
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Ioannis Zabetakis | + 5362 word(s) | 5362 | 2021-07-01 05:50:24 | | | |
| 2 | Peter Tang | Meta information modification | 5362 | 2021-07-02 03:58:58 | | |
Video Upload Options
Cardiovascular diseases (CVD) remain a major cause of death and morbidity globally and diet plays a crucial role in the disease prevention and pathology. The negative perception of dairy fats stems from the effort to reduce dietary saturated fatty acid (SFA) intake due to their association with increased cholesterol levels upon consumption and the increased risk of CVD development. Recent research and meta-analyses have demonstrated the benefits of full-fat dairy consumption, based on higher bioavailability of high-value nutrients and anti-inflammatory properties.
1. Introduction
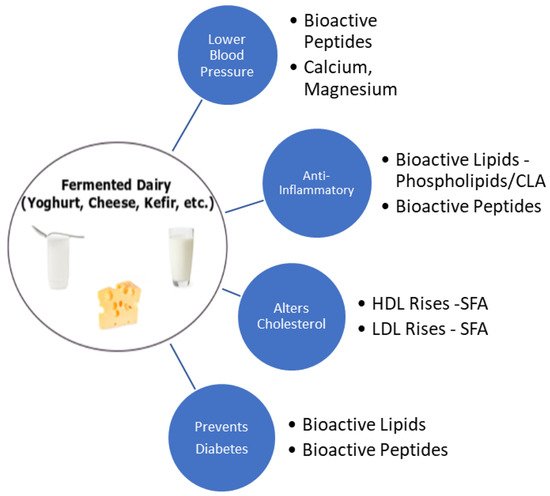
2. Dietary Guidelines and Dairy Product Consumption
3. Saturated Fat, Cholesterol and Dairy Products
4. Dairy Products and Cardiometabolic Health
5. Anti-Inflammatory Properties of Dairy Products
|
Author, Year |
Country |
Study Design |
Study Focus |
Outcome |
Conclusion |
|---|---|---|---|---|---|
|
Thompson, 2005 [54] |
USA |
Dietary intervention |
The effects of high-dairy and high-fibre consumption on weight loss in 90 obese subjects was assessed |
CRP was reduced by 0.8 mg/L from baseline (p < 0.0001), however there was no significant difference between the dairy diet and the others tested |
An insignificant reduction of CRP was observed following dairy consumption in obese participants |
|
Sofi, 2010 [55] |
Italy |
Dietary intervention |
Effect of pecorino cheese naturally enriched with cis-9, trans-11 CLA on inflammatory markers in 10 healthy participants |
Reduction in arachidonic acid-induced platelet aggregation (pre: 87.8 ± 1.76% vs. post: 77.7 ± 3.56%; p = 0.04), improvement of erythrocyte filtration rate and a reduction of TNF-α (40.1%), IL-6 (43.2%) and IL-8 (36.5%) |
Dietary short-term intake of pecorino cheese rich in cis-9, trans-11 CLA caused favourable biochemical changes of inflammatory and atherosclerotic markers |
|
Rosado, 2011 [56] |
Mexico |
Dietary intervention |
Effect of adding low-fat milk on anthropometrics, body composition, CRP etc. in energy restricted diets in 139 women |
Change in CRP after low-fat milk was 0.2 mg/L (95% CI 1.1–1.6) |
Dairy intake had no significant effect on CRP concentrations |
|
Stancliffe, 2011 [53] |
USA |
Dietary intervention |
Effects of an adequate full-fat dairy diet versus low-dairy (both mainly milk and yoghurt) intake on inflammatory markers in 40 overweight individuals with metabolic syndrome over a 12-week period versus a low-fat control |
After 7 days, the adequate full-fat dairy diet decreased plasma malondialdehyde and oxidised LDL (35% and 11% respectively, p < 0.01), TNF-α decreased by 35% (p < 0.05), which further decreased by week 12. By week 12, decreases in IL-6 (21%, p < 0.02) and MCP-1 (24%, p < 0.05) were observed. Low-dairy intake exerted no effects on oxidative or inflammatory markers |
An increase in dairy intake attenuates oxidative and inflammatory stress in metabolic syndrome |
|
Nestel, 2012 [57] |
Australia |
Dietary intervention |
Assessing the effects of low-fat or fermented dairy product intake on inflammation and atherogenesis on 13 overweight participants, using 5-single meal tests |
No significant changes in the levels of inflammatory biomarkers (CRP, IL-6, IL-13, TNF-α, VCAM-1 and others) were observed |
Authors could not confirm the reported increments in inflammation after high fat meals |
|
Esmaillzadeh, 2010 [58] |
Iran |
Cross-sectional |
Assessing the effect of dairy products on inflammatory markers in 486 women |
Low-fat dairy was inversely associated with CRP (β = −0.04), IL-6 (β = −0.02) and VCAM-1 (β = −0.06); high fat dairy was positively associated with log-transformed values of serum amyloid A (β = 0.08) and VCAM-1 (β = 0.05) |
Evidence suggests there is an independent relationship between dairy consumption and some markers of inflammation and endothelial dysfunction |
|
Panagiotakis, 2010 [59] |
Greece |
Cross-sectional |
The evaluation of effects of dairy product consumption on levels of inflammatory markers in blood samples from fasting adults with no evidence of previous chronic inflammatory disease |
Levels of inflammatory markers such as CRP, IL-6 and TNF-α were 29, 9 and 20% lower, respectively (p = 0.01), in people who consumed more than 14 servings of dairy per week compared with those who had fewer than 8 servings per week (p = 0.05) |
This inverse association between dairy consumption and levels of inflammatory markers in healthy adults indicates that dairy products may be protective against chronic inflammatory diseases |
|
Wang, 2011 [60] |
USA |
Cross-sectional |
305 adolescents were tested for serum phospholipid fatty acid markers of dairy intake (C15:0 & C17:0), which were linked to biomarkers of inflammation by generalised linear regression analyses adjusted for age, gender, race, tanner score, total energy intake and physical activity |
