
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Ke-Vin Chang | + 1979 word(s) | 1979 | 2020-06-04 05:28:33 | | | |
| 2 | Catherine Yang | -3 word(s) | 1976 | 2020-06-09 04:02:56 | | |
Video Upload Options
High resolution ultrasound is an emerging tool for evaluation of neuromuscular diseases. It has been widely used in assessment of brachial plexus disorders. However, ultrasound imaging is user-dependent. It is not easy to master the nerve tracking technique on that region. In this regard, we would like share certain tips to help investigators scan the brachial plexus in a prompt and precise way.
All the US images in this manuscript were obtained using a 5–18-MHz linear transducer (HI VISION Ascendus, Hitachi, Japan).
Should We Start the Scanning Cranially?
Scanning of the BP is highly recommended to be initiated from the supraclavicular fossa [1]. This enhances the chances of recognition of BP, resembling a bunch of grapes, situated posterior to the subclavian artery (Figure 1A). Traditionally, physicians were advised to start scanning from the cranial part of the BP, e.g., C5 anterior ramus, after identifying its corresponding transverse processes in a horizontal plane (Figure 1B). While the transverse processes project to the horizontal plane, anterior rami course inferiorly and laterally as they leave the inter-tubercular grooves. The angle between the transverse processes and the extraforaminal anterior rami impedes clear visualization of both structures (Figure 1C). Therefore, novice users may have difficulty in identifying and visualizing the cranial part of the BP, as they will be focusing on distinguishing different bony configurations of the transverse process. Visualization of BP distally and tracing it proximally will avoid this difficulty altogether. In case of variations, cervical anterior rami may course anterior to the anterior scalene muscle or pierce the muscle belly instead of traveling inside the inter-scalene groove [2]. As such, extra attention is a prerequisite when using the caudal-to-cranial tracking technique (Figure 1D and Supplementary Video S1).
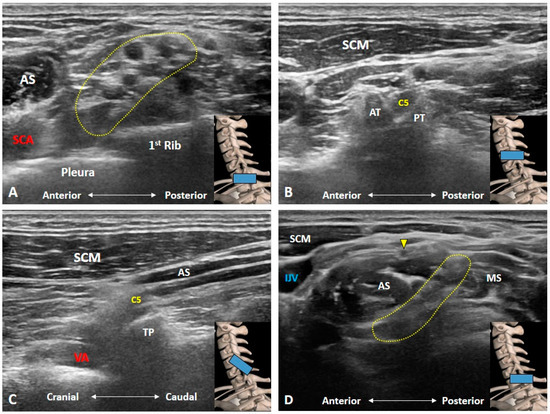
Figure 1. Ultrasound imaging of the brachial plexus. It resembles a bunch of grapes, situated posterior to the subclavian artery (A). The C5 anterior ramus is seen in its short-axis (B) and long-axis (C) views. In some variants, the C5 anterior ramus (yellow arrowhead) may course anterior to the anterior scalene muscle instead of the inter-scalene groove (D). AS: anterior scalene muscle; AT: anterior tubercle; IJV: internal jugular vein; MS: middle scalene muscle; PT: posterior tubercle; SCA: subclavian artery; SCM: sternocleidomastoid muscle; TP: transverse process; VA: vertebral artery. The yellow dashed area encircles the brachial plexus and the blue rectangles at the bottom-right corners represent the transducer position.
Is the C7 Transverse Process Easily Recognized?
Unlike the transverse processes of the C3 to C6 vertebrae, the C7 transverse process usually has only one posterior tubercle which is commonly used as a sonographic landmark to locate the C7 anterior ramus [3]. However, in certain cases, a rudimentary anterior tubercle might be visualized at the C7 transverse process (Figure 2A). Therefore, following the above stated caudal-to-cranial nerve tracking technique can effectively prevent misrecognition of the cervical anterior ramus level in such cases. However, the costal tubercle on the first rib may occasionally be mistaken as the posterior tubercle of the C7 transverse process (Figure 2B); swapping the transducer posteriorly and validating the first costotransverse joint (Figure 2C) help in differentiating the two. Alternately, one can confirm the attachment from the anterior and middle scalene muscles. Furthermore, if an echogenic shadow is visualized at the C7 level, a cervical rib should be highly suspected and swapping the transducer back and forth will clarify its connection with the C7 transverse process (Figure 3).
