
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Korosoglou Grigorios | + 2658 word(s) | 2658 | 2021-06-16 11:52:02 | | | |
| 2 | Lindsay Dong | Meta information modification | 2658 | 2021-06-17 03:28:30 | | |
Video Upload Options
Among all non-invasive diagnostic methods employed in the work-up of patients with chronic coronary syndromes (CCS), coronary computer tomography angiography (CCTA) stands out as an excellent integrative tool that provides information regarding calcium burden, presence and degree of coronary stenosis, type of atherosclerotic plaques, and functional relevance of such plaques, all in one examination.
1. Introduction
Coronary artery disease (CAD) remains an important cause of morbidity and mortality worldwide Currently, the term “chronic coronary syndromes” (CCS) gathers under one umbrella all patients who are affected from CAD in different forms and stages, excluding those with acute coronary syndromes (ACS) The work-up of patients with CCS is complex, beginning with the evaluation of the pre-test probability for CAD and proceeding with the selection of appropriate treatment pathways. In this regard, non-invasive stress imaging tests were shown to be excellent tools for properly selecting patients who would further benefit from an invasive procedure, thus providing both precise diagnostic classification and risk stratification [1][2].
Moreover, in the era of the ORBITA and ISCHEMIA trials, the optimal therapeutic approach for patients with significant CAD became a subject of debate, and in many situations shared decision approaches are recommended [3][4]. In this regard CCTA presents itself not only as an excellent diagnostic tool but also as an educational tool for the patient. The relatively “simple” representation of the coronary arteries provides the patient with a clear view and with the help of the physician, an understanding of the underlying anatomical problems.
2. Technical Aspects
2.1. What Do We Need?
The ideal diagnostic tool for optimally depicting the coronary arteries should be able to synchronize to the cardiac cycle (“gating”), visualize structures at sub-millimeter resolution (“spatial resolution”), and acquire the entire dataset at time frames of a couple dozens of milliseconds (“temporal resolution”) With the introduction of the 64-slice CT scanners, these requirements were met at such degree that the visualization of the coronary arteries was feasible with diagnostic image quality [5]. Even though most modern scanners exhibit excellent image quality with high isotropic spatial (best 0.35 mm) and temporal (best 65 ms) resolutions, these parameters are still half of what is needed and compared to the resolution provide by invasive coronary angiography (ICA), (0.2 mm and 30 ms, respectively) Developments in hardware technology were mirrored by advances in image processing software.
2.2. Which Protocol Needs to Be Chosen?
Modern scanners are versatile in regard to the type of protocol employed for acquiring the data [6]. This should always be tailored to the specific individual (i.e., habitus, heart rate, irregularities in heart rate, etc.) and the specific clinical question (status of the coronary arteries, left ventricular function, follow-up CCTA, etc.). Generally, three types of ECG-gated protocols can be employed during a CCTA acquisition [7] (Figure 1).
The main advantage of this protocol is the ability to reconstruct CCTA acquisitions at various time points of the cardiac cycle. With this scan mode, also known as “sequential” or “step and shoot”, images can be obtained without table movement during acquisition. This type of acquisition usually provides images with excellent contrast and with relatively low radiation exposure [8][9]. This type of acquisitions offers very high contrast images without “stitching” artefacts with very low radiation exposure for the patient (usually <1 mSv) [10].
However, as the coronary arteries show reduced movement at end-systole as well, and the systole is less affected by irregularities in heart rate, a “step and shoot” acquisition triggered during the systole often provides excellent image quality (Figure 2). Lastly, the technical advances seen in the last decade have enabled the development of protocols that allow the sampling of data needed for a full characterization of the coronary tree during a single heartbeat. This can be achieved in two ways, depending on the scanner. In scanners that allow a detector coverage of >=16 cm, a complete dataset can be acquired without moving the patient and during a single heartbeat, depending on the heart rate [11][12]. Conversely, with dual-source scanners, an ECG-triggered high pitch “helical” or “spiral” acquisition (a pitch value of ≈3) or so-called “Flash” mode allows for the entire dataset to be sampled in one heartbeat [13][14]. This type of acquisitions offers very high contrast images without “stitching” artefacts with very low radiation exposure for the patient (usually <1 mSv) [10] (Figure 3).
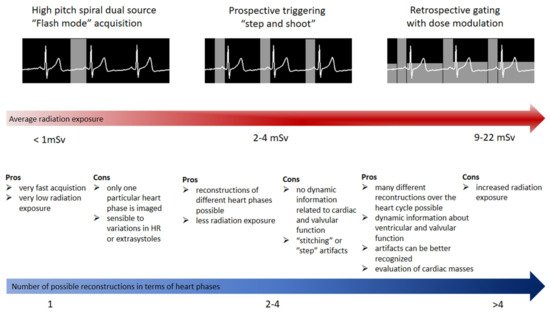
Figure 1. Scan modes used in coronary computer tomography angiography with advantages and disadvantages as well as radiation exposure for each of the different acquisition approaches.
