| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Riccardo Dalle Grave | + 2283 word(s) | 2283 | 2020-07-05 19:49:58 | | | |
| 2 | Vicky Zhou | -39 word(s) | 2244 | 2020-10-29 10:15:00 | | |
Video Upload Options
Personalized cognitive-behavioural therapy for obesity (CBT-OB) CBT-OB is an innovative treatment designed to help patients maintain long-term weight loss by addressing some limitations of traditional behavioural treatment of obesity (BT-OB), namely the poor personalization of the intervention and the prevalent focus on helping the patients to reach behavioural change (i.e., eating and exercise habits) rather than a cognitive change oriented to long-term weight control. As such, CBT-OB includes the main procedures of traditional BT-OB, but includes new strategies and procedures, introduced according to the individual patient’s needs, to address specific cognitive processes that previous research has found be associated with treatment discontinuation, weight loss and weight maintenance. Moreover, it can be delivered in a stepped-care approach, including three levels of care (i.e., outpatient, day-hospital, and residential) to treat patients with severe and disabling obesity.
1. Introduction
Personalized cognitive behavioural therapy for obesity (CBT-OB) is a new treatment designed to help patients with obesity to achieve and maintain a healthy weight loss through personalized combinations of strategies and procedures from traditional behavioural therapy for obesity (BT-OB) with others addressing some specific “cognitive processes” that the evidence suggests can influence attrition, weight loss and weight-loss maintenance. Personalized CBT-OB was devised by Dalle Grave and colleagues in Verona (Italy)[1][2], and it has been adapted to be delivered at outpatient, day-hospital and residential settings.
2. The Theory
The traditional treatments of obesity mainly aim to address the biological and behavioural factors hindering weight loss and maintenance, with very little attention to the cognitive processes that may be at play[3]. Failure to address a patients’ ability to adhere to lifestyle modification over time may therefore be one of the reasons why biological and behavioural treatments have limited effectiveness in promoting long-term weight loss[4]. Support to this theory comes by recent studies showing that there are several cognitive factors associated with treatment attrition, weight loss and weight maintenance (see Table 1).
Personalized CBT-OB has been designed with the aim to address some limitations of traditional behavioural treatment of obesity (BT-OB) namely the poor personalization of the intervention and the prevalent focus on helping the patients to reach behavioural change (i.e., eating and exercise habits) rather than a cognitive change oriented to long-term weight control.
|
Table 1. Cognitive factors associated with treatment discontinuation, amount of weight lost and weight-loss maintenance Cognitive factors associated with treatment discontinuation:
Cognitive factors associated with amount of weight lost:
Cognitive factors associated with weight-loss maintenance:
|
Goals, general strategies and procedures of personalized CBT-OB
The main goals of personalized CBT-OB are to help patients to (i) reach, accept and maintain a healthy amount of weight loss (i.e., 5–10% of their starting body weight); (ii) adopt and maintain a lifestyle conducive to weight control; and (iii) develop a stable “weight-control mind-set”.
CBT-OB therapists adopt, like other forms of CBT, a therapeutic style designed to develop and nurture a collaborative working relationship with the patients (collaborative empiricism). In addition to some of the procedures adopted by BT-OB (i.e., self-monitoring, goal setting, stimulus control, contingency management, behavioural substitution, skills for increasing social support, problem-solving and relapse prevention), CBT-OB includes specific cognitive strategies and procedures, some of which have been adapted from ‘enhanced’ CBT (CBT-E) for eating disorders[5] [5, 6] and Cooper et al. [7], and some have been developed ex novo. These integrations enable the treatment to be personalized, and help patients address the processes that our previous research has found to be respectively associated with drop-out, the amount of weight lost, and maintaining a lower weight in the long term (see Table 2).