Phospholipid dairy fatty acids, elevated by dairy consumption, were inversely associated with CRP, 8-iso-PGF2α and urinary 15-keto-dihydro-PGF2α in overweight but not in normal weight adolescents (all pinteraction < 0.05). However, higher PL dairy fatty acid levels were associated with lower IL-6 among all adolescents. Adjustment for dietary intake of calcium, vitamin D, protein, total flavonoids and ω-3 fatty acids did not alter the findings |
Dairy-specific saturated fats C15:0 and 17:0 fatty acids, may contribute to the potential health benefits of dairy products, especially for overweight adolescents |
|
Gadotti, 2017 [61] |
Brazil |
Cross-sectional |
To assess the effect of dairy consumption and plasma inflammatory markers in 259 participants. Subjects were assigned groups depending on inflammatory status and multiple logistic regression tests were conducted to estimate the odds ratio (OR) for the inflammatory cluster across tertiles of dairy consumption |
The highest tertile of yoghurt consumption was 0.34 [95% CI: (0.14–0.81)] relative to the reference tertile, demonstrating a linear effect (ptrend = 0.015). Cheese consumption exhibited an OR of 2.49 (95% CI: (1.09–5.75)) relative to the reference |
Increasing yoghurt consumption might have a protective effect on inflammation, while cheese consumption seems to be associated with a pro-inflammatory status |
|
van Meijl, 2010 [62] |
Netherlands |
Randomised crossover |
Effects of low-fat milk and yoghurt intake on inflammatory markers in 35 overweight or obese participants versus carbohydrate controls for 8 weeks |
No significant effects on IL-6, MCP-1, ICAM-1 or VCAM-1 versus control. TNF-α index decreased by 53 (p = 0.015) |
Low-fat dairy consumption may increase concentrations of s-TNFR but it has no effects on other inflammatory markers of chronic inflammation and endothelial function |
|
Zemel, 2010 [63] |
USA |
Randomised crossover |
Effects of a dairy-rich, high calcium diet on oxidative and inflammatory stress in 10 overweight and 10 obese individuals compared with soy supplemented eucaloric diets |
After 7 days, dairy intake decreased oxidative stress by lowering 8-isoprostane-F2α (12%, p < 0.0005), plasma malondialdehyde (22%, p < 0.0005). Adiponectin increased significantly (20%, p < 0.002). Inflammatory markers were significantly reduced versus the control diet: IL-6 (13%, p < 0.01); TNF-α (15%, p < 0.002); MCP-1 (10%, p < 0.0006) |
An increase in dairy food intake produces significant and substantial suppression of the oxidative and inflammatory stress associated with overweight and obesity |
|
Nestel, 2013 [64] |
Australia |
Randomised crossover |
Consumption of full-fat versus low-fat dairy on biomarkers of inflammation in 12 overweigh individuals |
75% of those who consumed low-fat products versus full-fat fermented products tended to have higher levels of inflammatory markers tested (CRP, IL-13, TNF-α, VCAM-1 and others; ptrend < 0.001) |
Short-term diets of low-fat dairy products did not lead to a favourable biomarker profile associated with CVD risk compared with the full-fat dairy products. Full-fat fermented dairy products are more favourable |
|
Labonté, 2014 [65] |
Canada |
Randomised crossover |
Assessing the impact of dairy intake versus energy equivalent products on inflammatory markers in 112 healthy participants with systemic inflammation |
After dairy consumption, no significant changes in CRP (7.3%, p = 0.47). However, both the control and dairy diet reduced IL-6 (17.6% and 19.9%, respectively; p < 0.0001 for both, p = 0.77 for between-diet comparison |
Short-term consumption of a combination of low- and high-fat dairy products as part of a healthy diet has no adverse effects on inflammation |
|
Dugan, 2016 [66] |
USA |
Randomised crossover |
Effect of low-fat dairy consumption on hepatic enzymes and inflammation in 37 participants with metabolic syndrome versus a carbohydrate control |
Lower levels of TNF-α (p = 0.028) and MCP-1 (p = 0.001) were observed in women after low-fat dairy intake versus the control group. The hepatic steatosis index was also reduced (p = 0.001) |
Three servings of dairy per day improved both liver function and systemic inflammation in subjects with metabolic syndrome |
|
Zemel, 2008 [67] |
USA |
Randomised controlled longitudinal |
Evaluation of feeding calcium rich high-dairy eucaloric diet and hypocaloric diet versus low dairy group intake in obese participants over 24 weeks |
High-dairy eucaloric diet and a hypocaloric diet resulted in an 11% (p < 0.03) and 29% (p < 0.01) decrease in CRP, respectively (post-test vs. pre-test), whereas there was no significant change in the low-dairy groups. Adiponectin decreased by 8% in subjects fed the eucaloric high-dairy diet (p = 0.003) and 18% for the hypocaloric high-dairy diet (p = 0.05) |
Dietary calcium suppresses adipose tissue oxidative and inflammatory stress |
|
de Aguilar-Nascimento, 2011 [68] |
Brazil |
Randomised controlled longitudinal |
Effects of an early enteral formula on the levels of glutathione and inflammatory markers in 25 aged patients with acute ischemic stroke. Group 1 consumed whey, group 2, the control consumed casein |
Mortality was similar between groups (33%; p = 1.00) and was associated with higher IL-6 levels (group 1: 73.7 ± 24.7; versus group 2: 16.6 ± 2.4 pg/dL; p = 0.04) and CRP (82.0 ± 35.6 vs. 48.3 ± 14.5 mg/L; p = 0.02). Serum IL-6 was lower (p = 0.03) and glutathione was higher (p = 0.03) in whey protein-fed patients versus the casein group |
