
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Arianna Dal Buono | + 2769 word(s) | 2769 | 2021-07-05 08:13:18 | | | |
| 2 | Vivi Li | Meta information modification | 2769 | 2021-07-13 10:49:18 | | |
Video Upload Options
Inflammatory bowel diseases (IBD) are chronic, progressive, and disabling conditions, characterized by a relapsing and remitting behavior and long-term complications (i.e., colo-rectal cancer and demolitive surgery). Dedicated physicians are becoming confident with the ”treat-to-target” strategy in the management of IBD, aiming to prevent end-organ dysfunction. For years, symptom control has been the primary therapeutic goal of IBD patients.
1. Introduction
Inflammatory bowel diseases (IBD) are chronic, progressive, and disabling conditions, characterized by a relapsing and remitting behavior and long-term complications (i.e., colo-rectal cancer and demolitive surgery) [1][2]. Dedicated physicians are becoming confident with the “treat-to-target” strategy in the management of IBD, aiming to prevent end-organ dysfunction [3][4]. For years, symptom control has been the primary therapeutic goal of IBD patients. However, clinical remission is not a reliable outcome for the optimal management of IBD. Indeed, one out of four patients who are clinically asymptomatic can have an endoscopically active disease. Conversely, even in the presence of endoscopic remission, symptoms continue to be reported [5][6]. In the need for objective and measurable endpoints, bowel ultrasound (BUS) has gained increasing relevance. Traditionally, ultrasound was not considered a valid method for the assessment of the small bowel and colon [7]. It has taken a long time since the first studies in the 1970s on the effectiveness of this technique for bowel examination and its recent scientific acknowledgement [7]. According to the Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE-II), transmural healing (TH), assessed by imaging techniques including bowel ultrasound (BUS), is considered a treatment target neither in Crohn’s disease (CD) nor in ulcerative colitis (UC) [4]. Nevertheless, especially in CD, transmural healing is an adjunctive outcome to endoscopic remission and might represent a state of deeper healing [4]. Current recommendations recognize BUS as a valid method for the assessment of the small bowel in newly diagnosed CD and, generally, for the monitoring of IBD [8]; however, a standardization of the intestinal and extraintestinal features of active disease is still needed. The main advantages of BUS are its non-invasiveness and low costs compared to computed tomography (CT) or magnetic resonance imaging (MRI) [9]. It has been recently demonstrated that when performed by a skilled operator, BUS has a comparable sensitivity and specificity to second-level techniques for assessing disease activity and complications of IBD [9][10][11]. Moreover, BUS is readily available and can be performed bedside by the dedicated gastroenterologist upon need (i.e., point-of-care BUS (POCBUS)) [12]. The monitoring through BUS of the bowel wall thickness (BWT) predicts the outcomes of IBD patients, particularly in CD for its transmural features [9][10][11].