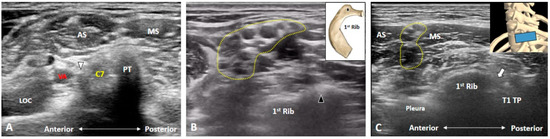
Figure 2. The C7 transverse process usually has only one posterior tubercle. In certain cases, a rudimentary anterior tubercle (white arrowhead) can be visualized (A). The costal tubercle (black arrowhead) on the first rib may be mistaken as the posterior tubercle of the transverse process (B). Swapping the transducer posteriorly to validate the first costotransverse joint (white arrow) helps differentiating the first rib from the C7 transverse process (C). AS: anterior scalene muscle; LOC: longus colli muscle; MS: middle scalene muscle; PT: posterior tubercle; TP: transverse process; VA: vertebral artery. The yellow dashed area encircles the brachial plexus and the blue rectangle represents the transducer position.
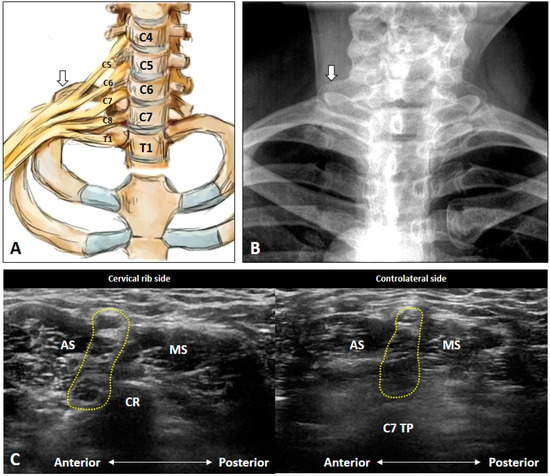
Figure 3. Schematic drawing (A), X-ray imaging (B) and ultrasound images (C) of the cervical rib (white arrows). AS: anterior scalene muscle; CR: cervical rib; MS: middle scalene muscle; TP: transverse process. The yellow dashed area encircles the brachial plexus.
How Can We Locate the C8 and T1 Roots?
The C8 anterior ramus emerges from the intervertebral foramen of C7/T1 and courses caudal to the C7 transverse process [3]. It can be easily depicted at the inter-scalene groove wherein the C5 to C8 anterior rami are arranged in a line between the anterior and middle scalene muscles with the C5 anterior ramus being most superficial and the C8 being the deepest (Figure 4A and Supplementary Video S2). Moreover, the C8 anterior ramus is cranial to the T1 transverse process coursing on top of the first rib. The T1 anterior ramus arises from the intervertebral foramen of T1/T2 and can be visualized distal and lateral to the inter-scalene groove. The transducer can be placed on the supraclavicular fossa to visualize the BP first and is then relocated more medially. The T1 anterior ramus can be found separate from the undersurface of the BP (inferior cord) submerging under the first rib (Figure 4B and Supplementary Video S2).
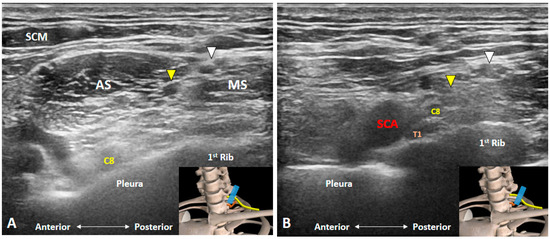
Figure 4. Ultrasound imaging of the C8 and T1 anterior rami. The C8 anterior ramus (A) is seen on top of the pleura at the bottom of the inter-scalene groove. T1 anterior ramus (B) can be visualized distal and lateral to the inter-scalene groove, emerging from the undersurface of the first rib. AS: anterior scalene muscle; MS: middle scalene muscle; SCA: subclavian artery; SCM: sternocleidomastoid muscle. White arrowheads: superior trunk; Yellow arrowheads: middle trunk. The blue rectangles at the bottom-right corners represent the transducer position.