Enteral formula containing whey protein may decrease inflammation and increase antioxidant defences in elderly patients with ischemic stroke |
|
Jones, 2013 [69] |
Canada |
Randomised controlled longitudinal |
Assessing a diet rich in calcium and dairy products on weight loss and appetite during energy restriction in 49 overweight and obese individuals for 12 weeks, versus a suitable control. A meal tolerance test was carried out in week 12 |
MCP-1 was reduced after 30 mins with Dairy/Calcium group compared with the control in the meal tolerance test (p = 0.04). No change was observed for IL-6, TNF-α, or IL-1β |
Modest reduction in MCP-1 |
|
Pei, 2017 [70] |
USA |
Randomised controlled |
Premenopausal women (BMI 18.5–27 and 30–40 kg/m2) were randomised to consume 339 g of low-fat yoghurt (yoghurt non-obese (YN); yoghurt obese (YO)) or 324 g of soya pudding (control non-obese; control obese (CO)) daily for 9 weeks (n 30/group). Fasting blood samples were analysed for various inflammatory markers |
After 9-week yoghurt consumption, YO and YN had decreased TNF-α/sTNFR RII. Yoghurt consumption increased plasma IgM EndoCAb regardless of obesity status. sCD14 was not affected by diet but LBP/sCD14 was lowered in both YN and YO. Yoghurt intervention increased plasma 2-arachidonoylglycerol in YO but not YN. YO peripheral blood mononuclear cells expression of NF-κB inhibitor α and transforming growth factor β1 increased relative to CO at 9 weeks |
Consumption of low-fat yoghurt for 9 weeks reduced biomarkers of chronic inflammation and endotoxin exposure in premenopausal women compared with a non-dairy control food |
|
Wannamethee, 2018 [71] |
UK |
Prospective cohort study |
This study investigated serum CLA (measured as a % of total fatty acids) and the risk of incident heart failure in 3806 older men aged between 60 and 79 years using metabolomics. The men were without prevalent HF and were followed up for an average of 13 years, during which there were 295 incident HF cases |
CLA was adversely associated with cholesterol levels but was inversely associated with CRP and NT-proBNP. No association between CLA and CHD. High CLA was associated with reduced risk of HF (hazard ratio [95% confidence interval], 0.64 [0.43–0.96]; quartile 4 versus quartile 1). Elevated CLA was associated with reduced HF risk only in those with higher dairy fat intake, a major dietary source of CLA (p = 0.03) |
The reduced risk of HF was partially explained by NT-proBNP. High dairy fat intake was not associated with incident coronary heart disease but was associated with reduced risk of HF, largely because of the inverse effect of CLA |
BMI = body mass index; CHD = coronary heart disease; CI = confidence interval; CLA = conjugated linoleic acid; CRP = C-reactive protein; EndoCab = endogenous endotoxin-core antibody; HF = heart failure; IL-X = interleukin-β/6/13 etc.; MCP-1 = monocyte chemoattractant protein-1; NF-κB = nuclear factor-κB; NT-proBNP = N-terminal prohormone of brain natriuretic peptide; s-CD14 = soluble cluster of differentiation 14; s-TNFR = soluble tumour necrosis factor receptors; TNF-α = tumour necrosis factor-α; VCAM-1 = vascular cell adhesion molecule-1.
6. Trans Fatty Acids
7. Fermented Dairy Products and Cardiovascular Health
References
- Wilkins, E.; Wilson, L.; Wickramasinghe, K.; Bhatnagar, P.; Leal, J.; Luengo-Fernandez, R.; Burns, R.; Rayner, M.; Townsend, N. European Cardiovascular Disease Statistics 2017; European Heart Network: Brussels, Belgium, 2017.
- Benjamin, E.J.; Blaha, M.J.; Chiuve, S.E.; Cushman, M.; Das, S.R.; Deo, R.; de Ferranti, S.D.; Floyd, J.; Fornage, M.; Gillespie, C.; et al. Heart disease and stroke statistics—2017 update: A report from the american heart association. Circulation 2017, 135, e146–e603.
- Health Service Executive Ireland. Coronary Heart Disease. Available online: (accessed on 20 January 2017).
- Lordan, R.; Zabetakis, I. Invited review: The anti-inflammatory properties of dairy lipids. J. Dairy Sci. 2017, 100, 4197–4212.
- O’Keefe, J.H.; Gheewala, N.M.; O’Keefe, J.O. Dietary strategies for improving post-prandial glucose, lipids, inflammation, and cardiovascular health. J. Am. Coll. Cardiol. 2008, 51, 249–255.
- Mozaffarian, D.; Appel, L.J.; Van Horn, L. Components of a cardioprotective diet new insights. Circulation 2011, 123, 2870–2891.
- Kapaj, A.; Deci, E. Chapter 7—World milk production and socio-economic factors effecting its consumption a2—Watson, ronald ross. In Dairy in Human Health and Disease Across the Lifespan; Collier, R.J., Preedy, V.R., Eds.; Academic Press: Cambridge, MA, USA, 2017; pp. 107–115.
- Artaud-Wild, S.M.; Connor, S.; Sexton, G.; Connor, W.E. Differences in coronary mortality can be explained by differences in cholesterol and saturated fat intakes in 40 countries but not in France and Finland. A paradox. Circulation 1993, 88, 2771–2779.
- Turpeinen, O. Effect of cholesterol-lowering diet on mortality from coronary heart disease and other causes. Circulation 1979, 59, 1–7.
- Huth, P.J.; Park, K.M. Influence of dairy product and milk fat consumption on cardiovascular disease risk: A review of the evidence. Adv. Nutr. 2012, 3, 266–285.
