
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Leonard Ionut Atanase | + 1553 word(s) | 1553 | 2021-05-14 11:17:27 | | | |
| 2 | Dean Liu | -10 word(s) | 1543 | 2021-07-14 04:18:50 | | |
Video Upload Options
Periodontal diseases are worldwide health problems that negatively affect the lifestyle of many people. The long-term effect of the classical treatments, including the mechanical removal of bacterial plaque, is not effective enough, causing the scientific world to find other alternatives.
1. Introduction
In the last 30 years, the field of controlled drug delivery systems, particularly the study of polymers as drug carriers, has received great interest. The polymer acts either as a support by protecting the bioactive agent during its transfer through the body until release or by its properties controlling the release kinetics. Such a controlled release system contains the bioactive principle loaded into the polymeric matrix or chemically bound (ionic, covalent) to the base chain, being administered orally, parenterally, transdermally, or surgically implanted in the body [1]. The drug will then be released at the site of the disease by diffusion, by hydrolysis of the chemical bonds between it and the support, or by erosion of the surface of the polymeric matrix [2].
The polymeric matrix must have an optimal combination of binding properties for compounds that work in or in contact with the human body, which makes biopolymers (proteins, polysaccharides) ideal candidates. Although the mechanisms of action of the release systems thus obtained are not yet fully elucidated and their technologies are not yet optimized, the results of some clinical experiments attest to the special value of some natural macromolecular compounds, and to a lesser extent of synthetic polymers, as adjuvants for the conditioning and immobilization of biologically active substances.
The main constraints that a polymer for bio-applications must meet are the (i) biocompatible and biodegradable. This assumes that the polymer must degrade in vivo into compounds that are easily eliminated from the body. Otherwise, the polymeric system must be surgically removed after completely or almost completely releasing the drug. (ii) The degradation products must be non-toxic and not create an inflammatory response in the body. (iii) Degradation of the polymer must occur within a reasonable period of time. In addition to these constraints, the choice of polymeric matrix also takes into account several criteria: (i) Molecular weight and polydispersity of molar masses. (ii) Basic chain geometry: linearity or cyclicity, branching, reticulation, etc. (iii) The chemical nature of the polymer, such as its chemical composition, aqueous solubility, and ionic charge. (iv) The polymer–drug relationship, such as the type of chemical bond that the partners can form (covalent, ionic, or coordinative); the physical interactions between partners, if no chemical bonds are involved; location of the pharmacologically active agent in the polymer (per chain, as a substituent, or included in the matrix). (v) The stereochemical phenomena.
The mentioned restrictions are fulfilled by few synthetic polymers, but mostly by biopolymers. Of this large category, the most used are polysaccharides and proteins; this review focuses only on polysaccharides and their derivatives. Given the specific diseases of the oral cavity, among which periodontal disease ranks first, the classes of drugs associated with different types of polysaccharide-based supports are those with anti-inflammatory and antimicrobial action on the microbial flora that causes periodontitis.
Numerous forms of the presentation of polymer–drug systems are currently known, these being chosen depending on the nature of the disease, the administration mode, the type of polymer used, etc. One of them is hydrogels (in the form of films, micro-/nanoparticles, implants, etc.), in which the drug can be included, encapsulated, or adsorbed on the surface. Another possibility is the direct association of the biologically active compound with the polymer chains by covalent or ionic binding (polymer–drug conjugates).
The literature abounds with a huge amount of articles dealing with the problem of classifying polymer–drug systems according to the way partners associate, how they are formulated, how they respond to external stimuli, the nature of the support polymer, the mechanism and kinetics of the release process, etc. This review will not refer to these aspects but will only investigate the polymer–drug systems with applications in the treatment of periodontitis.