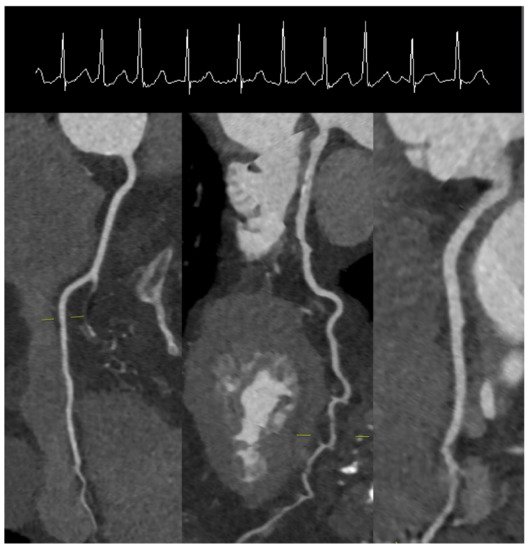
Figure 2. “Step and Shoot” protocol triggering during systole in a patient with atrial fibrillation and a heart rate of 114/min.
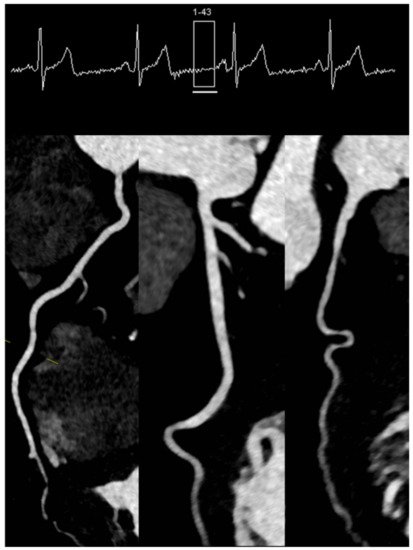
Figure 3. High-pitch dual source spiral protocol (“Flash” mode) in a patient with a stable heart rate of 58/min.
3.3. How Much Can We Reduce Radiation and Contrast Agent Exposure?
Radiation and contrast agent exposure constitute the main risks of a CCTA. With regard to radiation exposure, the radiation received by the patient is mainly dependent on the protocol employed and patient’s habitus. A meta-analysis including over 3000 patients comparing the radiation exposure between retrospective helical and prospective ECG-triggered protocols confirmed a fourfold dose reduction (from 12.3 to 3.5 mSv) with prospective acquisitions [15]. Lastly, the radiation exposure for the patient can be further minimized using prospective ECG-gated high-pitch acquisitions. Several strategies can be employed for reducing the radiation exposure to the patient [16].
The application of contrast agent can have adverse effects on the renal and thyroid function, and the function of these two organs should be evaluated prior to performing the CCTA. Newer scanners can acquire high quality datasets with relatively low amounts of iodine contrast (50–60 mL) and in selected populations can be as low as 30 mL by acquiring at low tube voltages [17][18]. Although each method has advantages and disadvantages, the test bolus method can better help identifying more accurately the optimal moment for acquisition [19][20]. An important aspect of contrast agent administration is to ensure an opacification of coronary vessels between 250 and 350 Hounsfield units (HU), since values outside this range may prevent the accurate evaluation of coronary stenoses [21].
3. Diagnosis
CAC has consistently exhibited significant predictive power for future cardiovascular events, with incremental value to conventional cardiovascular risk factors, including the Framingham risk score. Thus, a CAC of 0 is associated with a low event rate even in the presence of conventional cardiovascular risk factors—event rate of 2.72 per 1000 person-year in patients with three or more risk factors [22]. The main clinical value of CAC lies in the ability to reclassify asymptomatic individuals with an intermediate risk for cardiovascular events on the basis of conventional risk assessment [23][24]. Current European guidelines on cardiovascular disease prevention recommend the use of CAC screening with a IIb indication as a possible risk modifier in cardiovascular risk assessment [25].
CCTA has been extensively compared to invasive coronary angiography for the diagnosis of luminal coronary stenosis [26][27]. In regard to stenosis grading, an important aspect of CCTA has to be taken into account when reporting the severity of the stenosis, namely, that the spatial resolution of the most scanners is still half of that provided by invasive coronary angiography (see above). When that is kept in mind, an exact quantification of luminal stenosis generally is not recommended. Thus, reporting of individual stenosis should be based on the “range” of the stenosis as follows: normal—absence of plaque and no luminal stenosis, 1: minimal—plaque with <25% stenosis, 2: mild—plaque with 25–49% stenosis, 3: moderate—50–69% stenosis, 4:
In addition, if modifiers are present, they should be added at the end of the classification. G is graft, S is stents, and V is plaque vulnerability.