How Can We Better Visualize Cervical Anterior Rami during the Scanning Process?
When we are trying to obtain a good quality US image, it is advised to position the target in the middle of the screen. This facilitates the examiner to be attentive to the primary focus as well as to appreciate better the whole regional anatomy. During the cervical anterior ramus imaging, it is important to know that the cervical spine has a lordotic curvature. Therefore, while sweeping the transducer from the cranial to the caudal aspect, movement should be gradual from posterior to anterior to locate the transverse processes of the cervical vertebrae in the center. However, if the transducer is merely moved vertically, certain anterior rami will fall at the edge of the scanning plane or might even become invisible.
Which Vascular Structure(s) Should We Be Aware Of?
At the supraclavicular portion of the BP, two vessels are noteworthy [3]. Transverse cervical artery emerging from the thyrocervical trunk and traversing posteriorly on top of or through the BP (Figure 4A and Figure 5A and Supplementary Video S4). The other vessel is the suprascapular artery, which is also a branch of thyrocervical trunk and courses beside the suprascapular nerve (Figure 5A and Figure 6B and Supplementary Video S4). Furthermore, the origin of the transverse cervical artery is closer to the root of the thyrocervical trunk than that of the suprascapular artery. Therefore, it is mostly seen coursing through the middle of the supraclavicular BP, whereas the suprascapular artery is usually visualized coursing above the supraclavicular BP.
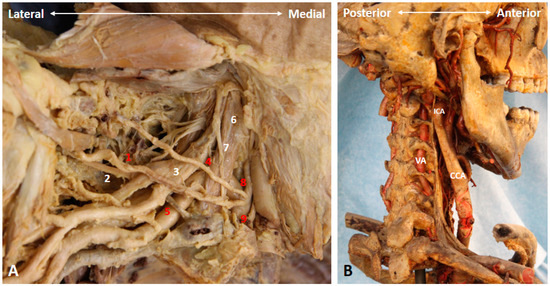
Figure 5. The transverse cervical artery, thyrocervical trunk, suprascapular artery and nerve (A), as well as the course and relevant vasculature of the vertebral artery (B) in a cadaver model. 1: suprascapular artery; 2: suprascapular nerve; 3: superior trunk; 4: transverse cervical artery; 5: subclavian artery; 6: anterior scalene muscle; 7: phrenic nerve; 8: inferior thyroid artery; 9: thyrocervical trunk. CCA: common carotid artery; ICA: internal carotid artery; VA: vertebral artery. Red numbers indicate arteries, while the white numbers indicate nerves and muscles.
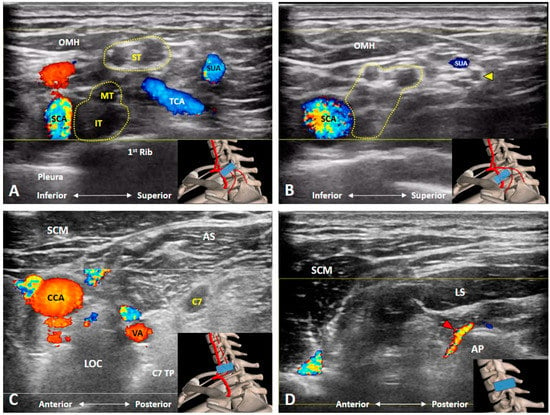
Figure 6. Doppler ultrasound imaging of the transverse cervical artery, thyrocervical trunk (A), suprascapular artery and nerve (B), vertebral artery (C), and radicular artery (D). AP: articular pillar; AS: anterior scalene muscle; CCA: common carotid artery; IT: inferior trunk; LOC: longus colli muscle; LS: levator scapulae muscle; MT: middle trunk; OMH: omohyoid muscle; SCA: subclavian artery; SCM: sternocleidomastoid muscle; ST: superior trunk; SUA: suprascapular artery; TCA: transverse cervical artery; VA: vertebral artery. Yellow arrowhead: suprascapular nerve; Red arrowhead: radicular artery. The yellow dashed area encircles the brachial plexus, and the blue rectangles in the bottom-right corners represent the transducer position.
