Chronic inflammation and oxidative stress are two major mechanisms leading to the imbalance between bone resorption and bone formation rate, and subsequently, bone loss. Thus, functional foods and dietary compounds with antioxidant and anti-inflammatory could protect skeletal health. This review aims to examine the current evidence on the skeletal protective effects of propolis, a resin produced by bees, known to possess antioxidant and anti-inflammatory activities.
1. Introduction
The skeletal system consisting of dense connective tissues, mainly bone, is metabolically active and functionally diverse. It undergoes modelling (construction) and remodelling (reconstruction) process in response to stimuli throughout our lifetime
[1][2]. Bone loss associated with age is often a result of defective bone remodelling. Bone remodelling refers to the skeletal reparative process, whereby small areas of bone are resorbed by osteoclasts and replaced by osteoblasts to prevent the accumulation of microfractures and preserve mineral homeostasis by releasing calcium and phosphorus into the circulation. This tightly regulated process replaces 10% of the bone annually and ensures that skeletal structural integrity, mass and mechanical strength are preserved
[3][4].
Many endogenous and exogenous factors influence the bone remodelling process. Among the factors is oxidative stress resulted from an imbalance between oxidants [reactive oxygen species (ROS) and reactive nitrogen species (RNS)] and antioxidants (enzymatic and non-enzymatic)
[5][6]. Oxidative stress favours osteoclast formation (osteoclastogenesis) and bone resorption while hampering osteoblast formation (osteoblastogenesis) and bone formation, leading to bone loss
[7][8][9]. These skeletal effects are achieved by activating signalling pathways, such as mitogen-activated protein kinases (MAPKs), including extracellular signal-regulated kinases (ERK1/2), c-Jun-N terminal kinase (JNK), and p38 MAPK
[10][11][12]. Given the role of oxidative stress in the development of bone loss, antioxidants present in food could have beneficial skeletal effects. Antioxidants improve the survival and functions of osteoblasts and osteocytes, while suppressing osteoclastogenesis and osteoclast activity
[7][10][13][14]. Vitamin C, vitamin E, polyphenols, and other antioxidants have been shown to promote osteoblastogenesis, as well as preventing oxidative stress-induced apoptosis of osteoblasts and osteoclastogenesis
[15][16][17][18].
Inflammation is closely associated with oxidative stress. Phagocytes involved in the immune response synthesise ROS to destroy the invading pathogens. These ROS could diffuse to the surrounding tissues causing damage. Both lipopolysaccharide from the bacterial cell wall and interleukin (IL)-4 synthesised by the immune cells could activate nicotinamide adenine dinucleotide phosphate (NADPH) oxidases (NOX) which generate ROS. In reciprocal, ROS can activate nuclear factor kappa B (NF-κB) signalling pathway and nucleotide-binding and oligomerisation domain-like receptor family pyrin domain containing 3 inflammasome
[19][20]. As implicated in inflammatory bowel disease, rheumatoid arthritis and systemic lupus erythematosus, chronic inflammation is a strong risk factor for bone loss. The pro-inflammatory cytokines released by immune cells potentiate inflammation and promote bone resorption and impair bone formation, resulting in accelerated bone loss and increased fracture risk
[21][22][23].
Propolis (or bee glue) is a natural resin mixture produced by honeybees from plant parts, buds, and exudates. Given its waxy consistency and mechanical properties, propolis is used by the bees in the construction and repair of hives to protect against foreign predators and weather elements
[24][25]. Propolis contains over 300 potentially active ingredients, including coumarins, phenolic aldehydes, steroids, amino acids and polyphenols
[26]. Its functions as an immune enhancer, antibacterial, anti-inflammatory, anti-tumour and antioxidant agent have been investigated
[27][28]. The antioxidant properties of propolis are contributors to its other biological effects, including chemoprevention
[29] and anti-inflammation
[30]. With regard to its anti-inflammatory effects, propolis could inhibit the synthesis of prostaglandin E2 and the inducible cyclooxygenase-2 expression
[25][31][32]. In a model of carrageenin-induced paw oedema, propolis prevented inflammation probably by inhibiting nitric oxide (NO) production
[30]. Regarding its antioxidant effects, propolis prevented DNA damage caused by hydrogen peroxide in fibroblasts
[33]. It also inhibits protein nitration, peroxidation of low-density lipoprotein and endothelial NOX expression, and increases endothelial nitric oxide synthase expression
[34]. Besides, propolis could enhance antioxidant capacity in animals
[35] and humans
[36], thereby lowering lipid peroxidation, which is linked to an increased risk of cardiovascular diseases
[37][38].