A higher BMI (>30 Kg/m2) could reduce the accuracy of a CCTA scan, mainly due to reduced signal to noise ratio secondary to increased X-ray scatter. Several approaches such as increased tube voltage, very good heart rate preparation, and administration of contrast with a higher rate (up to 7 mL/s) can improve the quality of the CCTA [28]. When many extrasystoles are present or the heart rate shows high variability such as in atrial fibrillation, acquisitions in systole should be favored. Of note, the high-pitch spiral protocol is not without drawbacks, even when the patient has a low heart rate with a minimal heart rate variability.
The diagnostic value of CCTA was compared to other non-invasive functional tests in several studies. Thus, the EVINCI study evaluated 475 patients with stable chest pain with CCTA, stress perfusion imaging, and wall motion imaging by either stress echocardiography or stress cardiovascular magnetic resonance imaging and used the results of invasive coronary angiography as reference standard. Ideally, a new medical tool should not result in increased costs. In the PROMISE trial, there was no significant difference in costs in the short term (<90 days) and long term (3 years) between the CCTA arm and the functional test arm [29].
A major advantage of CCTA over conventional ICA is its ability to non-invasively provide detailed characterization atherosclerotic plaque composition and volume (Figure 4). A quick overview of the atherosclerotic process points the role of wall shear stress (WSS) at the beginning of such pathophysiologic processes, explaining why many of the coronary plaques are seen in regions with an increased shear stress such as bifurcations. However, not all plaques take this pathway, and “stable” plaques, which have a low percentage of necrotic core and high percentage of calcium deposits, are also frequently seen. The exact mechanisms that underpin the development of a specific type of atherosclerotic plaque are not yet completely understood.
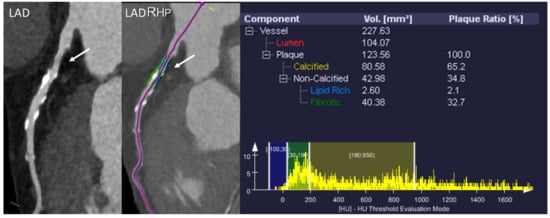
Figure 4. Example of plaque analysis (research software: syngo.via Frontier Coronary Plaque Analysis, Siemens Healthineers). Analysis performed in a moderate plaque in the proximal segment of the LAD. Note the presence of a partially calcified plaque with a predominance of calcium and a low percentage of lipids.
In this regard, a closer look at plaque morphology and composition and comparison with histopathological data revealed several patterns consisting of high-risk features of coronary atherosclerotic plaques in CCTA [30][31]: low attenuation, positive remodeling, spotty calcification, and napkin-ring sign (Figure 5): Similar to all other features of high-risk plaque, positive remodeling is seen more often in patients with ACS compared to patients with CCS [32].Spotty calcifications are more commonly seen in plaques with thin fibrous cap than in stable plaques [33]. Microcalcifications are considered to be a promoter of plaque destabilization and were often identified in culprit lesions of patients with ACS [34].The napkin-ring sign is a form of low attenuation plaque that exhibits a heterogenous pattern of attenuation. This type of pattern is highly suggestive of vulnerable plaque and is considered as a precursor of plaque rupture [35].

Figure 5. Examples of high-risk plaques. (A) Low-attenuation plaque (white arrow). (B) Positive remodeling—note the development of the plaque outside the coronary lumen (white arrow). (C) Spotty calcification—note the presence of calcium in an otherwise low-attenuation plaque (white arrow). (D) Napkin-ring sign—a heterogenous low-attenuation plaque (white arrow) that exhibits a cap with lower HU densities (interrupted white arrow) in comparison to the rest of the plaque.
The role of high-risk features in predicting future cardiovascular events was confirmed in several trials. In the same line, high-risk plaque features were predictive of the endpoint in the SCOT-HEART study [36]. Furthermore, high-risk plaque features were shown to correlate with troponin releases in patients with stable angina, thus suggesting that silent plaque ruptures with micro-embolization can occur in patients deemed as “stable” [37]. In addition, troponin and high-risk plaque features offer additive value in predicting future cardiovascular events [38].
