
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Yuman Lee | + 1755 word(s) | 1755 | 2021-07-12 10:43:08 | | | |
| 2 | Conner Chen | Meta information modification | 1755 | 2021-07-15 07:51:33 | | |
Video Upload Options
Beta-lactam antibiotics are considered a first-line therapy in many bacterial infections and include agents such as penicillins, cephalosporins and carbapenems. However, beta-lactam antibiotics are a common cause of adverse drug reactions and are associated with high rates of antibiotic allergy. Unverified beta-lactam allergies are a substantial public health problem, as the majority of patients labeled as beta-lactam allergic do not have clinically significant allergies that may hinder the use beta-lactam therapy when indicated. Outdated or inaccurate beta-lactam or penicillin allergies can result in serious consequences, including suboptimal antibiotic therapy, increased risk of adverse effects, and use of broader spectrum antibiotics than indicated, which may contribute to antimicrobial resistance.
1. Beta-Lactam Allergy Overview
1.1. Pathophysiology
Beta-lactam allergies are hypersensitivity reactions that are the consequence of an adaptive immune response. Of the four reaction types described in Table 1, penicillin allergies most often present as type I or type IV hypersensitivity reactions [1]. Type I hypersensitivity reactions are triggered by the interaction of an allergen with allergen-specific IgE bound to mast cells, basophils, and eosinophils. This interaction causes the cells to degranulate and release a potent mixture of histamine and inflammatory mediators [2]. In response to histamine and other inflammatory mediators, there is an increase in vascular permeability and a widespread constriction of smooth muscle, which can ultimately lead to anaphylactic shock [2]. Type I reactions are immediate in nature and may result in symptoms such as urticaria, flushing, dyspnea, bronchospasm, angioedema, hypotension, tachycardia, altered mental status or gastrointestinal upset [1].
Table 1. Classification of hypersensitivity reactions [1][3][2][4].
| Hypersensitivity Type | Reaction Type | Time of Onset | Examples |
|---|---|---|---|
| Type I | IgE-mediated | Within 1 h | Anaphylaxis, bronchospasm |
| Type II | Non-IgE-mediated, Cytotoxic | Several hours to days | Hemolytic Anemia |
| Type III | Non-IgE-mediated, Immune Complex | 7 days to 21 days | Serum Sickness |
| Type IV | Non-IgE-mediated, Cell-mediated | Days to weeks | Maculopapular rash, SJS, TEN, DRESS * |
* Stevens–Johnson syndrome (SJS), toxic epidermal necrolysis (TEN) or drug rash with eosinophilia and systemic symptoms (DRESS).
Because all penicillin antibiotics share a similar beta-lactam core ring structure, one must consider the potential for cross-allergenicity between different agents in the beta-lactam class. When a beta-lactam is administered, the common core ring structure is metabolized into major and minor antigenic determinants. The major determinant is penicilloyl, and the minor determinants include penicillin, penicilloate, and penilloate [1]. In patients with beta-lactam allergy, the minor antigenic determinants generate IgE-specific responses associated with type I allergy. The major antigenic determinant is more commonly associated with less severe urticarial reactions [1]. In addition to a core ring structure, beta-lactams have various side chains, which can also result in type I allergic reactions [1]. Type I reactions to beta-lactam antibiotics are individualized and have effects of varying severity.
Less frequently, beta-lactam allergies may present as other types of hypersensitivity reactions. Type II hypersensitivities are less severe, but can be caused by an IgG response to small molecules like penicillin that become covalently bound to the outside surface of cells. The chemical reaction modifies the structures of human cell surface components, which become perceived as foreign antigens by the immune system. B cells are stimulated to make IgG antibodies against the new epitopes. On binding to their specific cell-surface antigens, the antibodies cause the modified human cells to become subject to complement activation and phagocytosis, resulting in inflammation and damaged tissue [2].
Type III hypersensitivities involve small, soluble, immune complexes of antigen and specific IgG, forming deposits in the walls of small blood vessels or the alveoli of the lungs. At these sites, the immune complexes activate complement and an inflammatory response that damages the tissue and impairs its function. Typically, type III hypersensitivities are not associated with beta-lactam exposure [3].
Type IV hypersensitivities are caused by CD4 T-cells responding to the epitopes of foreign proteins or to peptides derived from chemically modified human proteins [2]. The result is typically cutaneous reactions such as a maculopapular rash or urticarial eruption. Although rare, severe reactions, such as Stevens–Johnson syndrome (SJS), toxic epidermal necrolysis (TEN) or drug rash with eosinophilia and systemic symptoms (DRESS) may occur as a result of a type IV hypersensitivity. Type IV hypersensitivities are delayed in nature, occurring several days to weeks after the last administered dose, and have been associated with beta-lactam allergy [4].