- Grosso, G. Chapter 30—Milk and chronic-degenerative diseases: Main components and potential mechanisms a2—Watson, ronald ross. In Dairy in Human Health and Disease Across the Lifespan; Collier, R.J., Preedy, V.R., Eds.; Academic Press: Cambridge, MA, USA, 2017; pp. 385–393.
- Guo, J.; Astrup, A.; Lovegrove, J.A.; Gijsbers, L.; Givens, D.I.; Soedamah-Muthu, S.S. Milk and dairy consumption and risk of cardiovascular diseases and all-cause mortality: Dose-response meta-analysis of prospective cohort studies. Eur. J. Epidemiol. 2017, 32, 269–287.
- Goldbohm, R.A.; Chorus, A.M.J.; Garre, F.G.; Schouten, L.J.; van den Brandt, P.A. Dairy consumption and 10-y total and cardiovascular mortality: A prospective cohort study in The Netherlands. Am. J. Clin. Nutr. 2011, 93, 615–627.
- Lamarche, B.; Givens, D.I.; Soedamah-Muthu, S.; Krauss, R.M.; Jakobsen, M.U.; Bischoff-Ferrari, H.A.; Pan, A.; Després, J.-P. Does milk consumption contribute to cardiometabolic health and overall diet quality? Can. J. Cardiol. 2016, 32, 1026–1032.
- Dumas, A.-A.; Lapointe, A.; Dugrenier, M.; Provencher, V.; Lamarche, B.; Desroches, S. A systematic review of the effect of yogurt consumption on chronic diseases risk markers in adults. Eur. J. Clin. Nutr. 2017, 56, 1375–1392.
- Alexander, D.D.; Bylsma, L.C.; Vargas, A.J.; Cohen, S.S.; Doucette, A.; Mohamed, M.; Irvin, S.R.; Miller, P.E.; Watson, H.; Fryzek, J.P. Dairy consumption and CVD: A systematic review and meta-analysis. Br. J. Nutr. 2016, 115, 737–750.
- Qin, L.-Q.; Xu, J.-Y.; Han, S.-F.; Zhang, Z.-L.; Zhao, Y.-Y.; Szeto, I.M. Dairy consumption and risk of cardiovascular disease: An updated meta-analysis of prospective cohort studies. Asia Pac. J. Clin. Nutr. 2015, 24, 90–100.
- Crichton, G.E.; Elias, M.F. Dairy food intake and cardiovascular health: The maine-syracuse study. Adv. Dairy Res. 2014, 2, 1–8.
- Crichton, G.E.; Alkerwi, A. Dairy food intake is positively associated with cardiovascular health: Findings from observation of cardiovascular risk factors in Luxembourg study. Nutr. Res. 2014, 34, 1036–1044.
- Gijsbers, L.; Ding, E.L.; Malik, V.S.; de Goede, J.; Geleijnse, J.M.; Soedamah-Muthu, S.S. Consumption of dairy foods and diabetes incidence: A dose-response meta-analysis of observational studies. Am. J. Clin. Nutr. 2016, 103, 1111–1124.
- Lu, L.; Xun, P.; Wan, Y.; He, K.; Cai, W. Long-term association between dairy consumption and risk of childhood obesity: A systematic review and meta-analysis of prospective cohort studies. Eur. J. Clin. Nutr. 2016, 70, 414–423.
- Crichton, G.E.; Alkerwi, A. Whole-fat dairy food intake is inversely associated with obesity prevalence: Findings from the observation of cardiovascular risk factors in Luxembourg study. Nutr. Res. 2014, 34, 936–943.
- Lee, K.; Cho, W. The consumption of dairy products is associated with reduced risks of obesity and metabolic syndrome in Korean women but not in men. Nutrients 2017, 9, 630.
- Chen, G.C.; Szeto, I.; Chen, L.; Han, S.; Li, Y.; van Hekezen, R.; Qin, L. Dairy products consumption and metabolic syndrome in adults: Systematic review and meta-analysis of observational studies. Sci. Rep. 2015, 5, 14606.
- Liu, A.G.; Ford, N.A.; Hu, F.B.; Zelman, K.M.; Mozaffarian, D.; Kris-Etherton, P.M. A healthy approach to dietary fats: Understanding the science and taking action to reduce consumer confusion. Nutr. J. 2017, 16, 53.
- Rousseau, S. The celebrity quick-fix. Food Cult. Soc. 2015, 18, 265–287.
- United States Department of Health and Human Services. Dietary Guidelines for Americans 2015–2020; Skyhorse Publishing Inc.: New York, NY, USA, 2017.
- Health Service Executive Ireland. Healthy Food for Life Guidelines. Available online: (accessed on 17 January 2018).
- Weaver, C.M. How sound is the science behind the dietary recommendations for dairy? Am. J. Clin. Nutr. 2014, 99, 1217S–1222S.
- Bantle, J.P.; Wylie-Rosett, J.; Albright, A.L.; Apovian, C.M.; Clark, N.G.; Franz, M.J.; Hoogwerf, B.J.; Lichtenstein, A.H.; Mayer-Davis, E.; Mooradian, A.D. Nutrition recommendations and interventions for diabetes: A position statement of the American Diabetes Association. Diabetes Care 2008, 31, S61–S78.
- Benatar, J.R. Chapter 20—Does dairy food have effects on cardiovascular disease and cardiometabolic risk? A2—Watson, ronald ross. In Dairy in Human Health and Disease Across the Lifespan; Collier, R.J., Preedy, V.R., Eds.; Academic Press: Cambridge, MA, USA, 2017; pp. 263–271.
- Harvard School of Public Health. Healthy Eating Plate and Healthy Eating Pyramid. Available online: (accessed on 21 January 2018).