Likewise, at the cervical root level, two vessels require extra attention [1]. The vertebral artery (branch of the subclavian artery) usually enters the transverse foramen over the C6 transverse process. At the level of C7, it is just anterior to the C7 anterior ramus (Figure 5B and Figure 6C). Of note, both structures may look similar without the use of Doppler US imaging. Additionally, during US-guided cervical anterior ramus injection, the needle is suggested to be introduced from posterior to anterior for preventing injury to the vertebral artery [4]. The second vessel to be precisely recognized is the radicular artery, which might be arising from the ascending and deep cervical arteries and entering the intervertebral foramen from the articular pillars [5]. Since it is mostly located posterior to the corresponding cervical anterior ramus, the examiner should be cautious if a posterior-to-anterior approach is used while they perform the cervical root injection (Figure 6D).
Which Branches of the BP Can Be Seen in the Cervical Region?
Three branches of the BP can be visualized at this level. First of which is the dorsal scapular nerve emerging from the posterior aspect of the C5 anterior ramus [1]. As it pierces the medial scalene muscle (Figure 7 and Figure 8A) and further courses underneath the levator scapular muscle (Figure 8B and Supplementary Video S5 ), the transducer is suggested to be placed along the transection of the middle scalene muscle to retrieve better the short-axis view of the nerve. In certain variants, the dorsal scapular nerve pierces the anterior or posterior scalene muscle [6]. This nerve should be cautiously located and avoided when performing an US-guided C5 anterior ramus injection.
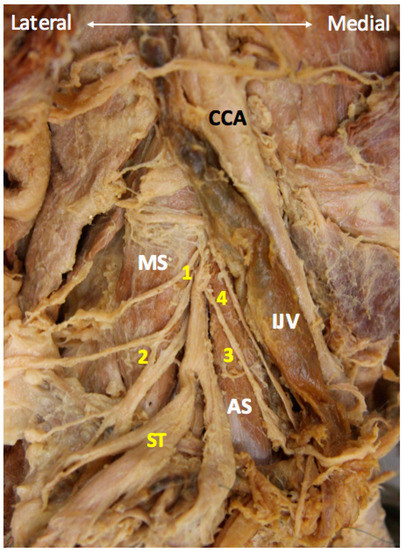
Figure 7. The long thoracic and dorsal scapular nerves cadaveric models. 1: dorsal scapular nerve; 2: long thoracic nerve; 3 phrenic nerve; 4: vagus nerve. AS: anterior scalene muscle; CCA: common carotid artery; IJV: internal jugular vein; MS: middle scalene muscle; ST: superior trunk.
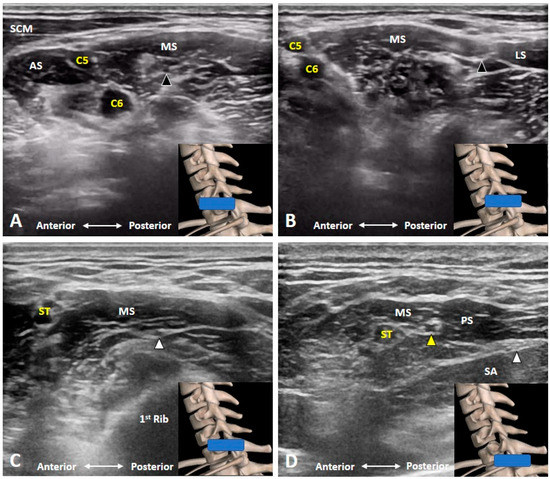
Figure 8. The dorsal scapular nerve (black arrowhead) emerges from the C5 anterior ramus, pierces the medial scalene muscle (A) and further courses underneath the levator scapulae muscle (B). The long thoracic nerve (white arrowhead) also travels inside the middle scalene muscle (C). The suprascapular nerve (yellow arrowhead) branches from the superior trunk of the brachial plexus (D). AS: anterior scalene muscle; LS: levator scapulae muscle; MS: middle scalene muscle; PS: posterior scalene muscle; SCM: sternocleidomastoid muscle; ST: superior trunk; SA: serratus anterior muscle. The blue rectangles at the bottom-right corners represent the transducer position.