Further details of personalized CBT-OB, together with a comprehensive description of the treatment and its implementation, can be found in the main treatment guide “Treating Obesity with Personalized Cognitive Behavioral Therapy”[6].
|
Table 2. CBT-OB strategies and procedures for reducing attrition, enhancing weight loss and improving weight-loss maintenance Strategies and procedures for minimising attrition:
Strategies and procedures for enhancing weight loss
Strategies and procedures for improving weight-loss maintenance
|
3. The Versions of CBT-OB
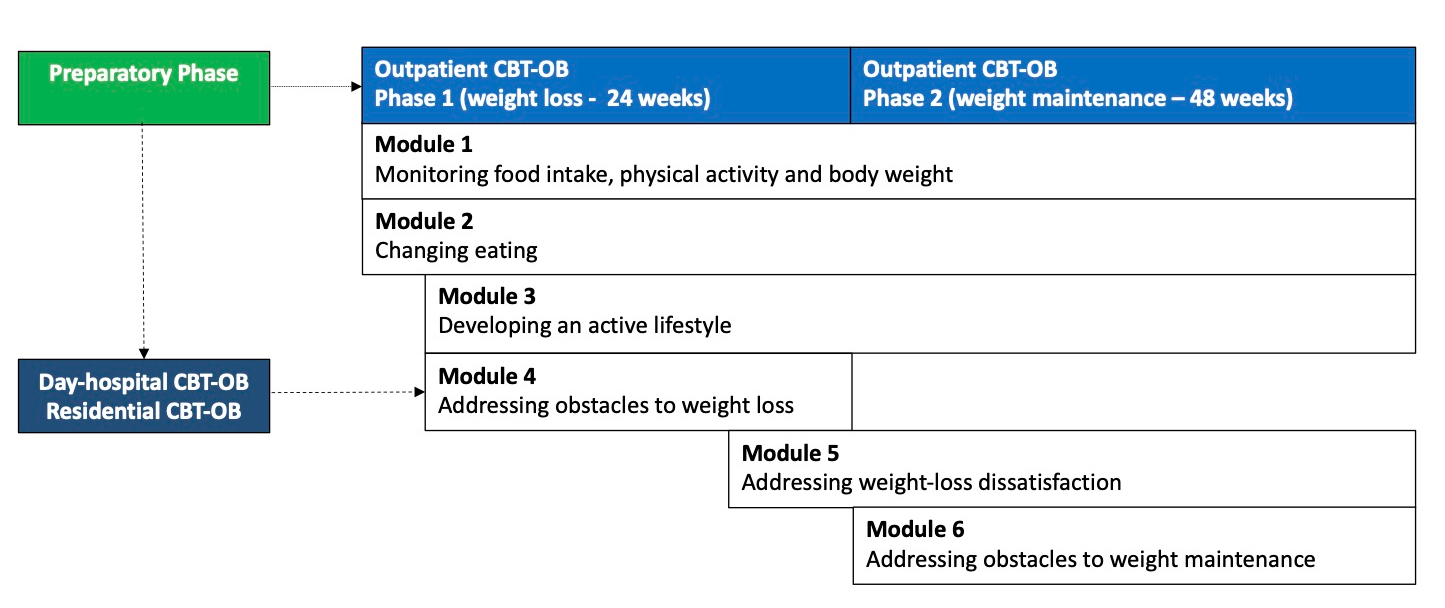
CBT-OB has been designed to treat all classes of obesity within a stepped-care approach involving three levels of care (outpatient, day-hospital and residential). Outpatient CBT-OB can be delivered individually by a single therapist or in group by two therapists. It includes the following phases (see Figure 1):
- Preparatory Phase. This is delivered in one or two sessions, and has the aims of assessing the nature and severity of a patient’s obesity, as well as any associated medical and psychosocial comorbidities, as well as engaging the patient(s) in the treatment.
- Phase 1. This has been designed to help patients achieve a healthy rate of weight loss and be satisfied with the resulting weight. It lasts about 24 weeks and is delivered across 16 sessions, the first eight of which are held once a week, and the remaining eight on a two-weekly basis.
- Phase 2. This has the aim of helping patients to develop a lifestyle and mindset conducive to long-term weight maintenance. It usually lasts 48 weeks and is delivered across 12 sessions that are held at four-weekly intervals.
Figure 1. The map of personalised cognitive behavioural therapy for obesity (CBT-OB)
CBT-OB is delivered in six modules (see Table 3), each including specific strategies and procedures that may be adapted to the patient’s individual progress and barriers; the six modules are introduced in a flexible and individualized way, according to the patient’s needs, across Phase 1 and Phase 2.
Each session lasts 45 minutes (90 minutes when the treatment is delivered in group), and is divided into five parts, each with a distinct objective, specifically:
- In-session collaborative weighing (up to 5 minutes)
- Reviewing self-monitoring and other homework (up to 10 minutes)
- Collaboratively setting the session agenda (about 2 minutes)
- Working through the agenda and agreeing on homework tasks (up to 30 minutes).