- National Health and Medical Research Council. Australian Dietary Guidelines Ageing; Department of Health and Ageing, Ed.; National Health and Medical Research Council Canberra: Canberra, Australia, 2013.
- Markey, O.; Vasilopoulou, D.; Givens, D.I.; Lovegrove, J.A. Dairy and cardiovascular health: Friend or foe? Nutr. Bull. 2014, 39, 161–171.
- Wade, A.T.; Davis, C.R.; Dyer, K.A.; Hodgson, J.M.; Woodman, R.J.; Keage, H.A.; Murphy, K.J. A mediterranean diet to improve cardiovascular and cognitive health: Protocol for a randomised controlled intervention study. Nutrients 2017, 9, 145.
- Van Ballegooijen, A.J.; Beulens, J.W. The role of vitamin K status in cardiovascular health: Evidence from observational and clinical studies. Curr. Nutr. Rep. 2017, 6, 197–205.
- Heaney, R.P. Calcium, dairy products and osteoporosis. J. Am. Coll. Nutr. 2000, 19, 83S–99S.
- Edem, D.O. Palm oil: Biochemical, physiological, nutritional, hematological and toxicological aspects: A review. Plant Foods Hum. Nutr. 2002, 57, 319–341.
- Mukherjee, S.; Mitra, A. Health effects of palm oil. J. Hum. Ecol. 2009, 26, 197–203.
- Pehowich, D.J.; Gomes, A.V.; Barnes, J.A. Fatty acid composition and possible health effects of coconut constituents. West Indian Med. J. 2000, 49, 128–133.
- Guarner, V.; Rubio-Ruiz, M.E. Low-grade systemic inflammation connects aging, metabolic syndrome and cardiovascular disease. In Aging and Health—A Systems Biology Perspective; Karger Publishers: Basel, Switzerland, 2014; Volume 40, pp. 99–106.
- Vishnu, A.; Gurka, M.J.; DeBoer, M.D. The severity of the metabolic syndrome increases over time within individuals, independent of baseline metabolic syndrome status and medication use: The atherosclerosis risk in communities study. Atherosclerosis 2015, 243, 278–285.
- Lordan, R.; Tsoupras, A.; Zabetakis, I. Phospholipids of animal and marine origin: Structure, function, and anti-inflammatory properties. Molecules 2017, 22, 1964.
- Da Silva, M.S.; Rudkowska, I. Dairy nutrients and their effect on inflammatory profile in molecular studies. Mol. Nutr. Food Res. 2015, 59, 1249–1263.
- Palur Ramakrishnan, A.V.K.; Varghese, T.P.; Vanapalli, S.; Nair, N.K.; Mingate, M.D. Platelet activating factor: A potential biomarker in acute coronary syndrome? Cardiovasc. Ther. 2017, 35, 64–70.
- Castro Faria Neto, H.C.; Stafforini, D.M.; Prescott, S.M.; Zimmerman, G.A. Regulating inflammation through the anti-inflammatory enzyme platelet-activating factor-acetylhydrolase. Mem. Inst. Oswaldo Cruz 2005, 100, 83–91.
- Lordan, R.; Zabetakis, I. Ovine and caprine lipids promoting cardiovascular health in milk and its derivatives. Adv. Dairy Res 2017, 5.
- Antonopoulou, S.; Semidalas, C.E.; Koussissis, S.; Demopoulos, C.A. Platelet-activating factor (PAF) antagonists in foods: A study of lipids with PAF or anti-PAF-like activity in cow’s milk and yogurt. J. Agric. Food Chem. 1996, 44, 3047–3051.
- Poutzalis, S.; Anastasiadou, A.; Nasopoulou, C.; Megalemou, K.; Sioriki, E.; Zabetakis, I. Evaluation of the in vitro anti-atherogenic activities of goat milk and goat dairy products. Dairy Sci. Technol. 2016, 96, 317–327.
- Tsorotioti, S.E.; Nasopoulou, C.; Detopoulou, M.; Sioriki, E.; Demopoulos, C.A.; Zabetakis, I. In vitro anti-atherogenic properties of traditional Greek cheese lipid fractions. Dairy Sci. Technol. 2014, 94, 269–281.
- Megalemou, K.; Sioriki, E.; Lordan, R.; Dermiki, M.; Nasopoulou, C.; Zabetakis, I. Evaluation of sensory and in vitro anti-thrombotic properties of traditional Greek yogurts derived from different types of milk. Heliyon 2017, 3, e00227.
- Da Silva, M.S.; Rudkowska, I. Chapter 22—Macro components in dairy and their effects on inflammation parameters: Preclinical studies a2—Watson, ronald ross. In Nutrients in Dairy and Their Implications on Health and Disease; Collier, R.J., Preedy, V.R., Eds.; Academic Press: Cambridge, MA, USA, 2017; pp. 287–302.
- Stancliffe, R.A.; Thorpe, T.; Zemel, M.B. Dairy attentuates oxidative and inflammatory stress in metabolic syndrome. Am. J. Clin. Nutr. 2011, 94, 422–430.
- Thompson, W.G.; Holdman, N.R.; Janzow, D.J.; Slezak, J.M.; Morris, K.L.; Zemel, M.B. Effect of energy-reduced diets high in dairy products and fiber on weight loss in obese adults. Obes. Res. 2005, 13, 1344–1353.
- Sofi, F.; Buccioni, A.; Cesari, F.; Gori, A.M.; Minieri, S.; Mannini, L.; Casini, A.; Gensini, G.F.; Abbate, R.; Antongiovanni, M. Effects of a dairy product (pecorino cheese) naturally rich in cis-9, trans-11 conjugated linoleic acid on lipid, inflammatory and haemorheological variables: A dietary intervention study. Nutr. Metab. Cardiovasc. Dis. 2010, 20, 117–124.
