Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Guillaume Gaudet | + 982 word(s) | 982 | 2021-05-26 08:43:24 | | | |
| 2 | Vicky Zhou | Meta information modification | 982 | 2021-06-15 05:20:12 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Gaudet, G. Sensorless/Sensor-Based Upper Limb Exoskeletons. Encyclopedia. Available online: https://encyclopedia.pub/entry/10827 (accessed on 08 February 2026).
Gaudet G. Sensorless/Sensor-Based Upper Limb Exoskeletons. Encyclopedia. Available at: https://encyclopedia.pub/entry/10827. Accessed February 08, 2026.
Gaudet, Guillaume. "Sensorless/Sensor-Based Upper Limb Exoskeletons" Encyclopedia, https://encyclopedia.pub/entry/10827 (accessed February 08, 2026).
Gaudet, G. (2021, June 14). Sensorless/Sensor-Based Upper Limb Exoskeletons. In Encyclopedia. https://encyclopedia.pub/entry/10827
Gaudet, Guillaume. "Sensorless/Sensor-Based Upper Limb Exoskeletons." Encyclopedia. Web. 14 June, 2021.
Copy Citation
Sensorless and sensor-based upper limb exoskeletons that enhance or support daily motor function are limited for children.
exoskeleton
upper limb
pediatrics
biomechatronics
1. Introduction
There is a wide variety of diagnoses that impair the arm movements of children, such as muscular dystrophy [1], spinal muscular atrophy [2], cerebral palsy [3], arthrogryposis multiplex congenita [4], and brachial plexus palsy [5]. Despite the important differences in the origin of these diseases, they all share a similar symptom: muscular weakness or stiffness at the upper limb. Such symptoms prevent these children from moving their upper limb freely.
For children, the difficulty of moving the upper limb and, hence, interacting with their environment can have great consequences for the learning process. Indeed, it is known that children with limited exploration ability are at higher risk of developing cognitive, social, and motor impairments [6]. Moreover, weakness or impairments at the upper limb decrease autonomy in most activities of daily living (ADL), such as eating, bathing, getting dressed, and playing [7][8].
Traditional interventions to improve upper extremity function in children consist of strength training and aquatic therapy [9][10][11]. There is also evidence about the benefits of neuromuscular electrical stimulation to improve upper extremity strength, range of motion, and function [12]. The efficiency of these interventions relies on the frequency at which they are provided. However, it is often impossible for the specialized therapists to ensure sufficient hours to every child in order to maximize the intervention benefits. Another factor that ensures efficiency and security of these interventions comes from the patient feedback, which is not always reliable with children.
In the last few years, numerous sensorless and sensor-based exoskeletons have been developed to improve the quality of life of people with impairments at the upper limb, by acting both for rehabilitation, i.e., enhancement of the motor function, and assistance, i.e., support of the motor function. Furthermore, exoskeletons showed potential to increase intensive therapy [13] and reduce the workload of the therapists [14]. However, the targeted population for these devices is mainly adults who are recovering from a stroke. These include the ARMIN III [15], the CADEN-7 [16], the CAREX [17], the ETS-MARSE [18], the IntelliArm [19], the RUPERT [20], and the SUEFUL-7 [21].
Despite the increasing number of rehabilitation and assistance exoskeletons developed for adults, the options available for children are limited [22][23]. This is mainly due to the fact that a simple scaling of adult devices to children’s size is not appropriate for safe use. Indeed, additional considerations towards children’s growth, usage, and muscle force must be made in the design process since this population is heterogenous [22]. Further developments are desired since it is known that a greater functional improvement can be reached in robot-assisted rehabilitation compared to traditional interventions [24].
In the last few years, numerous reviews on upper limb exoskeletons have been published. However, these reviews mostly addressed the trends and challenges of exoskeletons and robotic rehabilitation devices for adults [25][26][27][28][29][30][31]. The review by Falzarano et al. [23] focused on pediatric rehabilitation devices but did not include any assistance exoskeletons, which are sometimes the preferred option depending on the child’s diagnosis.
