
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Diletta Cozzi | + 1516 word(s) | 1516 | 2021-06-22 10:32:15 |
Video Upload Options
Viral pneumonia is one the most frequent respiratory diseases among very young people and the elderly, contributing to an increase in the number of hospitalizations and deaths, mainly in subjects over 60 years of age. To assess the presence of pulmonary involvement and extension of disease, diagnostic imaging techniques are traditional chest radiographs (CXR) and computed tomography (CT). CXR may show a negative radiological pattern or otherwise areas of monolateral or bilateral consolidations, in association with nodular opacities, bronchial wall thickening, and small pleural effusions.
1. Introduction
|
Virus |
Chest X-ray Signs |
Chest CT Signs |
Figure in the Text |
|---|---|---|---|
|
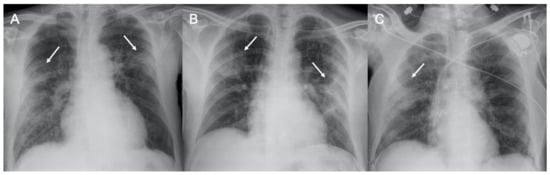
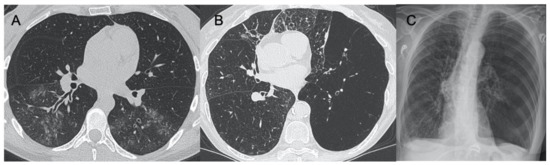
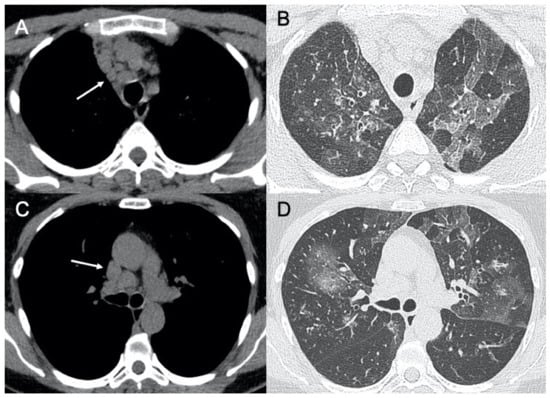
Sars-CoV-2 |
Lung subpleural consolidations, ground-glass opacities, nodules and reticular–nodular opacities, manifesting as interstitial pneumonia with diffuse alveolar damage |
In the early phase, predominantly peripheral, bilateral GGOs, in association with limited consolidations, interlobular and intralobular septal thickening creating a “crazy-paving” pattern. Air bronchograms, vascular enlargement, halo sign, and reverse halo sign are also reported |
Figure 1 and Figure 2 |
|
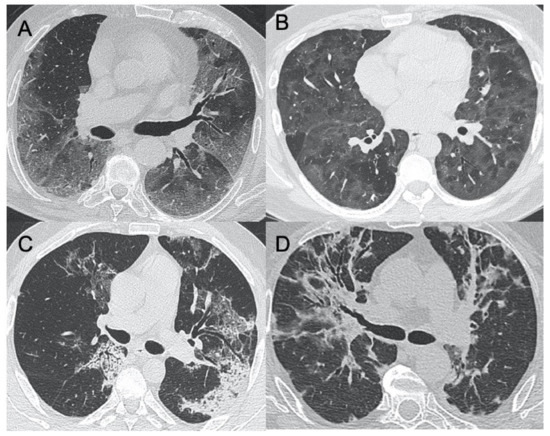
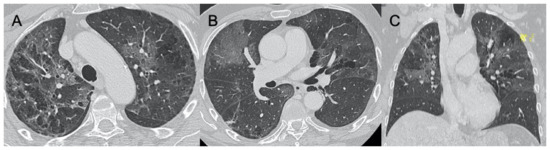
Influenza A |
Bilateral reticular-nodular opacities in association with areas of consolidation, usually in the lower lobes |
Multifocal consolidations and diffuse areas of GGO. Lymphadenopathy, cavitation, pleural effusion, and pneumatocele were also observed |
Figure 3 |
|
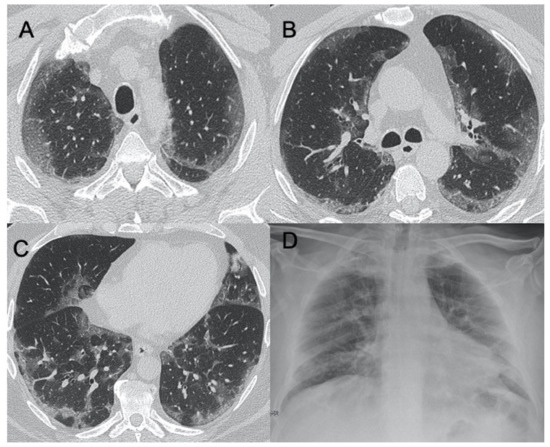
H1N1 virus |