HMG-CoA reductase and newer molecules such as PCSK9 inhibitors or small interfering ribonucleic acid have all exhibited significant effects on reducing cholesterol values and improving the prognosis of patients with CAD [39]. Thus, patients who received high-dose statin therapy exhibited a significant reduction in plaque burden in the ASTEROID and SATURN trials [40][41]. The results are conflicting, and this may be related to the type of study, used methodology, and low number of patients. Nevertheless, a more recent study, involving 467 patients who received LDL-lowering therapies and who were followed up at 2 years with CCTA, highlighted a significant plaque burden reduction in patients who reached a target LDL
Thus, Goeller et al. found that PCAT attenuation is increased around culprit versus non-culprit lesions in patients with ACS [42]. When CCTA is used, a fat attenuation index (FAI) can be derived that expresses weighted attenuation shifts within the perivascular tissue [43]. When measured in the proximal segments of the coronary arteries (i.e., the first 40 mm of the RCA, LAD, and LCX), FAI was shown to mirror the inflammatory burden of the entire coronary tree, detecting early subclinical CAD [44]. Furthermore, in the CRISP-CT study including over 4000 patients the FAI measured around the proximal segment of the RCA exhibited a strong predictive power in regard to all-cause and cardiovascular mortality, improving the predictive model containing conventional cardiovascular risk factors, plaque burden, and high-risk plaque features [45].
The FAME studies elegantly showed that patients undergoing PCI exhibit a benefit in terms of cardiovascular endpoints only when hemodynamically relevant stenoses (FFR < 0.8) are treated [46][47]. The ability of FFRCTto accurately identify hemodynamically relevant stenoses was tested in several studies that used invasive FFR as the reference standard. In addition, a sub-study of the PACIFIC trial evaluated FFRCTagainst invasively measured FFR as well as PET and SPECT and found superior AUC in the diagnosis of relevant coronary stenoses compared to standard CCTA, PET, and SPECT [48]. Thus, it appears that due to model constraints, very distal segments could exhibit values <0.8 without the presence of a hemodynamically relevant stenosis.
Other computational methods were developed to extract hemodynamic data from three-dimensional CCTA datasets. The vFAI can also be obtained from CCTA datasets and was shown to exhibit very strong correlation with invasively measured FFR [49]. An integrative approach in modelling risk stratification, diagnosis, treatment, and prognosis of patients with CAD is represented by the SMARTool [50]. Clinical data, anatomical information, and data extracted using various computational models such as vFAI are fed into a decision support system.
Another function of computational fluid dynamics is to clarify the underlying mechanical mechanisms that determine the evolution of coronary plaques [51][52]. Similar results were obtained in the PREDICTION study that showed that segments with low WSS progress towards higher plaque burden and lumen The integration of CCTA data in the analysis of fluid dynamics has revealed a significant association between higher plaque burden and regions of the coronary tree with low WSS [53]. On the other hand, regions with high WSS appear to be associated with plaques exhibiting high risk features as well as with culprit lesions in patients who develop acute coronary syndromes [54].
The principle is similar to that employed in other non-invasive stress tests such as CMR, SPECT, or PET and is based on inducing “forced” vasodilation of the distal arterioles using hyperemia inducing agents such as adenosine, dipyridamole, or regadenoson [55][56]. Several protocols have been proposed such as dynamic versus static scanning or stress-first versus rest-first scanning, each one exhibiting specific advantages and disadvantages [56]. Dynamic CTP might offer a more quantitative and thus objective approach in establishing myocardial perfusion, but this comes at a higher radiation cost for the patient since serial acquisitions are needed. Moreover, the use of CTP was shown to improve the diagnostic accuracy of CCTA alone in 150 patients with previous stents by identifying relevant in-stent restenosis as shown by the ADVATNAGE trial [57].
4. Prognosis: Can We See into the Future?
Although patients in the CCTA arm had more invasive procedures in the first two years, at the five-year follow-up no difference in the number of invasive procedures was noted between the two arms. In this study, over 10,000 patients were randomized to either a functional testing arm (exercise electrocardiography, nuclear stress testing, or exercise echocardiography) or anatomical testing arm (CCTA). Thus, patients with a normal or mildly abnormal functional testing result still have an event rate of 2.09%, and the discriminatory power of functional testing in terms of prognosis begins only in patients with moderate ischemia. CCTA on the other hand, has an excellent discriminatory power at every stage of disease, with a normal CCTA translating into an exceptionally low event rate of 0.93 and a mildly abnormal CCTA an event rate of 3.01 (c index 0.72 for CCTA vs. 0.64 for functional testing).
References
- Korosoglou, G.; Giusca, S.; Gitsioudis, G.; Erbel, C.; Katus, H.A. Cardiac magnetic resonance and computed tomography angiography for clinical imaging of stable coronary artery disease. Diagnostic classification and risk stratification. Front. Physiol. 2014, 5, 291.
- Knuuti, J.; Ballo, H.; Juarez-Orozco, L.E.; Saraste, A.; Kolh, P.; Rutjes, A.W.S.; Jüni, P.; Windecker, S.; Bax, J.J.; Wijns, W. The performance of non-invasive tests to rule-in and rule-out significant coronary artery stenosis in patients with stable angina: A meta-analysis focused on post-test disease probability. Eur. Hear. J. 2018, 39, 3322–3330.