2. Classification of Sensorless and Sensor-Based Upper Limb Exoskeletons
In this review, the term sensorless describes exoskeletons that do not contain any form of sensor. Conversely, the term sensor-based is used to describe exoskeletons that contain at least one type of sensor which can provide useful information to the user or therapist.
Upper limb exoskeletons can be classified using several methods [26], such as the applied segment, the number of active DOF, the method of actuation, the method of power transmission, and the application domain. In this review, the upper limb exoskeletons are first classified as sensorless or sensor-based. Each exoskeleton is then categorized regarding its application domain, motorization solution, targeted population(s), and supported movement(s) (Figure 1).
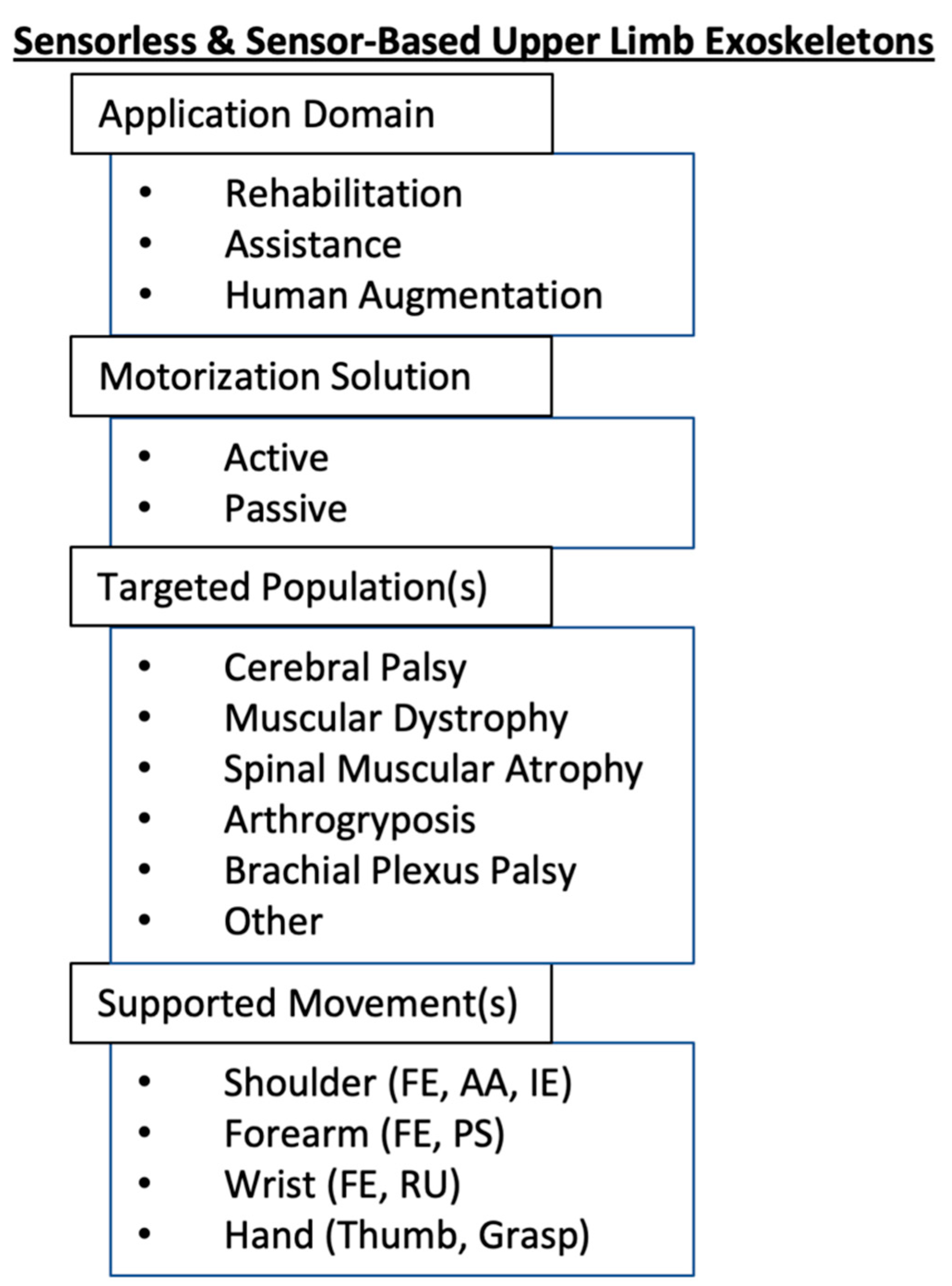 Figure 1. Categorization of sensorless and sensor-based upper limb exoskeletons in pediatrics. Abbreviations: FE: flexion–extension, AA: abduction–adduction, IE: internal–external rotation, PS: pronation–supination, RU: radial–ulnar deviation.