- Concluding the session (about 3 minutes). This includes summarizing what has been addressed in session, confirming the homework assignment(s), and scheduling the next appointment.
Day-hospital and residential CBT-OB, on the other hand, which are indicated for patients with severe and disabling obesity, last 21 days.
Finally, CBT-OB may be also associated with weight loss drugs and/or bariatric surgery in selected case, and can also be adapted for patients with obesity associated with binge-eating disorder (BED).
|
Table 3. The main procedures of the six CBT-OB modules Module 1 - Monitoring food Intake, physical activity and body weight
Module 2 - Changing eating
Module 3 - Developing an active lifestyle
Module 4 - Addressing obstacles to weight loss
Module 5 - Addressing weight-loss dissatisfaction
Module 6: Addressing the obstacles to weight maintenance
|
4. The Current Status of Personalized CBT-OB
The research findings may be summarised as follows:
- A randomized control trial assessing the effectiveness of personalized CBT-OB (3 weeks of residential CBT-OB followed by outpatient CBT- OB) found that weight loss at 43 weeks in completers (n=69) was about 15%. The treatment was associated with improvements in cardiovascular risk factors and psychological profiles; what is more, no tendency to regain weight was observed between 6 and 12 months[6].
- A real-world study, conducted in an Italian National Health Service obesity clinic, assessed the effectiveness of group CBT-OB in 67 patients with severe obesity. 76.2% patients completed the treatment, displaying an average weight loss of 11.5% after 6 months and 9.9% after 18 months. This weight loss was associated with a significant reduction in cardiovascular risk factors, anxiety, depression and eating-disorder psychopathology, and an improvement in obesity-related quality of life[7].
- A study compared the long-term effects of residential CBT-OB in 54 patients with severe obesity with or without BED. Even though patients did not receive outpatient CBT-OB after discharge, at 5-year follow-up, 51.5% of the former group no longer met the diagnostic criteria for BED. Moreover, no difference was observed between the two groups in terms of mean weight loss (6.3 kg in BED vs. 7.4 kg in non-BED)[8].
References
- Riccardo Dalle Grave; Massimiliano Sartirana; Marwan El Ghoch, M; Simona Calugi. Treating obesity with personalized cognitive behavioral therapy.; Springer: Cham, 2018; pp. 244.
- Riccardo Dalle Grave; Massimiliano Sartirana; Simona Calugi; Personalized cognitive-behavioural therapy for obesity (CBT-OB): theory, strategies and procedures.. BioPsychoSocial Medicine 2020, 14, 5-8, 10.1186/s13030-020-00177-9.
- Zafra Cooper; Christopher G Fairburn; A new cognitive behavioural approach to the treatment of obesity.. Behaviour Research and Therapy 2001, 39, 499-511, 10.1016/s0005-7967(00)00065-6.
- Riccardo Dalle Grave; Simona Calugi; Giulio Marchesini; The influence of cognitive factors in the treatment of obesity: Lessons from the QUOVADIS study. Behaviour Research and Therapy 2014, 63, 157-161, 10.1016/j.brat.2014.10.004.
- Riccardo Dalle Grave; Simona Calugi. Cognitive behavior therapy for adolescents with eating disorders; Guilford Press: New York, 2020; pp. 304.
- Riccardo Dalle Grave; Simona Calugi; Ilaria Gavasso; Marwan El Ghoch; Giulio Marchesini; A randomized trial of energy-restricted high-protein versus high-carbohydrate, low-fat diet in morbid obesity. Obesity 2013, 21, 1774-1781, 10.1002/oby.20320.
- Riccardo Dalle Grave; Simona Calugi; Giovanna Bosco; Luigi Valerio; Chiara Valenti; Marwan El Ghoch; Dante Zini; Personalized group cognitive behavioural therapy for obesity: a longitudinal study in a real-world clinical setting. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity 2018, 25, 337-346, 10.1007/s40519-018-0593-z.
- Simona Calugi; Antonella Ruocco; Marwan El Ghoch; Coppini Andrea; Eleonora Geccherle; Federica Sartori; Riccardo Dalle Grave; Residential cognitive-behavioral weight-loss intervention for obesity with and without binge-eating disorder: A prospective case-control study with five-year follow-up. International Journal of Eating Disorders 2016, 49, 723-730, 10.1002/eat.22549.