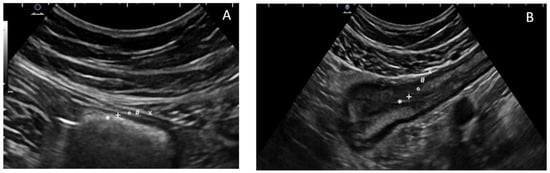
2. Technique and Features of Normality
 |
|||
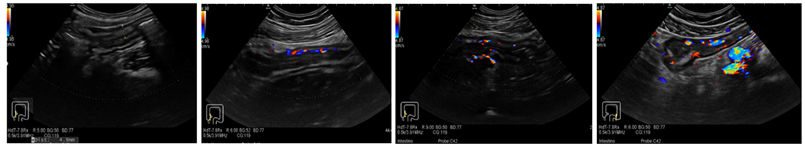
| Grade 1 | Grade 2 | Grade 3 | Grade 4 |
| No vascularization signal at color Doppler | Mild: minimal signal, short stretches of vascularity in spots | Moderate: longer stretches of vascularity, blood vessels located only intra-mural |
Severe: long continuous intra- and extra-mural blood vessels, extending into the mesentery |
3. Crohn’s Disease in Bowel Ultrasound
| Indications to Perform BUS in Crohn’s Disease |
|---|
| Initial work-up in suspected CD (i.e., differential diagnosis) |
| Baseline evaluation of disease activity and extension before therapy |
| Suspected complications (i.e., fistulas, abscesses, strictures) |
| Monitoring after/during the treatment course (response vs. worsening) |
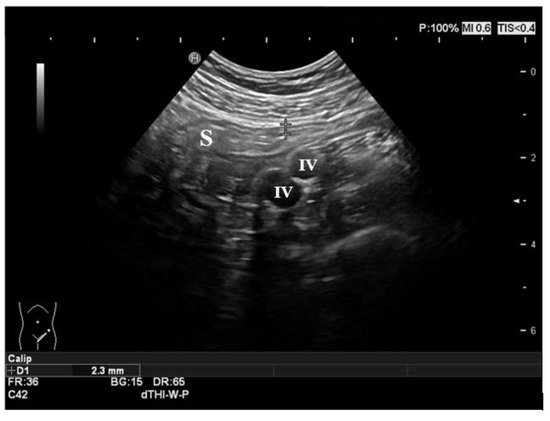
3.1. Ultrasound Features of CD
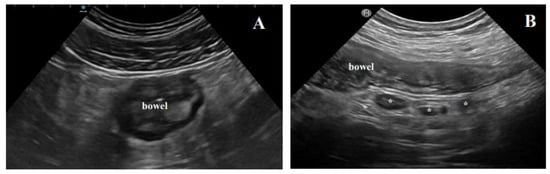
3.2. Complications of Crohn’s Disease
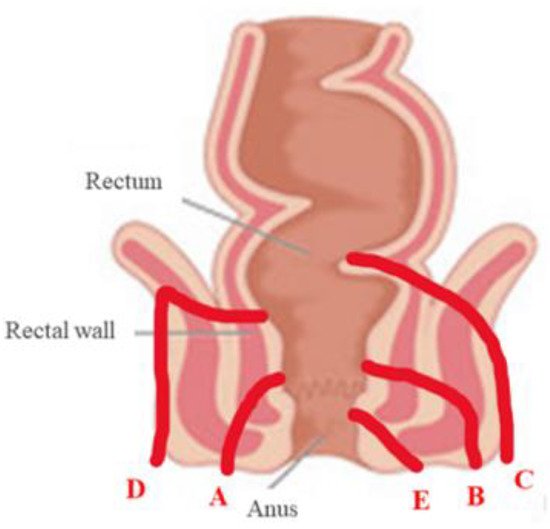
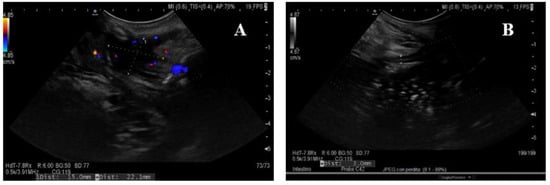
3.3. Transperineal Ultrasound
References
- Ungaro, R.; Mehandru, S.; Allen, P.B.; Peyrin-Biroulet, L.; Colombel, J.F. Ulcerative colitis. Lancet 2017, 389, 1756–1770.
- Torres, J.; Mehandru, S.; Colombel, J.F.; Peyrin-Biroulet, L. Crohn’s disease. Lancet 2017, 389, 1741–1755.
- Turner, D.; Ricciuto, A.; Lewis, A.; D’Amico, F.; Dhaliwal, J.; Griffiths, A.M.; Bettenworth, D.; Sandborn, W.J.; Sands, B.E.; Reinisch, W.; et al. International Organization for the Study of IBD. STRIDE-II: An Update on the Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE) Initiative of the International Organization for the Study of IBD (IOIBD): Determining Therapeutic Goals for Treat-to-Target strategies in IBD. Gastroenterology 2021, 160, 1570–1583.
- Colombel, J.-F.; D’haens, G.; Lee, W.-J.; Petersson, J.; Panaccione, R. Outcomes and Strategies to Support a Treat-to-target Approach in Inflammatory Bowel Disease: A Systematic Review. J. Crohn’s Colitis 2020, 14, 254–266.
- Colombel, J.F.; Keir, M.E.; Scherl, A.; Zhao, R.; de Hertogh, G.; Faubion, W.A.; Lu, T.T. Discrepancies between patient reported outcomes, and endoscopic and histological appearance in UC. Gut 2017, 66, 2063–2068.
- Colombel, J.F.; Shin, A.; Gibson, P.R. AGA Clinical Practice Update on functional gastrointestinal symptoms in patients with inflammatory bowel disease: Expert review. Clin. Gastroenterol. Hepatol. 2019, 17, 380–390.
- Holt, S.; Samuel, E. Grey scale ultrasound in Crohn’s disease. Gut 1979, 20, 590–595.