Figure 1. Categorization of sensorless and sensor-based upper limb exoskeletons in pediatrics. Abbreviations: FE: flexion–extension, AA: abduction–adduction, IE: internal–external rotation, PS: pronation–supination, RU: radial–ulnar deviation.Each exoskeleton was first categorized according to its application domain: rehabilitation or assistance. A rehabilitation exoskeleton’s primary purpose is to enhance motor function by allowing partial or full recovery of the impairment. An assistance exoskeleton’s primary purpose is to support the motor function by facilitating the movements of the upper limb. While assistance exoskeletons can also have a rehabilitation purpose, the targeted population for this type of device is mainly people with a condition that cannot be improved. A third category, known as augmentation exoskeletons, was not included in this review. The primary purpose of these exoskeletons is to improve human strength and endurance [32]. Therefore, the principal users of augmentation exoskeletons are healthy adults, which are not the subject of interest for this review.
Regarding the motorization solution, each device was categorized as active or passive. An active exoskeleton uses powered actuators to move the user joints. A passive exoskeleton generally uses gravity compensation mechanisms to reduce the effect of gravity on the user’s arm.
The movements supported by upper limb exoskeletons can either be at the shoulder, the elbow, the wrist, the hand, or a combination of these.
3. Conclusions
We highlighted that the most prevalent diagnoses in pediatrics do not allow for potential motor function improvements. Therefore, it is essential for these children to have access to an exoskeleton that can assist them in ADL. Assistance exoskeletons are better suited than rehabilitation exoskeletons in pediatrics. There exist both sensorless and sensor-based assistance exoskeletons. However, sensor-based exoskeletons are more promising since the additional data provided by the sensors allow better adjustment to the user’s needs. Nevertheless, the options in pediatrics are still limited when comparing to adults. This is mainly explained by additional challenges regarding children’s growth and wearability. New design methods, such as user-centered approaches, will help to tackle these challenges and improve the accessibility of pediatric exoskeletons. This is important to improve children’s participation in ADL and limit the risks of cognitive, social, and motor impairments during their development.
References
- Emery, A. The Muscular Dystrophies. Lancet 2002, 359, 687–695.
- Lunn, M.R.; Wang, C.H. Spinal Muscular Atrophy. Lancet 2008, 371, 2120–2133.
- Odding, E.; Roebroeck, M.E.; Stam, H.J. The Epidemiology of Cerebral Palsy: Incidence, Impairments and Risk Factors. Disabil. Rehabil. 2006, 28, 183–191.
- Bamshad, M.; Van Heest, A.E.; Pleasure, D. Arthrogryposis: A Review and Update. J. Bone Jt. Surg. Am. 2009, 91, 40–46.
- Van der Looven, R.; Le Roy, L.; Tanghe, E.; Samijn, B.; Roets, E.; Pauwels, N.; Deschepper, E.; De Muynck, M.; Vingerhoets, G.; Van den Broeck, C. Risk Factors for Neonatal Brachial Plexus Palsy: A Systematic Review and Meta-Analysis. Dev. Med. Child Neurol. 2020, 62, 673–683.