- Al-Lamee, R.; Thompson, D.; Dehbi, H.-M.; Sen, S.; Tang, K.; Davies, J.; Keeble, T.; Mielewczik, M.; Kaprielian, R.; Malik, I.S.; et al. Percutaneous coronary intervention in stable angina (ORBITA): A double-blind, randomised controlled trial. Lancet 2018, 391, 31–40.
- Maron, D.J.; Hochman, J.S.; Reynolds, H.R.; Bangalore, S.; O’Brien, S.M.; Boden, W.E.; Chaitman, B.R.; Senior, R.; López-Sendón, J.; Alexander, K.P.; et al. Initial Invasive or Conservative Strategy for Stable Coronary Disease. N. Engl. J. Med. 2020, 382, 1395–1407.
- Lawler, L.P.; Pannu, H.K.; Fishman, E.K. MDCT Evaluation of the Coronary Arteries, 2004: How We Do It—Data Acquisition, Postprocessing, Display, and Interpretation. Am. J. Roentgenol. 2005, 184, 1402–1412.
- Toia, P.; La Grutta, L.; Sollami, G.; Clemente, A.; Gagliardo, C.; Galia, M.; Maffei, E.; Midiri, M.; Cademartiri, F. Technical development in cardiac CT: current standards and future improvements—a narrative review. Cardiovasc. Diagn. Ther. 2020, 10, 2018–2035.
- Halliburton, S.; Arbab-Zadeh, A.; Dey, D.; Einstein, A.J.; Gentry, R.; George, R.T.; Gerber, T.; Mahesh, M.; Weigold, W.G. State-of-the-art in CT hardware and scan modes for cardiovascular CT. J. Cardiovasc. Comput. Tomogr. 2012, 6, 154–163.
- Bischoff, B.; Hein, F.; Meyer, T.; Krebs, M.; Hadamitzky, M.; Martinoff, S.; Schömig, A.; Hausleiter, J. Comparison of Sequential and Helical Scanning for Radiation Dose and Image Quality: Results of the Prospective Multicenter Study on Radiation Dose Estimates of Cardiac CT Angiography (PROTECTION) I Study. Am. J. Roentgenol. 2010, 194, 1495–1499.
- Husmann, L.; Valenta, I.; Gaemperli, O.; Adda, O.; Treyer, V.; Wyss, C.A.; Veit-Haibach, P.; Tatsugami, F.; Von Schulthess, G.K.; Kaufmann, P.A. Feasibility of low-dose coronary CT angiography: First experience with prospective ECG-gating. Eur. Hear. J. 2007, 29, 191–197.
- Achenbach, S.; Marwan, M.; Ropers, D.; Schepis, T.; Pflederer, T.; Anders, K.; Kuettner, A.; Daniel, W.G.; Uder, M.; Lell, M.M. Coronary computed tomography angiography with a consistent dose below 1 mSv using prospectively electrocardiogram-triggered high-pitch spiral acquisition. Eur. Hear. J. 2009, 31, 340–346.
- Rybicki, F.J.; Otero, H.J.; Steigner, M.L.; Vorobiof, G.; Nallamshetty, L.; Mitsouras, D.; Ersoy, H.; Mather, R.T.; Judy, P.F.; Cai, T.; et al. Initial evaluation of coronary images from 320-detector row computed tomography. Int. J. Cardiovasc. Imaging 2008, 24, 535–546.
- Khan, A.; Nasir, K.; Khosa, F.; Saghir, A.; Sarwar, S.; Clouse, M.E. Prospective Gating With 320-MDCT Angiography: Effect of Volume Scan Length on Radiation Dose. Am. J. Roentgenol. 2011, 196, 407–411.
- Hausleiter, J.; Bischoff, B.; Hein, F.; Meyer, T.; Hadamitzky, M.; Thierfelder, C.; Allmendinger, T.; Flohr, T.G.; Schömig, A.; Martinoff, S. Feasibility of dual-source cardiac CT angiography with high-pitch scan protocols. J. Cardiovasc. Comput. Tomogr. 2009, 3, 236–242.
- Achenbach, S.; Marwan, M.; Schepis, T.; Pflederer, T.; Bruder, H.; Allmendinger, T.; Petersilka, M.; Anders, K.; Lell, M.; Kuettner, A.; et al. High-pitch spiral acquisition: A new scan mode for coronary CT angiography. J. Cardiovasc. Comput. Tomogr. 2009, 3, 117–121.
- Menke, J.; Unterberg-Buchwald, C.; Staab, W.; Sohns, J.M.; Hosseini, A.S.A.; Schwarz, A. Head-to-head comparison of prospectively triggered vs retrospectively gated coronary computed tomography angiography: Meta-analysis of diagnostic accuracy, image quality, and radiation dose. Am. Hear. J. 2013, 165, 154–163.e3.
- Hausleiter, J.; Meyer, T. Tips to minimize radiation exposure. J. Cardiovasc. Comput. Tomogr. 2008, 2, 325–327.