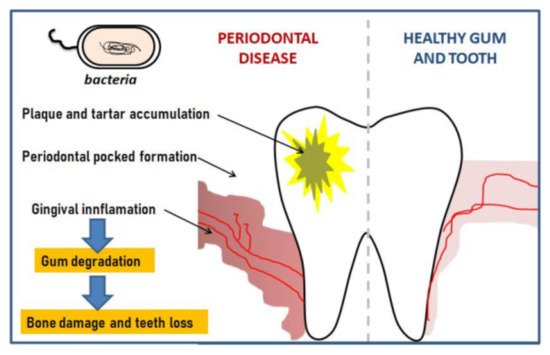
Apart from trauma produced by injuries, the most common diseases of the oral cavity are tooth decay, periodontal disease, oral infections, and cancer. It is estimated, for example, that approximately 48% of the US adult population is affected by periodontitis, but similar results have been reported in other countries. Periodontitis is therefore a chronic inflammatory disease of the periodontal tissue caused by pathogenic microorganisms and characterized by the destruction of the supporting structures of the teeth [3]. The inflammation is first located in the gum but then penetrates deep and in the absence of treatment creates bags colonized by anaerobic bacteria that erode the supporting ligaments of the tooth until it is lost; the progress of the inflamed bags can take several years. Several inflammatory and degenerative stages of the tissue surrounding the tooth are highlighted, the gum, periodontal ligaments, enamel, and alveolar bone being affected in turn; these stages in the evolution of the disease are suggestively presented in Figure 1 [4].
2. The Prevention of Periodontal Disease
References
- DeRossi, D. Polymer Gels; Plenum Press: New York, NY, USA, 1991.
- Dunn, R.L.; Ottenbrite, R.M. Polymeric Drugs and Drug Delivery Systems; American Chemical Society: Washington, DC, USA, 1991.
- Kononen, E.; Gursoy, M.; Gursoy, U.K. Periodontitis: A multifaceted disease of tooth-supporting tissues. J. Clin. Med. 2019, 8, 1135.
- Zieba, M.; Chaber, P.; Duale, K.; Maksymiak, M.M.; Basczok, M.; Kowalczuk, M.; Adamus, G. Polymeric carriers for delivery systems in the treatment of chronic periodontal disease. Polymers 2020, 12, 1574.
- Socransky, S.S.; Haffajee, A.D.; Cugini, M.A.; Smith, C.; Kent, R.L.J. Microbial complexes in subgingival plaque. J. Clin. Periodontol. 1998, 25, 134–144.
- Lamont, R.J.; Koo, H.; Hajishengallis, G. The oral microbiota: Dynamic communities and host interactions. Nat. Rev. Microbiol. 2018, 16, 745–759.
- Rams, T.E.; Degener, J.E.; van Winkelhoff, A.J. Antibiotic resistance in human chronic periodontitis microbiota. J. Periodontol. 2014, 85, 160–169.
- Wade, G.W. The oral microbiome in health and disease. Pharmacol. Res. 2013, 69, 137–143.
- Pflughoeft, K.J.; Versalovic, J. Human microbiome in health and disease. Annu. Rev. Pathol. 2012, 7, 99–122.
- Konig, J.; Schwahn, C.; Fanghanel, J.; Plotz, J.; Hoffmann, T.; Kocher, T. Repeated scaling versus surgery in young adults with generalized advanced periodontitis. J. Periodontol. 2008, 79, 1006–1013.
- Lundgren, D.; Asklöw, B.; Thorstensson, H.; Härefeldt, A.M. Success rates in periodontal treatment as related to choice of evaluation criteria. Presentation of an evaluation criteria staircase for costbenefit use. J. Clin. Periodontol. 2001, 28, 23–30.
- Darveau, R.P. Periodontitis: A polymicrobial disruption of host homeostasis. Nat. Rev. Microbiol. 2010, 8, 481–490.
- Holpuch, A.; Desai, K.G.; Schwendeman, S.; Mallery, S. Optimizing therapeutic efficacy of chemopreventive agents. A critical review of delivery strategies in oral cancer chemoprevention clinical trials. J. Carcinog. 2011, 10, 23.
- Sankar, V.; Hearnden, V.; Hull, K.; Juras, D.V.; Greenberg, M.S.; Kerr, A.R.; Lockhart, P.B.; Patton, L.L.; Porter, S.; Thornhill, M. Local drug delivery for oral mucosal diseases. Challenges and opportunities. Oral Dis. 2011, 17, 73–84.
- Rata, D.M.; Cadinoiu, A.N.; Burlui, V.; Atanase, L.I. Polysaccharide-based orodental delivery systems. In Polysaccharide Carriers for Drug Delivery; Maiti, S., Jana, S., Eds.; Woodhead Publishing: Sawston, UK, 2019; pp. 685–711.
- Rajeshwari, H.R.; Dhamecha, D.; Jagwani, S.; Rao, M.; Jadhav, K.; Shaikh, S.; Puzhankara, L.; Jalalpure, S. Local drug delivery systems in the management of periodontitis: A scientific review. J. Control. Rel. 2019, 307, 393–409.