- Lobo, M.A.; Harbourne, R.T.; Dusing, S.C.; McCoy, S.W. Grounding Early Intervention: Physical Therapy Cannot Just Be about Motor Skills Anymore. Phys. Ther. 2013, 93, 94–103.
- Magermans, D.J.; Chadwick, E.K.J.; Veeger, H.E.J.; van der Helm, F.C.T. Requirements for Upper Extremity Motions during Activities of Daily Living. Clin. Biomech. Bristol Avon 2005, 20, 591–599.
- Hatch, M.N.; Kurillo, G.; Chan, V.; Han, J.J. Motion Sensor-Acquired Reachable Workspace Correlates with Patient-Reported Upper Extremity Activities of Daily Living (ADL) Function in Facioscapulohumeral Dystrophy. Muscle Nerve 2021, 63, 250–257.
- Kim, D.-A.; Lee, J.-A.; Hwang, P.-W.; Lee, M.-J.; Kim, H.-K.; Park, J.-J.; You, J.H.; Lee, D.-R.; Lee, N.-G. The Effect of Comprehensive Hand Repetitive Intensive Strength Training (CHRIST) Using Motion Analysis in Children with Cerebral Palsy. Ann. Rehabil. Med. 2012, 36, 39–46.
- Iftikhar, M.; Frey, J.; Shohan, M.J.; Malek, S.; Mousa, S.A. Current and Emerging Therapies for Duchenne Muscular Dystrophy and Spinal Muscular Atrophy. Pharmacol. Ther. 2021, 220, 107719.
- Lai, C.-J.; Liu, W.-Y.; Yang, T.-F.; Chen, C.-L.; Wu, C.-Y.; Chan, R.-C. Pediatric Aquatic Therapy on Motor Function and Enjoyment in Children Diagnosed with Cerebral Palsy of Various Motor Severities. J. Child Neurol. 2015, 30, 200–208.
- Wright, P.A.; Durham, S.; Ewins, D.J.; Swain, I.D. Neuromuscular Electrical Stimulation for Children with Cerebral Palsy: A Review. Arch. Dis. Child. 2012, 97, 364–371.
- Keller, U.; Riener, R. Design of the Pediatric Arm Rehabilitation Robot ChARMin. In Proceedings of the 5th IEEE RAS/EMBS International Conference on Biomedical Robotics and Biomechatronics, Sao Paulo, Brazil, 12–15 August 2014; pp. 530–535.
- Krebs, H.I.; Hogan, N.; Aisen, M.L.; Volpe, B.T. Robot-Aided Neurorehabilitation. IEEE Trans. Rehabil. Eng. Publ. IEEE Eng. Med. Biol. Soc. 1998, 6, 75–87.
- Nef, T.; Guidali, M.; Riener, R. ARMin III – Arm Therapy Exoskeleton with an Ergonomic Shoulder Actuation. Appl. Bionics Biomech. 2009, 6, 127–142.
- Perry, J.C.; Rosen, J.; Burns, S. Upper-Limb Powered Exoskeleton Design. IEEE ASME Trans. Mechatron. 2007, 12, 408–417.
- Mao, Y.; Agrawal, S.K. Design of a Cable-Driven Arm Exoskeleton (CAREX) for Neural Rehabilitation. IEEE Trans. Robot. 2012, 28, 922–931.
- Rahman, M.H.; Rahman, M.J.; Cristobal, O.L.; Saad, M.; Kenné, J.P.; Archambault, P.S. Development of a Whole Arm Wearable Robotic Exoskeleton for Rehabilitation and to Assist Upper Limb Movements. Robotica 2015, 33, 19–39.
- Park, H.; Ren, Y.; Zhang, L.-Q. IntelliArm: An Exoskeleton for Diagnosis and Treatment of Patients with Neurological Impairments. In Proceedings of the 2nd IEEE RAS EMBS International Conference on Biomedical Robotics and Biomechatronics, Scottsdale, AZ, USA, 19–22 October 2008; pp. 109–114.