Unilateral/bilateral GGO with or without associated areas of consolidation with predominantly peribroncho-vascular and subpleural distribution |
Unilateral or bilateral GGO with or without associated areas of consolidation with predominantly peribroncho-vascular and subpleural distribution |
Figure 4 |
|
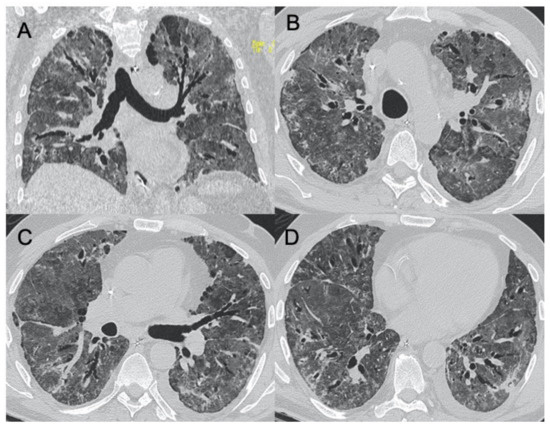
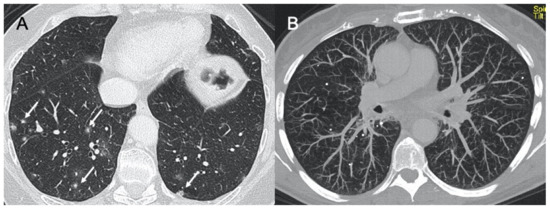
Adenovirus |
Bilateral and multifocal GGO with lobar or segmental involvement, similarly to bacterial pneumonia. In case of complication, unilateral small lung with hyperlucency and air trapping on expiration (Swyer–James Syndrome) |
Bilateral and multifocal GGO with lobar or segmental involvement, similarly to bacterial pneumonia |
Figure 5 |
|
Herpes virus |
Bilateral areas of consolidation with GGO with lobular, segmental, or sub-segmental distribution |
Multifocal areas of segmental or sub-segmental GGO are observed; pleural effusion is frequent |
Figure 6 |
|
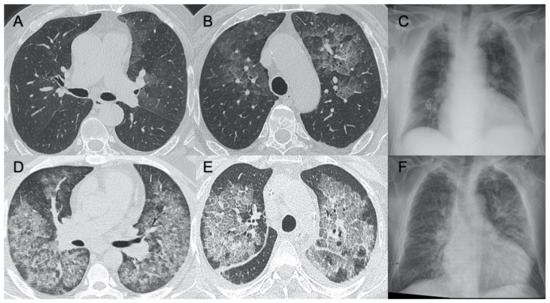
Varicella Zoster |
Multiple nodules (5–10 mm) with defined margins that may tend to confluence. Pleural effusion and lymphadenopathy may be present although they are not common |
Well-defined nodules (1–10 mm) with a halo of GGO. These millimetric lesions may calcify. |
Figure 7 |
|
Cytomegalovirus |
Diffuse and bilateral consolidations with interstitial involvement. |
Interstitial and alveolar infiltrates, bilateral and asymmetric GGO areas in association with areas of parenchymal consolidation |
Figure 8 |
|
Epstein-Barr virus |
Lymphadenopathies with smooth interstitial parenchymal involvement in both lungs |
Lymphadenopathies and less frequently interstitial infiltrates with diffuse GGOs and consolidations |
Figure 9 |
2. Lower Respiratory Tract Viral Infections in Immunocompetent
3. Lower Respiratory Tract Viral Infections in Immunocompromised
4. Conclusions
References
- Falsey, A.R.; Walsh, E.E. Viral Pneumonia in Older Adults. Clin. Infect. Dis. 2006, 42, 518–524.