- Rosado, J.L.; Garcia, O.P.; Ronquillo, D.; Hervert-Hernández, D.; Caamaño, M.D.C.; Martínez, G.; Gutiérrez, J.; García, S. Intake of milk with added micronutrients increases the effectiveness of an energy-restricted diet to reduce body weight: A randomized controlled clinical trial in Mexican women. J. Am. Diet. Assoc. 2011, 111, 1507–1516.
- Nestel, P.J.; Pally, S.; MacIntosh, G.L.; Greeve, M.A.; Middleton, S.; Jowett, J.; Meikle, P.J. Circulating inflammatory and atherogenic biomarkers are not increased following single meals of dairy foods. Eur. J. Clin. Nutr. 2012, 66, 25–31.
- Esmaillzadeh, A.; Azadbakht, L. Dairy consumption and circulating levels of inflammatory markers among Iranian women. Public Health Nutr. 2010, 13, 1395–1402.
- Panagiotakos, D.B.; Pitsavos, C.H.; Zampelas, A.D.; Chrysohoou, C.A.; Stefanadis, C.I. Dairy products consumption is associated with decreased levels of inflammatory markers related to cardiovascular disease in apparently healthy adults: The ATTICA study. J. Am. Coll. Nutr. 2010, 29, 357–364.
- Wang, H.; Steffen, L.M.; Vessby, B.; Basu, S.; Steinberger, J.; Moran, A.; Jacobs, D.R.; Hong, C.-P.; Sinaiko, A.R. Obesity modifies the relations between serum markers of dairy fats and inflammation and oxidative stress among adolescents. Obesity 2011, 19, 2404–2410.
- Gadotti, T.N.; Norde, M.M.; Rogero, M.M.; Fisberg, M.; Fisberg, R.M.; Oki, E.; Martini, L.A. Dairy consumption and inflammatory profile: A cross-sectional population-based study, São Paulo, Brazil. Nutrition 2017, 48, 1–5.
- Van Meijl, L.E.C.; Mensink, R.P. Effects of low-fat dairy consumption on markers of low-grade systemic inflammation and endothelial function in overweight and obese subjects: An intervention study. Br. J. Nutr. 2010, 104, 1523–1527.
- Zemel, M.B.; Sun, X.; Sobhani, T.; Wilson, B. Effects of dairy compared with soy on oxidative and inflammatory stress in overweight and obese subjects. Am. J. Clin. Nutr. 2010, 91, 16–22.
- Nestel, P.J.; Mellett, N.; Pally, S.; Wong, G.; Barlow, C.K.; Croft, K.; Mori, T.A.; Meikle, P.J. Effects of low-fat or full-fat fermented and non-fermented dairy foods on selected cardiovascular biomarkers in overweight adults. Br. J. Nutr. 2013, 110, 2242–2249.
- Labonté, M.-È.; Cyr, A.; Abdullah, M.M.; Lépine, M.-C.; Vohl, M.-C.; Jones, P.; Couture, P.; Lamarche, B. Dairy product consumption has no impact on biomarkers of inflammation among men and women with low-grade systemic inflammation. J. Nutr. 2014, 144, 1760–1767.
- Dugan, C.E.; Aguilar, D.; Park, Y.K.; Lee, J.Y.; Fernandez, M.L. Dairy consumption lowers systemic inflammation and liver enzymes in typically low-dairy consumers with clinical characteristics of metabolic syndrome. J. Am. Coll. Nutr. 2016, 35, 255–261.
- Zemel, M.B.; Sun, X. Dietary calcium and dairy products modulate oxidative and inflammatory stress in mice and humans. J. Nutr. 2008, 138, 1047–1052.
- De Aguilar-Nascimento, J.E.; Prado Silveira, B.R.; Dock-Nascimento, D.B. Early enteral nutrition with whey protein or casein in elderly patients with acute ischemic stroke: A double-blind randomized trial. Nutrition 2011, 27, 440–444.
- Jones, K.W.; Eller, L.K.; Parnell, J.A.; Doyle-Baker, P.K.; Edwards, A.L.; Reimer, R.A. Effect of a dairy-and calcium-rich diet on weight loss and appetite during energy restriction in overweight and obese adults: A randomized trial. Eur. J. Clin. Nutr. 2013, 67, 371–376.
- Pei, R.; DiMarco, D.M.; Putt, K.K.; Martin, D.A.; Gu, Q.; Chitchumroonchokchai, C.; White, H.M.; Scarlett, C.O.; Bruno, R.S.; Bolling, B.W. Low-fat yogurt consumption reduces biomarkers of chronic inflammation and inhibits markers of endotoxin exposure in healthy premenopausal women: A randomised controlled trial. Br. J. Nutr. 2017, 118, 1043–1051.
- Wannamethee, S.G.; Jefferis, B.J.; Lennon, L.; Papacosta, O.; Whincup, P.H.; Hingorani, A.D. Serum conjugated linoleic acid and risk of incident heart failure in older men: The British regional heart study. JAMA 2018, 7, e006653.
- De Souza, R.J.; Mente, A.; Maroleanu, A.; Cozma, A.I.; Ha, V.; Kishibe, T.; Uleryk, E.; Budylowski, P.; Schünemann, H.; Beyene, J.; et al. Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: Systematic review and meta-analysis of observational studies. BMJ 2015, 351, h3978.
- Poudyal, H.; Brown, L. Should the pharmacological actions of dietary fatty acids in cardiometabolic disorders be classified based on biological or chemical function? Prog. Lipid Res. 2015, 59, 172–200.
- Micha, R.; Mozaffarian, D. Trans fatty acids: Effects on cardiometabolic health and implications for policy. Prostaglandins Leukot. Essent. Fat. Acids 2008, 79, 147–152.
- Ganguly, R.; Pierce, G.N. Trans fat involvement in cardiovascular disease. Mol. Nutr. Food Res. 2012, 56, 1090–1096.