- Maaser, C.; Sturm, A.; Vavricka, S.R.; Kucharzik, T.; Fiorino, G.; Annese, V.; Calabrese, E.; Baumgart, D.C.; Bettenworth, D.; Borralho Nunes, P.; et al. European Crohn’s and Colitis Organization [ECCO] and the European Society of Gastrointestinal and Abdominal Radiology [ESGAR]. ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 1: Initial diagnosis, monitoring of known IBD, detection of complications. J. Crohn’s Colitis 2019, 1, 144–164.
- Fraquelli, M.; Castiglione, F.; Calabrese, E.; Maconi, G. Impact of intestinal ultrasound on the management of patients with inflammatory bowel disease: How to apply scientific evidence to clinical practice. Dig. Liver Dis. 2020, 52, 9–18.
- Allocca, M.; Fiorino, G.; Bonovas, S.; Furfaro, F.; Gilardi, D.; Argollo, M.; Magnoni, P.; Peyrin-Biroulet, L.; Danese, S. Accuracy of Humanitas Ultrasound Criteria in assessing disease activity and severity in ulcerative colitis: A prospective study. J. Crohn’s Colitis 2018, 12, 1385–1391.
- Allocca, M.; Filippi, E.; Costantino, A.; Bonovas, S.; Fiorino, G.; Furfaro, F.; Peyrin-Biroulet, L.; Fraquelli, M.; Caprioli, F.; Danese, S. Milan Ultrasound Criteria are accurate in assessing disease activity in ulcerative colitis: External validation. United Eur. Gastroenterol. J. 2020, 21, 2050640620980203.
- Allocca, M.; Furfaro, F.; Fiorino, G.; Peyrin-Biroulet, L.; Danese, S. Point-of-Care Ultrasound in Inflammatory Bowel Disease. J. Crohn’s Colitis 2021, 15, 143–151.
- Nylund, K.; Maconi, G.; Hollerweger, A.; Ripolles, T.; Pallotta, N.; Higginson, A.; Serra, C.; Dietrich, C.F.; Sporea, I.; Saftoiu, A. EFSUMB recommendations and guidelines for gastrointestinal ultrasound. Ultraschall Med. Eur. J. Ultrasound 2017, 38, e1–e15.
- Maconi, G.; Nylund, K.; Ripolles, T.; Calabrese, E.; Dirks, K.; Dietrich, C.F.; Hollerweger, A.; Sporea, I.; Saftoiu, A.; Maaser, C.; et al. EFSUMB recommendations and clinical guidelines for intestinal ultrasound (GIUS) in inflammatory bowel diseases. Ultraschall Med. Eur. J. Ultrasound 2018, 39, 304–317.
- Atkinson, N.S.S.; Bryant, R.V.; Dong, Y.; Maaser, C.; Kucharzik, T.; Maconi, G.; Asthana, A.K.; Blaivas, M.; Goudie, A.; Gilja, O.H. How to perform gastrointestinal ultrasound: Anatomy and normal findings. World J. Gastroenterol. 2017, 23, 6931–6941.
- Lu, C.; Merrill, C.; Medellin, A.; Novak, K.; Wilson, S.R. Bowel ultrasound state of the art: Grayscale and doppler ultrasound, contrast enhancement, and elastography in Crohn Disease. J. Ultrasound Med. 2019, 38, 271–288.
- Fraquelli, M.; Colli, A.; Casazza, G.; Paggi, S.; Colucci, A.; Massironi, S.; Duca, P.; Conte, D. Role of US in detection of Crohn disease: Meta-analysis. Radiology 2005, 236, 95–101.
- Horsthuis, K.; Bipat, S.; Bennink, R.J.; Stoker, J. Inflammatory bowel disease diagnosed with US, MR, scintigraphy, and CT: Meta-analysis of prospective studies. Radiology 2008, 247, 64–79.
- Limberg, B. Diagnostik von chronisch-entzündlichen Darmerkrankungen durch Sonographie [Diagnosis of chronic inflammatory bowel disease by ultrasonography]. Z. Gastroenterol. 1999, 37, 495–508.
- Sagami, S.; Kobayashi, T.; Aihara, K.; Umeda, M.; Morikubo, H.; Matsubayashi, M.; Kiyohara, H.; Nakano, M.; Ohbu, M.; Hibi, T. Transperineal ultrasound predicts endoscopic and histological healing in ulcerative colitis. Aliment. Pharmacol. Ther. 2020, 51, 1373–1383.