- Nakaura, T.; Awai, K.; Yauaga, Y.; Nakayama, Y.; Oda, S.; Hatemura, M.; Nagayoshi, Y.; Ogawa, H.; Yamashita, Y. Contrast Injection Protocols for Coronary Computed Tomography Angiography Using a 64-Detector Scanner: Comparison Between Patient Weight-Adjusted- and Fixed Iodine-Dose Protocols. Investig. Radiol. 2008, 43, 512–519.
- Yamamuro, M.; Tadamura, E.; Kanao, S.; Wu, Y.-W.; Tambara, K.; Komeda, M.; Toma, M.; Kimura, T.; Kita, T.; Togashi, T. Coronary angiography by 64-detector row computed tomography using low dose of contrast material with saline chaser: Influence of total injection volume on vessel attenuation. J. Comput. Assist. Tomogr. 2007, 31, 272–280.
- Oda, S.; Utsunomiya, D.; Nakaura, T.; Kidoh, M.; Funama, Y.; Tsujita, K.; Yamashita, Y. Basic Concepts of Contrast Injection Protocols for Coronary Computed Tomography Angiography. Curr. Cardiol. Rev. 2018, 15, 24–29.
- Bae, K.T. Intravenous Contrast Medium Administration and Scan Timing at CT: Considerations and Approaches. Radiology 2010, 256, 32–61.
- Johnson, P.T.; Pannu, H.K.; Fishman, E.K. IV Contrast Infusion for Coronary Artery CT Angiography: Literature Review and Results of a Nationwide Survey. Am. J. Roentgenol. 2009, 192, 214.
- Nasir, K.; Rubin, J.; Blaha, M.J.; Shaw, L.J.; Blankstein, R.; Rivera, J.J.; Khan, A.N.; Berman, D.; Raggi, P.; Callister, T.; et al. Interplay of Coronary Artery Calcification and Traditional Risk Factors for the Prediction of All-Cause Mortality in Asymptomatic Individuals. Circ. Cardiovasc. Imaging 2012, 5, 467–473.
- Erbel, R.; Möhlenkamp, S.; Moebus, S.; Schmermund, A.; Lehmann, N.; Stang, A.; Dragano, D.; Grönemeyer, D.; Seibel, R.; Kälsch, H.; et al. Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: The Heinz Nixdorf Recall study. J. Am. Coll. Cardiol. 2010, 56, 1397–1406.
- Elias-Smale, S.E.; Proença, R.V.; Koller, M.T.; Kavousi, M.; van Rooij, F.J.A.; Hunink, M.G.; Steyerberg, E.W.; Hofman, A.; Oudkerk, M.; Witteman, J.C.M. Coronary calcium score improves classification of coronary heart disease risk in the elderly: The Rotterdam study. J. Am. Coll. Cardiol. 2010, 56, 1407–1414.
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart J. 2016, 37, 2315–2381.
- Stein, P.D.; Yaekoub, A.Y.; Matta, F.; Sostman, H.D. 64-Slice CT for Diagnosis of Coronary Artery Disease: A Systematic Review. Am. J. Med. 2008, 121, 715–725.
- Sun, Z.; Lin, C.; Davidson, R.; Dong, C.; Liao, Y. Diagnostic value of 64-slice CT angiography in coronary artery disease: A systematic review. Eur. J. Radiol. 2008, 67, 78–84.
- Mangold, S.; Wichmann, J.L.; Schoepf, U.J.; Litwin, S.E.; Canstein, C.; Varga-Szemes, A.; Muscogiuri, G.; Fuller, S.R.; Stubenrauch, A.C.; Nikolaou, K.; et al. Coronary CT angiography in obese patients using 3rd generation dual-source CT: Effect of body mass index on image quality. Eur. Radiol. 2016, 26, 2937–2946.
- Mark, D.B.; Federspiel, J.J.; Cowper, P.A.; Anstrom, K.J.; Hoffmann, U.; Patel, M.R.; Davidson-Ray, L.; Daniels, M.R.; Cooper, L.S.; Knight, J.D.; et al. Economic Outcomes With Anatomical Versus Functional Diagnostic Testing for Coronary Artery Disease. Ann. Intern. Med. 2016, 165, 94–102.
- Schaar, J.A.; Muller, J.E.; Falk, E.; Virmani, R.; Fuster, V.; Serruys, P.W.; Colombo, A.; Stefanadis, C.; Casscells, S.W.; Moreno, P.R.; et al. Terminology for high-risk and vulnerable coronary artery plaques. Eur. Hear. J. 2004, 25, 1077–1082.
- Maurovich-Horvat, P.; Ferencik, M.; Voros, S.; Merkely, B.; Hoffmann, U. Comprehensive plaque assessment by coronary CT angiography. Nat. Rev. Cardiol. 2014, 11, 390–402.