- Stone, N.J.; Robinson, J.; Lichtenstein, A.H.; Merz, C.N.B.; Blum, C.B.; Eckel, R.H.; Goldberg, A.C.; Gordon, D.; Levy, D.; Lloyd-Jones, D.M.; et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults; A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines; American College of Cardiology: Washington, DC, USA, 2013.
- Lichtenstein, A.H.; Appel, L.J.; Brands, M.; Carnethon, M.; Daniels, S.; Franch, H.A.; Franklin, B.; Kris-Etherton, P.; Harris, W.S.; Howard, B. Diet and lifestyle recommendations revision 2006. Circulation 2006, 114, 82–96.
- L’Abbé, M.R.; Stender, S.; Skeaff, C.M.; Ghafoorunissa; Tavella, M. Approaches to removing trans fats from the food supply in industrialized and developing countries. Eur. J. Clin. Nutr. 2009, 63, S50–S67.
- Dawczynski, C.; Lorkowski, S. Trans-fatty acids and cardiovascular risk: Does origin matter? Expert Rev. Cardiovasc. Ther. 2016, 14, 1001–1005.
- Mozaffarian, D.; Katan, M.B.; Ascherio, A.; Stampfer, M.J.; Willett, W.C. Trans fatty acids and cardiovascular disease. N. Engl. J. Med. 2006, 354, 1601–1613.
- Wang, Y.; Jacome-Sosa, M.M.; Proctor, S.D. The role of ruminant trans fat as a potential nutraceutical in the prevention of cardiovascular disease. Food Res. Int. 2012, 46, 460–468.
- Lichtenstein, A.H. Dietary trans fatty acids and cardiovascular disease risk: Past and present. Curr. Atheroscler. Rep. 2014, 16, 433.
- Ascherio, A.; Hennekens, C.H.; Buring, J.E.; Master, C.; Stampfer, M.J.; Willett, W.C. Trans-fatty acids intake and risk of myocardial infarction. Circulation 1994, 89, 94–101.
- Gebauer, S.K.; Chardigny, J.-M.; Jakobsen, M.U.; Lamarche, B.; Lock, A.L.; Proctor, S.D.; Baer, D.J. Effects of ruminant trans fatty acids on cardiovascular disease and cancer: A comprehensive review of epidemiological, clinical, and mechanistic studies. Adv. Nutr. 2011, 2, 332–354.
- Bassett, C.M.C.; Edel, A.L.; Patenaude, A.F.; McCullough, R.S.; Blackwood, D.P.; Chouinard, P.Y.; Paquin, P.; Lamarche, B.T.; Pierce, G.N. Dietary vaccenic acid has antiatherogenic effects in LDLr−/− mice. J. Nutr. 2010, 140, 18–24.
- Van de Vijver, L.; Kardinaal, A.; Couet, C.; Aro, A. Association between trans fatty acid intake and cardiovascular risk factors in Europe: The transfair study. Eur. J. Clin. Nutr. 2000, 54, 126–135.
- Martínez-González, M.A.; Salas-Salvadó, J.; Estruch, R.; Corella, D.; Fitó, M.; Ros, E. Benefits of the mediterranean diet: Insights from the predimed study. Prog. Cardiovasc. Dis. 2015, 58, 50–60.
- Smit, L.A.; Baylin, A.; Campos, H. Conjugated linoleic acid in adipose tissue and risk of myocardial infarction. Am. J. Clin. Nutr. 2010, 92, 34–40.
- Moloney, F.; Toomey, S.; Noone, E.; Nugent, A.; Allan, B.; Loscher, C.E.; Roche, H.M. Antidiabetic effects of cis-9, trans-11–conjugated linoleic acid may be mediated via anti-inflammatory effects in white adipose tissue. Diabetes 2007, 56, 574–582.
- Ahn, I.-S.; Choi, B.-H.; Ha, J.-H.; Byun, J.-M.; Shin, H.-G.; Park, K.-Y.; Do, M.-S. Isomer-specific effect of conjugated linoleic acid on inflammatory adipokines associated with fat accumulation in 3T3-L1 adipocytes. J. Med. Food 2006, 9, 307–312.
- Mozaffarian, D.; Cao, H.; King, I.B.; Lemaitre, R.N.; Song, X.; Siscovick, D.S.; Hotamisligil, G.K.S. Trans-palmitoleic acid, metabolic risk factors, and new-onset diabetes in us adults. Ann. Intern. Med. 2010, 153, 790–799.
- Bolton-Smith, C.; Woodward, M.; Fenton, S.; Brown, C. Does dietary trans fatty acid intake relate to the prevalence of coronary heart disease in Scotland? Eur. Heart J. 1996, 17, 837–845.
- Olmedilla-Alonso, B.; Nova-Rebato, E.; García-González, N.; Martín-Diana, A.-B.; Fontecha, J.; Delgado, D.; Gredilla, A.-E.; Bueno, F.; Asensio-Vegas, C. Effect of ewe’s (semi-skimmed and whole) and cow’s milk yogurt consumption on the lipid profile of control subjects: A crossover study. Food Nutr. Res. 2017, 61, 1391669.
- Zoumpopoulou, G.; Pot, B.; Tsakalidou, E.; Papadimitriou, K. Dairy probiotics: Beyond the role of promoting gut and immune health. Int. Dairy J. 2017, 67, 46–60.
- Beltrán-Barrientos, L.M.; Hernández-Mendoza, A.; Torres-Llanez, M.J.; González-Córdova, A.F.; Vallejo-Córdoba, B. Invited review: Fermented milk as antihypertensive functional food. J. Dairy Sci. 2016, 99, 4099–4110.