- Kucharzik, T.; Wittig, B.M.; Helwig, U.; Börner, N.; Rössler, A.; Rath, S.; Maaser, C.; TRUST Study Group. Use of Intestinal Ultrasound to Monitor Crohn’s Disease Activity. Clin. Gastroenterol. Hepatol. 2017, 15, 535–542.
- Dong, J.; Wang, H.; Zhao, J.; Zhu, W.; Zhang, L.; Gong, J.; Li, Y.; Gu, L.; Li, J. Ultrasound as a diagnostic tool in detecting active Crohn’s disease: A meta-analysis of prospective studies. Eur. Radiol. 2014, 24, 26–33.
- Maconi, G.; Carsana, L.; Fociani, P.; Sampietro, G.M.; Ardizzone, S.; Cristaldi, M.; Parente, F.; Vago, G.L.; Taschieri,, A.M.; Bianchi Porro, G. Small bowel stenosis in Crohn’s disease: Clinical, biochemical and ultrasonographic evaluation of histological features. Alim. Pharmacol. Ther. 2003, 18, 749–756.
- Rigazio, C.; Ercole, E.; Laudi, C.; Daperno, M.; Lavagna, A.; Crocellà, L.; Bertolino, F.; Viganò, L.; Sostegni, R.; Pera, A.; et al. Abdominal bowel ultrasound can predict the risk of surgery in Crohn’s disease: Proposal of an ultrasonographic score. Scand. J. Gastroenterol. 2009, 44, 585–593.
- Drews, B.H.; Barth, T.F.; Hänle, M.M.; Akinli, A.S.; Mason, R.A.; Muche, R.; Thiel, R.; Pauls, S.; Klaus, J.; Von Boyen, G.; et al. Comparison of sonographically measured bowel wall vascularity, histology, and disease activity in Crohn’s disease. Eur. Radiol. 2009, 19, 1379–1386.
- Sasaki, T.; Kunisaki, R.; Kinoshita, H.; Yamamoto, H.; Kimura, H.; Hanzawa, A.; Shibata, N.; Yonezawa, H.; Miyajima, E.; Sakamaki, K.; et al. Use of color Doppler ultrasonography for evaluating vascularity of small intestinal lesions in Crohn’s disease: Correlation with endoscopic and surgical macroscopic findings. Scand. J. Gastroenterol. 2014, 49, 295–301.
- Maconi, G.; Di Sabatino, A.; Ardizzone, S.; Greco, S.; Colombo, E.; Russo, A.; Cassinotti, A.; Casini, V.; Corazza, G.R.; Bianchi Porro, G.; et al. Prevalence and clinical significance of sonographic detection of enlarged regional lymph nodes in Crohn’s disease. Scand. J. Gastroenterol. 2005, 40, 1328–1333.
- Maconi, G.; Greco, S.; Duca, P.; Ardizzone, S.; Massari, A.; Cassinotti, A.; Radice, E.; Porro, G.B. Prevalence and clinical significance of sonographic evidence of mesenteric fat alterations in Crohn’s disease. Inflamm. Bowel Dis. 2008, 14, 1555–1561.
- Cammarota, T.; Ribaldone, D.G.; Resegotti, A.; Repici, A.; Danese, S.; Fiorino, G.; Sarno, A.; Robotti, D.; Debani, P.; Bonenti, G.; et al. Role of bowel ultrasound as a predictor of surgical recurrence of Crohn’s disease. Scand. J. Gastroenterol. 2013, 48, 552–555.
- Ribaldone, D.G.; Cammarota, T.; Resegotti, A.; Sarno, A.; Robotti, D.; Debani, P.; Bonenti, G.; Bresso, F.; Pellicano, R.; Adriani, A.; et al. Power Doppler sonography to predict the risk of surgical recurrence of Crohn’s disease. J. Ultrasound 2014, 18, 51–55.
- Ribaldone, D.G.; Cammarota, T.; Resegotti, A.; Astegiano, M. A preserved stratified pattern of the bowel wall 1 year after major surgery does not influence the surgical recurrence of Crohn’s disease. Ir. J. Med. Sci. 2016, 185, 269–270.
- Allocca, M.; Fiorino, G.; Bonifacio, C.; Furfaro, F.; Gilardi, D.; Argollo, M.; Peyrin-Biroulet, L.; Danese, S. Comparative accuracy of Bowel Ultrasound versus Magnetic Resonance Enterography in combination with colonoscopy in assessing Crohn’s disease and guiding clinical decision-making. J. Crohn’s Colitis 2018, 12, 1280–1287.