- Hoffmann, U.; Moselewski, F.; Nieman, K.; Jang, I.-K.; Ferencik, M.; Rahman, A.M.; Cury, R.C.; Abbara, S.; Joneidi-Jafari, H.; Achenbach, S.; et al. Noninvasive Assessment of Plaque Morphology and Composition in Culprit and Stable Lesions in Acute Coronary Syndrome and Stable Lesions in Stable Angina by Multidetector Computed Tomography. J. Am. Coll. Cardiol. 2006, 47, 1655–1662.
- Van Velzen, J.E.; de Graaf, F.R.; de Graaf, M.A.; Schuijf, J.D.; Kroft, L.J.; de Roos, A.; Reiber, J.H.C.; Bax, J.J.; Jukema, J.W.; Boersma, E.; et al. Comprehensive assessment of spotty calcifications on computed tomography angiography: Comparison to plaque characteristics on intravascular ultrasound with radiofrequency backscatter analysis. J. Nucl. Cardiol. 2011, 18, 893–903.
- Pflederer, T.; Marwan, M.; Schepis, T.; Ropers, D.; Seltmann, M.; Muschiol, G.; Daniel, W.G.; Achenbach, S. Characterization of culprit lesions in acute coronary syndromes using coronary dual-source CT angiography. Atherosclerosis 2010, 211, 437–444.
- Seifarth, H.; Schlett, C.L.; Nakano, M.; Otsuka, F.; Károlyi, M.; Liew, G.; Maurovich-Horvat, P.; Alkadhi, H.; Virmani, R.; Hoffmann, U. Histopathological correlates of the napkin-ring sign plaque in coronary CT angiography. Atherosclerosis 2012, 224, 90–96.
- Williams, M.C.; Kwiecinski, J.; Doris, M.; McElhinney, P.; D’Souza, M.S.; Cadet, S.; Adamson, P.D.; Moss, A.J.; Alam, S.; Hunter, A.; et al. Low-Attenuation Noncalcified Plaque on Coronary Computed Tomography Angiography Predicts Myocardial Infarction. Circulation 2020, 141, 1452–1462.
- Korosoglou, G.; Lehrke, S.; Mueller, D.; Hosch, W.; Kauczor, H.-U.; Humpert, P.M.; Giannitsis, E.; A Katus, H. Determinants of troponin release in patients with stable coronary artery disease: Insights from CT angiography characteristics of atherosclerotic plaque. Heart 2010, 97, 823–831.
- Gitsioudis, G.; Schüssler, A.; Nagy, E.; Maurovich-Horvat, P.; Buss, S.J.; Voss, A.; Hosch, W.; Hofmann, N.; Kauczor, H.-U.; Giannitsis, E.; et al. Combined Assessment of High-Sensitivity Troponin T and Noninvasive Coronary Plaque Composition for the Prediction of Cardiac Outcomes. Radiology 2015, 276, 141110-81.
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur. Heart J. 2020, 41, 111–188.
- Nissen, S.E.; Nicholls, S.J.; Sipahi, I.; Libby, P.; Raichlen, J.S.; Ballantyne, C.M.; Davignon, J.; Erbel, R.; Fruchart, J.C.; Tardif, J.C.; et al. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: The ASTEROID trial. JAMA 2006, 295, 1556–1565.
- Nicholls, S.J.; Ballantyne, C.M.; Barter, P.J.; Chapman, M.J.; Erbel, R.M.; Libby, P.; Raichlen, J.S.; Uno, K.; Borgman, M.; Wolski, K.; et al. Effect of Two Intensive Statin Regimens on Progression of Coronary Disease. N. Engl. J. Med. 2011, 365, 2078–2087.
- Goeller, M.; Achenbach, S.; Cadet, S.; Kwan, A.C.; Commandeur, F.; Slomka, P.J.; Gransar, H.; Albrecht, M.H.; Tamarappoo, B.K.; Berman, D.S.; et al. Pericoronary Adipose Tissue Computed Tomography Attenuation and High-Risk Plaque Characteristics in Acute Coronary Syndrome Compared With Stable Coronary Artery Disease. JAMA Cardiol. 2018, 3, 858–863.
- Antoniades, C.; Kotanidis, C.; Berman, D.S. State-of-the-art review article. Atherosclerosis affecting fat: What can we learn by imaging perivascular adipose tissue? J. Cardiovasc. Comput. Tomogr. 2019, 13, 288–296.
- Antonopoulos, A.; Sanna, F.; Sabharwal, N.; Thomas, S.; Oikonomou, E.K.; Herdman, L.; Margaritis, M.; Shirodaria, C.; Kampoli, A.-M.; Akoumianakis, I.; et al. Detecting human coronary inflammation by imaging perivascular fat. Sci. Transl. Med. 2017, 9, eaal2658.