The second branch is the long thoracic nerve receiving fibers from the C5, C6 and C7 anterior rami [7]. Like the dorsal scapular nerve, it also traverses within the middle scalene muscle in most cases. However, it may pierce the anterior scalene or posterior scalene muscle in some variants [6]. As such, the transducer can be positioned along a similar but slightly inferior scanning plane as in the dorsal scapular nerve. To distinguish the two nerves, the transducer is needed to be swapped back and forth to ensure that one rootlet of the long thoracic nerve is derived from C6 or C7 anterior rami (Figure 8C and Supplementary Video S6). The nerve should be avoided during an US-guided interscalene block.
The third branch is the suprascapular nerve from the superior trunk of the BP [8]. Scanning can start from the C5 anterior ramus and gradually moving the transducer laterally until the C5 and C6 anterior rami merge to become the superior trunk. The suprascapular nerve usually emerges from the posterior aspect of the superior trunk (Figure 8D), whereas the anterior and posterior divisions are branched off from its anterior aspect.
References
- Chang, K.V.; Lin, C.P.; Hung, C.Y.; Ozcakar, L.; Wang, T.G.; Chen, W.S.; Sonographic nerve tracking in the cervical region: A pictorial essay and video demonstration. Am. J. Phys. Med. Rehabil. 2016, 95, 862–870.
- Vanessa Leonhard; Riley Smith; Gregory Caldwell; Heather F. Smith; Riley Landreth; Anatomical variations in the brachial plexus roots: implications for diagnosis of neurogenic thoracic outlet syndrome. Annals of Anatomy - Anatomischer Anzeiger 2016, 206, 21-26, 10.1016/j.aanat.2016.03.011.
- Chang, K.V.; Kara, M.; Su, D.C.; Gurcay, E.; Kaymak, B.; Wu, W.T.; Ozcakar, L.; Sonoanatomy of the spine: A comprehensive scanning protocol from cervical to sacral region. Med. Ultrason. 2019, 21, 474–482.
- Ke-Vin Chang; Wei-Ting Wu; Levent Özçakar; Ultrasound-Guided Interventions of the Cervical Spine and Nerves. Physical Medicine and Rehabilitation Clinics of North America 2018, 29, 93-103, 10.1016/j.pmr.2017.08.008.
- Finlayson, R.J.; Etheridge, J.P.; Chalermkitpanit, P.; Tiyaprasertkul, W.; Nelems, B.; Tran, D.Q.; Huntoon, M.A.; Real-time detection of periforaminal vessels in the cervical spine: An ultrasound survey. Reg. Anesth. Pain Med. 2016, 41, 130–134.
- Williams, A.A.; Smith, H.F.; Anatomical entrapment of the dorsal scapular and long thoracic nerves, secondary to brachial plexus piercing variation. Anat. Sci. Int. 2020, 95, 67–75.
- Ke-Vin Chang; Wei-Ting Wu; Kamal Mezian; Ondřej Naňka; Levent Özçakar; Sonoanatomy revisited: the long thoracic nerve. Medical Ultrasonography 2019, 21, 349-352, 10.11152/mu-1952.
- Ke-Vin Chang; Kamal Mezian; Ondřej Naňka; Wei-Ting Wu; Chih-Peng Lin; Levent Özçakar; Ultrasound-guided interventions for painful shoulder: from anatomy to evidence. Journal of Pain Research 2018, 11, 2311-2322, 10.2147/JPR.S169434.