- Balasubramanian, S.; Wei, R.; Perez, M.; Shepard, B.; Koeneman, E.; Koeneman, J.; He, J. RUPERT: An Exoskeleton Robot for Assisting Rehabilitation of Arm Functions. In Proceedings of the Virtual Rehabilitation, Vancouver, BC, Canada, 25–27 August 2008; pp. 163–167.
- Gopura, R.A.R.C.; Kiguchi, K.; Li, Y. SUEFUL-7: A 7DOF Upper-Limb Exoskeleton Robot with Muscle-Model-Oriented EMG-Based Control. In Proceedings of the IEEE/RSJ International Conference on Intelligent Robots and Systems, St. Louis, MO, USA, 10–15 October 2009; pp. 1126–1131.
- Keller, U.; Klamroth, V.; van Hedel, H.J.A.; Riener, R. ChARMin: A Robot for Pediatric Arm Rehabilitation. In Proceedings of the IEEE International Conference on Robotics and Automation, Karlsruhe, Germany, 6–10 May 2013; pp. 3908–3913.
- Falzarano, V.; Marini, F.; Morasso, P.; Zenzeri, J. Devices and Protocols for Upper Limb Robot-Assisted Rehabilitation of Children with Neuromotor Disorders. Appl. Sci. 2019, 9, 2689.
- Berdina, O.N.; Bairova, T.A.; Rychkova, L.V.; Sheptunov, S.A. The Pediatric Robotic-Assisted Rehabilitation Complex for Children and Adolescents with Cerebral Palsy: Background and Product Design. In Proceedings of the International Conference “Quality Management, Transport and Information Security, Information Technologies” (IT QM IS), St. Petersburg, Russia, 24–30 September 2017; pp. 360–363.
- Gull, M.A.; Bai, S.; Bak, T. A Review on Design of Upper Limb Exoskeletons. Robotics 2020, 9, 16.
- Gopura, R.A.R.C.; Bandara, D.S.V.; Kiguchi, K.; Mann, G.K.I. Developments in Hardware Systems of Active Upper-Limb Exoskeleton Robots: A Review. Robot. Auton. Syst. 2016, 75, 203–220.
- Stewart, A.M.; Pretty, C.G.; Adams, M.; Chen, X. Review of Upper Limb Hybrid Exoskeletons. IFAC-PapersOnLine 2017, 50, 15169–15178.
- Rehmat, N.; Zuo, J.; Meng, W.; Liu, Q.; Xie, S.Q.; Liang, H. Upper Limb Rehabilitation Using Robotic Exoskeleton Systems: A Systematic Review. Int. J. Intell. Robot. Appl. 2018, 2, 283–295.
- Demofonti, A.; Carpino, G.; Zollo, L.; Johnson, M.J. Affordable Robotics for Upper Limb Stroke Rehabilitation in Developing Countries: A Systematic Review. IEEE Trans. Med. Robot. Bionics 2021, 3, 11–20.
- Islam, M.R.; Brahmi, B.; Ahmed, T.; Assad-Uz-Zaman, M.; Rahman, M.H. Chapter 9—Exoskeletons in upper limb rehabilitation: A review to find key challenges to improve functionality. In Control Theory in Biomedical Engineering; Boubaker, O., Ed.; Academic Press: Cambridge, MA, USA, 2020; pp. 235–265. ISBN 978-0-12-821350-6.
- Qassim, H.M.; Wan Hasan, W.Z. A Review on Upper Limb Rehabilitation Robots. Appl. Sci. 2020, 10, 6976.
- Sawicki, G.S.; Beck, O.N.; Kang, I.; Young, A.J. The Exoskeleton Expansion: Improving Walking and Running Economy. J. Neuroeng. Rehabil. 2020, 17, 25.
More
Information
Subjects:
Engineering, Biomedical
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
886
Revisions:
2 times
(View History)
Update Date:
15 Jun 2021
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