- Elwood, P.C.; Pickering, J.E.; Givens, D.I.; Gallacher, J.E. The consumption of milk and dairy foods and the incidence of vascular disease and diabetes: An overview of the evidence. Lipids 2010, 45, 925–939.
- Darmon, N.; Drewnowski, A. Does social class predict diet quality? Am. J. Clin. Nutr. 2008, 87, 1107–1117.
- Hobbs, D.A.; Givens, D.I.; Lovegrove, J.A. Yogurt consumption is associated with higher nutrient intake, diet quality and favourable metabolic profle in children: A cross-sectional analysis using data from years 1–4 of the national diet and nutrition survey, UK. Eur. J. Nutr. 2018, 1–14.
- Tognon, G.; Nilsson, L.M.; Shungin, D.; Lissner, L.; Jansson, J.-H.; Renström, F.; Wennberg, M.; Winkvist, A.; Johansson, I. Nonfermented milk and other dairy products: Associations with all-cause mortality. Am. J. Clin. Nutr. 2017, 105, 1502–1511.
- Chen, M.; Sun, Q.; Giovannucci, E.; Mozaffarian, D.; Manson, J.E.; Willett, W.C.; Hu, F.B. Dairy consumption and risk of type 2 diabetes: 3 cohorts of us adults and an updated meta-analysis. BMC Med. 2014, 12, 215.
- Sluijs, I.; Forouhi, N.G.; Beulens, J.W.J.; van der Schouw, Y.T.; Agnoli, C.; Arriola, L.; Balkau, B.; Barricarte, A.; Boeing, H.; Bueno-de-Mesquita, H.B. The amount and type of dairy product intake and incident type 2 diabetes: Results from the epic-interact study. Am. J. Clin. Nutr. 2012, 96, 382–390.
- Tong, X.; Chen, G.-C.; Zhang, Z.; Wei, Y.-L.; Xu, J.-Y.; Qin, L.-Q. Cheese consumption and risk of all-cause mortality: A meta-analysis of prospective studies. Nutrients 2017, 9, 63.
- Kießling, G.; Schneider, J.; Jahreis, G. Long-term consumption of fermented dairy products over 6 months increases HDL cholesterol. Eur. J. Clin. Nutr. 2002, 56, 843–849.
- Drouin-Chartier, J.-P.; Brassard, D.; Tessier-Grenier, M.; Côté, J.A.; Labonté, M.-È.; Desroches, S.; Couture, P.; Lamarche, B. Systematic review of the association between dairy product consumption and risk of cardiovascular-related clinical outcomes. Adv. Nutr. 2016, 7, 1026–1040.
- Turner, K.M.; Keogh, J.B.; Clifton, P.M. Dairy consumption and insulin sensitivity: A systematic review of short- and long-term intervention studies. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 3–8.
- Hove, K.D.; Brøns, C.; Færch, K.; Lund, S.S.; Rossing, P.; Vaag, A. Effects of 12 weeks of treatment with fermented milk on blood pressure, glucose metabolism and markers of cardiovascular risk in patients with type 2 diabetes: A randomised double-blind placebo-controlled study. Eur. J. Endocrinol. 2015, 172, 11–20.
- Houston, D.K.; Driver, K.E.; Bush, A.J.; Kritchevsky, S.B. The association between cheese consumption and cardiovascular risk factors among adults. J. Hum. Nutr. Diet. 2008, 21, 129–140.
- Tholstrup, T. Dairy products and cardiovascular disease. Curr. Opin. Lipidol. 2006, 17, 1–10.
- Tavani, A.; Gallus, S.; Negri, E.; La Vecchia, C. Milk, dairy products, and coronary heart disease. J. Epidemiol. Community Health 2002, 56, 471–472.
- Hjerpsted, J.; Tholstrup, T. Cheese and cardiovascular disease risk: A review of the evidence and discussion of possible mechanisms. Crit. Rev. Food Sci. Nutr. 2016, 56, 1389–1403.
- Praagman, J.; Dalmeijer, G.W.; van der Schouw, Y.T.; Soedamah-Muthu, S.S.; Monique Verschuren, W.M.; Bas Bueno-de-Mesquita, H.; Geleijnse, J.M.; Beulens, J.W.J. The relationship between fermented food intake and mortality risk in the European prospective investigation into cancer and nutrition-netherlands cohort. Br. J. Nutr. 2015, 113, 498–506.
- Wu, L.; Sun, D. Consumption of yogurt and the incident risk of cardiovascular disease: A meta-analysis of nine cohort studies. Nutrients 2017, 9, 315.
- Sayon-Orea, C.; Martínez-González, M.A.; Ruiz-Canela, M.; Bes-Rastrollo, M. Associations between yogurt consumption and weight gain and risk of obesity and metabolic syndrome: A systematic review. Adv. Nutr. 2017, 8, 146S–154S.
- Sayón-Orea, C.; Bes-Rastrollo, M.; Martí, A.; Pimenta, A.M.; Martín-Calvo, N.; Martínez-González, M.A. Association between yogurt consumption and the risk of metabolic syndrome over 6 years in the sun study. BMC Public Health 2015, 15, 170.
- Nestel, P. Chapter 16—Fermented Dairy Foods and Cardiovascular Risk a2—Watson, Ronald Ross. In Dairy in Human Health and Disease Across the Lifespan; Collier, R.J., Preedy, V.R., Eds.; Academic Press: Cambridge, MA, USA, 2017; pp. 225–229.
- Rosqvist, F.; Smedman, A.; Lindmark-Månsson, H.; Paulsson, M.; Petrus, P.; Straniero, S.; Rudling, M.; Dahlman, I.; Risérus, U. Potential role of milk fat globule membrane in modulating plasma lipoproteins, gene expression, and cholesterol metabolism in humans: A randomized study. Am. J. Clin. Nutr. 2015, 102, 20–30.