- Jain, S. Epidemiology of Viral Pneumonia. Clin. Chest Med. 2017, 38, 1–9.
- Reynolds, J.H.; McDonald, G.; Alton, H.; Gordon, S.B. Pneumonia in the immunocompetent patient. Br. J. Radiol. 2010, 83, 998–1009.
- Vigil, K.J.; Adachi, J.A.; Chemaly, R.F. Analytic Review: Viral Pneumonias in Immunocompromised Adult Hosts. J. Intensive Care Med. 2010, 25, 307–326.
- Azoulay, E.; the Nine-i Investigators; Russell, L.; Van De Louw, A.; Metaxa, V.; Bauer, P.; Povoa, P.; Montero, J.G.; Loeches, I.M.; Mehta, S.; et al. Diagnosis of severe respiratory infections in immunocompromised patients. Intensive Care Med. 2020, 46, 298–314.
- Azoulay, E.; Mokart, D.; Kouatchet, A.; Demoule, A.; Lemiale, V. Acute respiratory failure in immunocompromised adults. Lancet Respir. Med. 2019, 7, 173–186.
- Seemungal, T.; Harper-Owen, R.; Bhowmik, A.; Moric, I.; Sanderson, G.; Message, S.; Maccallum, P.; Meade, T.W.; Jeffries, D.J.; Johnston, S.; et al. Respiratory Viruses, Symptoms, and Inflammatory Markers in Acute Exacerbations and Stable Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 2001, 164, 1618–1623.
- Sullivan, C.J.; Jordan, M.C. Diagnosis of viral pneumonia. Semin. Respir. Infect. 1988, 3, 148–161.
- Couch, R.B.; Englund, J.A. Respiratory Viral Infections in Immunocompetent and Immunocompromised Persons. Am. J. Med. 1997, 102, 2–9.
- Koo, H.J.; Lim, S.; Choe, J.; Choi, S.-H.; Sung, H.; Do, K.-H. Radiographic and CT Features of Viral Pneumonia. Radiographies 2018, 38, 719–739.
- Talbot, H.K.; Falsey, A.R. The Diagnosis of Viral Respiratory Disease in Older Adults. Clin. Infect. Dis. 2010, 50, 747–751.
- Franquet, T. Imaging of Pulmonary Viral Pneumonia. Radiology 2011, 260, 18–39.
- ACR Recommendations for the Use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection. American College of Radiology. Available online: (accessed on 22 March 2020).
- COVID-19 SIUMB INFORMS. Available online: (accessed on 23 April 2020).
- Giovagnoni, A. Facing the COVID-19 emergency: We can and we do. Radiol. Med. 2020, 125, 337–338.
- Choi, H.; Qi, X.; Yoon, S.H.; Park, S.J.; Lee, K.H.; Kim, J.Y.; Lee, Y.K.; Ko, H.; Kim, K.H.; Park, C.M.; et al. Extension of Coronavirus Disease 2019 on Chest CT and Implications for Chest Radiographic Interpretation. Radiol. Cardiothorac. Imaging 2020, 2, e200107.