2. Possible Molecular Mechanisms of Propolis in Preserving Skeletal Health
Many studies have shown that antioxidants help to promote osteoblast differentiation, mineralisation and reduce osteoclast activity by directly or indirectly counteracting the effects of oxidants
[13][14][39]. Propolis has been shown to possess antioxidant activity
[40], and the majority of studies showing a reduction in oxidative stress markers with propolis treatment
[41]. Guney et al.
[42] reported a reduction in femoral SOD and glutathione levels in rats treated with propolis. The authors suggested that the administration of an exogenous antioxidant could reduce endogenous antioxidant enzyme expression because the components in propolis could scavenge free radicals
[42]. Malondialdehyde (MDA) is frequently used as an indicator of oxidative lipid damage. Wiwekowati et al.
[43] reported that propolis reduced MDA levels in rats with OTM. Propolis could effectively eliminate free radicals due to the polyphenol content
[44]. Flavonoids, one of the polyphenols in propolis, are potent antioxidants capable of scavenging free radicals, thereby shielding the cell membrane from lipid peroxidation
[45]. A positive relationship has been established between the flavonoid content and propolis inhibition of MDA
[46]. Caffeic acid phenethyl ester (CAPE) has also been linked to the antioxidant properties of propolis
[18]. Propolis extracts containing CAPE were more efficient at inhibiting xanthine oxidase and lipoperoxidase activity than propolis extracts lacking CAPE
[47]. The presence of caffeic acid and phenyl caffeate is linked to the high antioxidant potential of propolis
[48].
M-CSF and RANKL are two essential cytokines regulating osteoclast differentiation. M-CSF ensures the survival and proliferation of osteoclast precursor cells. It also increases the RANK expression in osteoclast precursor cells, ensuring a more efficient response to the RANKL-RANK signalling pathways
[49][50][51][52]. Wimolsantirungsri et al.
[53] reported decreased RANKL and M-CSF-induced RANK expression in osteoclast precursor cells following propolis treatment, suggesting the inhibition of RANKL-RANK signalling pathway, which would eventually lead to reduced osteoclast differentiation. RANKL activates several transcription factors, including NFAT2, a master regulator of osteoclast differentiation that controls the expression of several osteoclast-specific genes, such as TRAP, cathepsin K, and CTR
[54][55][56][57]. Two studies demonstrated that propolis inhibited osteoclast formation from human peripheral blood mononuclear cells
[53] and RAW 264.7 cells
[58] by inhibiting the expression of NFAT2, cathepsin K and CTR.
Inflammatory cytokines cause bone loss by promoting osteoclast differentiation and maturation directly. These cytokines work together to attract, differentiate, and activate osteoclasts through the NF-κB signalling pathway
[59][60][61]. Propolis-incorporated bone implants were shown to downregulate the expression of IL-1β, and TNF-α at the surrounding tissue
[62], thereby preventing osteoclast formation and bone resorption that would loosen the implants. Another study on ligature-induced periodontitis failed to reduce circulating inflammatory cytokines by propolis, probably because the rats also presented diabetes and a higher degree of inflammation
[63]. Propolis suppressed LPS-induced expression of IL-1β, IL-6, and IL-8 in human periodontal ligament cells
[64] and IL-6 in RAW264.7 macrophages
[65].
Osteoblasts derived from mesenchymal stem cells in the bone marrow are responsible for the synthesis, secretion, and mineralisation of bone matrix. They also secrete OPG, a RANKL decoy receptor that prevents the binding of RANKL to RANK, thereby halting RANKL signalling and osteoclastogenesis
[66]. Propolis was shown to stimulate the proliferation, differentiation and maturation of osteoblasts
[67]. Among the many osteoblast markers, OPG expression was also upregulated by propolis, indicating that it could affect RANKL/OPG dynamic or crosstalk between osteoblasts and osteoclasts, thereby suppressing osteoclastogenesis.