- Bettenworth, D.; Bokemeyer, A.; Baker, M.; Mao, R.; Parker, C.E.; Nguyen, T.; Ma, C.; Panés, J.; Rimola, J.; Fletcher, J.G.; et al. Stenosis Therapy and Anti-Fibrotic Research (STAR) Consortium. Assessment of Crohn’s disease-associated small bowel strictures and fibrosis on cross-sectional imaging: A systematic review. Gut 2019, 68, 1115–1126.
- Adamina, M.; Bonovas, S.; Raine, T.; Spinelli, A.; Warusavitarne, J.; Armuzzi, A.; Bachmann, O.; Bager, P.; Biancone, L.; Bokemeyer, B.; et al. ECCO Guidelines on Therapeutics in Crohn’s Disease: Surgical Treatment. J. Crohn’s Colitis 2020, 14, 155–168.
- Wilkens, R.; Hagemann-Madsen, R.H.; Peters, D.A.; Nielsen, A.H.; Nørager, C.B.; Glerup, H.; Krogh, K. Validity of contrast-enhanced ultrasonography and dynamic contrast-enhanced MR enterography in the assessment of transmural activity and fibrosis in Crohn’s disease. J. Crohn’s Colitis 2018, 12, 48–56.
- Baumgart, D.C.; Müller, H.P.; Grittner, U.; Metzke, D.; Fischer, A.; Guckelberger, O.; Pascher, A.; Sack, I.; Vieth, M.; Rudolph, B. US-based Real-time Elastography for the Detection of Fibrotic Gut Tissue in Patients with Stricturing Crohn Disease. Radiology 2015, 275, 889–899.
- Sasaki, T.; Kunisaki, R.; Kinoshita, H.; Kimura, H.; Kodera, T.; Nozawa, A.; Hanzawa, A.; Shibata, N.; Yonezawa, H.; Miyajima, E.; et al. Doppler ultrasound findings correlate with tissue vascularity and inflammation in surgical pathology specimens from patients with small intestinal Crohn’s disease. BMC Res. Notes 2014, 7, 363.
- Ripollés, T.; Martínez-Pérez, M.J.; Paredes, J.M.; Vizuete, J.; García-Martínez, E.; Jiménez-Restrepo, D.H. Contrast-enhanced ultrasound in the differentiation between phlegmon and abscess in Crohn’s disease and other abdominal conditions. Eur. J. Radiol. 2013, 82, e525–e531.
- Panés, J.; Bouzas, R.; Chaparro, M.; García-Sánchez, V.; Gisbert, J.P.; De Guereñu, B.M.; Mendoza, J.L.; Paredes, J.M.; Quiroga, S.; Ripollés, T.; et al. Systematic review: The use of ultrasonography, computed tomography and magnetic resonance imaging for the diagnosis, assessment of activity and abdominal complications of Crohn’s disease. Aliment. Pharmacol. Ther. 2011, 34, 125–145.
- Nuernberg, D.; Saftoiu, A.; Barreiros, A.P.; Burmester, E.; Ivan, E.T.; Clevert, D.A.; Dietrich, C.F.; Gilja, O.H.; Lorentzen, T.; Maconi, G.; et al. EFSUMB recommendations for gastrointestinal ultrasound part 3: Endorectal, endoanal and perineal ultrasound. Ultrasound Int. Open 2019, 5, E34–E51.
- Maconi, G.; Ardizzone, S.; Greco, S.; Radice, E.; Bezzio, C.; Porro, G.B. Transperineal ultrasound in the detection of perianal and rectovaginal fistulae in Crohn’s disease. Am. J. Gastroenterol. 2007, 102, 2214–2219.
- Lavazza, A.; Maconi, G. Transperineal ultrasound for assessment of fistulas and abscesses: A pictorial essay. J. Ultrasound 2019, 22, 241–249.
- Parks, A.G.; Gordon, P.H.; Hardcastle, J.D. A classification of fistula-in-ano. BJS 1976, 63, 1–12.
- Mallouhi, A.; Bonatti, H.; Peer, S.; Lugger, P.; Conrad, F.; Bodner, G. Detection and characterization of perianal inflammatory disease: Accuracy of transperineal combined gray scale and color Doppler sonography. J. Ultrasound Med. 2004, 23, 19–27.
- Maconi, G.; Greco, M.T.; Asthana, A.K. Transperineal Ultrasound for Perianal Fistulas and Abscesses-A Systematic Review and Meta-Analysis. Ultraschall Med. Eur. J. Ultrasound 2017, 38, 265–272.




