; pp. 39–42.