- Oikonomou, E.K.; Marwan, M.; Desai, M.Y.; Mancio, J.; Alashi, A.; Centeno, E.H.; Thomas, S.; Herdman, L.; Kotanidis, C.; E Thomas, K.; et al. Non-invasive detection of coronary inflammation using computed tomography and prediction of residual cardiovascular risk (the CRISP CT study): a post-hoc analysis of prospective outcome data. Lancet 2018, 392, 929–939.
- Tonino, P.A.; De Bruyne, B.; Pijls, N.H.; Siebert, U.; Ikeno, F.; Veer, M.V.; Klauss, V.; Manoharan, G.; Engstrøm, T.; Oldroyd, K.G.; et al. Fractional Flow Reserve versus Angiography for Guiding Percutaneous Coronary Intervention. N. Engl. J. Med. 2009, 360, 213–224.
- De Bruyne, B.; Pijls, N.H.; Kalesan, B.; Barbato, E.; Tonino, P.A.; Piroth, Z.; Jagic, N.; Mobius-Winckler, S.; Rioufol, G.; Witt, N.; et al. Fractional Flow Reserve–Guided PCI versus Medical Therapy in Stable Coronary Disease. N. Engl. J. Med. 2012, 367, 991–1001.
- Driessen, R.S.; Danad, I.; Stuijfzand, W.J.; Raijmakers, P.G.; Schumacher, S.P.; van Diemen, P.A.; Leipsic, J.A.; Knuuti, J.; Underwood, S.R.; van de Ven, P.M.; et al. Comparison of Coronary Computed Tomography Angiography, Fractional Flow Reserve, and Perfusion Imaging for Ischemia Diagnosis. J. Am. Coll. Cardiol. 2019, 73, 161–173.
- Siogkas, P.K.; Anagnostopoulos, C.D.; Liga, R.; Exarchos, T.P.; Sakellarios, A.I.; Rigas, G.; Scholte, A.J.H.A.; Papafaklis, M.I.; Loggitsi, D.; Pelosi, G.; et al. Noninvasive CT-based hemodynamic assessment of coronary lesions derived from fast computational analysis: a comparison against fractional flow reserve. Eur. Radiol. 2018, 29, 2117–2126.
- Sakellarios, A.I.; Rigas, G.; Kigka, V.; Siogkas, P.; Tsompou, P.; Karanasiou, G.; Exarchos, T.; Andrikos, I.; Tachos, N.; Pelosi, G.; et al. SMARTool: A tool for clinical decision support for the management of patients with coronary artery disease based on modeling of atherosclerotic plaque process. In Proceedings of the 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Jeju Island, South Korea, 11–15 July 2017; Institute of Electrical and Electronics Engineers (IEEE): Piscataway, NJ, SAD, 2017; Volume 2017, pp. 96–99.
- Sun, Z.; Xu, L. Computational fluid dynamics in coronary artery disease. Comput. Med Imaging Graph. 2014, 38, 651–663.
- Carvalho, V.; Pinho, D.; Lima, R.A.; Teixeira, J.C.; Teixeira, S. Blood Flow Modeling in Coronary Arteries: A Review. Fluids 2021, 6, 53.
- Hetterich, H.; Jaber, A.; Gehring, M.; Curta, A.; Bamberg, F.; Filipovic, N.; Rieber, J. Coronary Computed Tomography Angiography Based Assessment of Endothelial Shear Stress and Its Association with Atherosclerotic Plaque Distribution In-Vivo. PLoS ONE 2015, 10, e0115408.
- Lee, J.M.; Choi, G.; Koo, B.-K.; Hwang, D.; Park, J.; Zhang, J.; Kim, K.-J.; Tong, Y.; Kim, H.J.; Grady, L.; et al. Identification of High-Risk Plaques Destined to Cause Acute Coronary Syndrome Using Coronary Computed Tomographic Angiography and Computational Fluid Dynamics. JACC: Cardiovasc. Imaging 2019, 12, 1032–1043.
- Salerno, M.; Beller, G.A. Noninvasive Assessment of Myocardial Perfusion. Circ. Cardiovasc. Imaging 2009, 2, 412–424.
- Yang, D.H.; Kim, Y.-H. CT myocardial perfusion imaging: Current status and future perspectives. Int. J. Cardiovasc. Imaging 2017, 52, 1009–1020.
- Andreini, D.; Mushtaq, S.; Pontone, G.; Conte, E.; Collet, C.; Sonck, J.; D’Errico, A.; Di Odoardo, L.; Guglielmo, M.; Baggiano, A.; et al. CT Perfusion Versus Coronary CT Angiography in Patients With Suspected In-Stent Restenosis or CAD Progression. JACC: Cardiovasc. Imaging 2020, 13, 732–742.