BMPs are growth factors belonging to the transforming growth factor-superfamily. Their diverse functions range from regulating bone induction, preservation, and reconstruction to determining non-osteogenic embryological developmental pathways and maintaining adult tissue homeostasis
[68]. BMP-2 and 7 are involved in bone development and regeneration during osteoblast differentiation
[69]. The role of BMP signalling in polyphenol-mediated bone anabolism has been extensively studied, and several studies have shown that increasing BMP-2 promoter activity and BMP-2 expression increases new bone formation
[70][71]. Propolis loaded implants increased the expression of BMP-2 and 7 at the surrounding tissue. This event occurs in parallel with a reduction in inflammatory cytokine expression, increased new bone development around the implant, and enhanced adhesion with the mandibular and implant
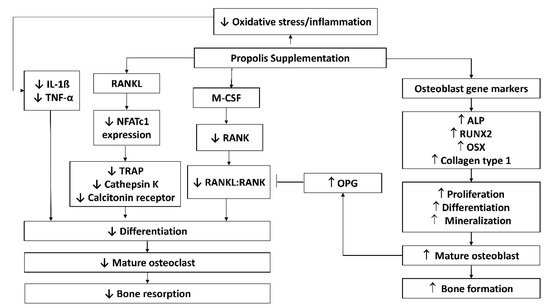
[62]. The possible molecular mechanisms of propolis are summarised in .
Figure 1. Possible molecular mechanisms of propolis in protecting against bone loss. Abbreviations: ALP, alkaline phosphatase; IL-1β, interleukin-1 beta; M-CSF, macrophage colony-stimulating factor; NFATc1, nuclear factor of activated T-cells; OPG, osteoprotegerin; OSX, osterix; RANK, receptor activator of nuclear factor-kappa B; RANKL, RANK ligand; TNF-α, tumour necrosis factor-alpha; TRAP, tartrate-resistant acid phosphatase.
Based on current evidence and the possible molecular mechanism, propolis has the potential to protect the skeletal system and improve bone remodelling by reducing the expression of inflammatory cytokines responsible for osteoclast differentiation and osteoblast apoptosis, inhibiting RANKL and M-CSF signalling pathway responsible for osteoclast differentiation and maturation and increasing osteoblast proliferation, differentiation, and mineralisation through its increased expression of osteoblast markers. These properties could be useful in the treatment of several medical conditions which promote bone loss or fractures. So far, propolis is already being considered in periodontal healthcare as there are existing clinical trials on the effect of propolis on periodontal health. However, there are no results available.
3. Bioavailability and Safety Concerns of Propolis
Propolis is made up of lipids, waxes, and resins in a complex matrix with a high molecular weight, contributing to its low absorption and bioavailability
[72]. The type of polyphenols present and their interactions dictate the synergistic effects and influence the bioavailability of propolis
[72]. Digestive instability, poor transcellular efflux in intestinal cells, as well as rapid metabolism and excretion are all thought to play a role in polyphenol bioavailability
[45]. Dietary polyphenols cannot be absorbed because they exist as esters, polymers, or glycosylated forms, and must be hydrolysed by intestinal enzymes or colonic microflora before absorption
[72]. Poorly absorbed polyphenolic compounds are converted to smaller phenolic acids with improved bioavailability in the intestinal system, owing to the colonic microbiota enzyme activity
[73]. Inter-individuality in absorption and metabolism is important as individual microbiota differ. Despite the low absorption percentages of bio-accessible phenolic compounds in propolis, Yesiltas et al.
[74] reported that the recovered amounts detected in plasma were still high compared to other food materials like fruits and vegetables.
Propolis and its constituents are generally well-tolerated and non-toxic unless given in huge doses according to clinical studies in mice and humans
[44][75][76]. According to Dobrowolski et al.
[77], the median lethal dose (LD50) for various propolis sources ranged from 2 to 7.3 g/kg in mice, implying a healthy dosage of 1.4 to 70 mg/day for humans based on a safety factor of 1000. The LD
50 of propolis extract given to conscious mice was more than 7.34 g/kg, indicating that the product is generally safe
[78][79]. However, it should be noted that propolis toxicity and adverse events were rarely monitored in human trials. Hypersensitivity is a more common side effect of propolis, especially when applied topically, resulting in allergic reactions, swelling, dermatitis, and urticaria
[80]. Hsu et al.
[80] reported a patient presenting severe swelling of the throat and anaphylactic shock upon topical application of propolis. Severe side effects like laryngeal oedema and anaphylactic shock have been reported infrequently
[81] and are rarely attributed to propolis. Propolis sensitivities have been reported in 1.2–6.6% of people with dermatitis
[82]. Therefore, consumers should seek medical advice before taking propolis supplements or applying propolis products, despite its positive safety profile.