1.2. Risk Factors
Although data are currently limited in regard to the risk factors for a beta-lactam allergy, there is speculation about a correlation between the clinical and genetic risk factors of self-reported penicillin allergy. A recent case-control study identified factors such as having a family history of penicillin allergy or an IL-4 gene single nucleotide polymorphism as possible risk factors of penicillin allergy. [5] Another recent study found that HLA-DRB1*10:01 predisposed patients to an immediate hypersensitivity reaction [6]. Furthermore, other studies suggest a greater risk of penicillin allergy in females and a greater risk of beta-lactam allergy in those with a history of a prior adverse reaction to penicillin [7][8].
1.3. Cross-Allergenicity
As noted earlier, all beta-lactam antibiotics share a similar chemical core ring structure. This core ring consists of a beta-lactam ring attached to a five- or six-membered ring. In addition to this core structure, beta-lactams have side chains (R1 and R2) that vary between the specific agents [9]. Because of the common core ring structure among beta-lactam antibiotics and the potential similarities in side-chains, there is a risk for cross-allergenicity among the different beta-lactam classes. Knowledge and understanding of the risk of beta-lactam cross-allergenicity plays an important role in selecting the appropriate antibiotic therapy for a patient with a beta lactam allergy. The rates of cross-allergenicity between penicillin and other beta-lactams can be found in Table 2.
Table 2. Beta-lactam cross-reactivity [9][10][11][12][13][14].
| Beta-Lactam | Rate of Cross-Reactivity with Penicillins | Examples of Agents with Identical Side Chains |
|---|---|---|
| 1st generation cephalosporins | ~2% | Ampicillin, cephalexin, cefaclor |
| Later generation cephalosporins | ≤1% | Amoxicillin, cefadroxil, cefprozil |
| Carbapenems | ≤1% | - |
| Monobactams | none | Aztreonam. ceftazidime |
2. Approach to Management
2.1. Initial Allergy Assessment
The initial management of patients with a history of beta-lactam allergy requires a detailed allergy assessment, given that many patients are inappropriately labeled as beta-lactam allergic. Oftentimes, known adverse effects of a beta-lactam are mislabeled and documented as a beta-lactam allergy. Approximately 90% of patients labeled as allergic can be de-labeled through a detailed allergy assessment or allergy testing [16][17]. The appropriate assessment of beta-lactam allergy includes the evaluation of factors such as the specific agent causing the reaction, the type, severity, and timing of the reaction, and previous tolerability of other beta-lactam agents. The de-labeling of penicillin allergy, based on historical evaluation alone, has been demonstrated to be safe and effective in patients reporting a mild, non-immune-mediated adverse drug reaction, or where subsequent tolerance to the implicated penicillin has been identified through their medical or pharmacy records [16]. Figure 1 includes a list of questions that may be appropriate to ask patients who report a beta-lactam allergy.
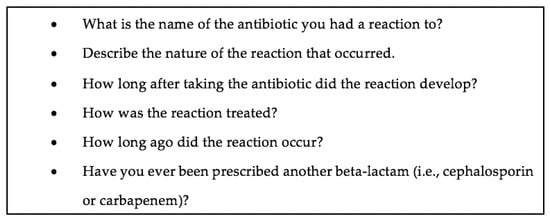
Figure 1. Sample allergy assessment questions.
Additionally, a direct oral challenge may be an effective option in de-labeling patients with low-risk penicillin allergies and has been used in both the inpatient and outpatient setting. Direct oral challenges offer a means to de-labeling penicillin allergies in patients who are low risk or have an inaccurate allergy label without having to pursue traditional allergy testing. Appropriate risk stratification is needed to ensure the safety of a direct oral challenge; however, no standard criteria to determine low-risk allergy patients has been established. Factors such as reaction type, onset of allergy symptoms, and severity have been utilized to determine risk. Validated allergy phenotyping tools may be used to identify low-risk allergy patients and help to facilitate de-labeling when appropriate [18].
2.2. Penicillin Skin Testing
In patients with ambiguous allergy histories, or those reporting allergies that are severe in nature, additional steps should be taken to determine the nature of their allergy and whether a beta-lactam can safely be administered. Penicillin skin testing (PST) is a safe and effective means of evaluating a penicillin allergy in these patients. It is used to detect the presence of penicillin-specific IgE and predicts the likelihood of a type I allergic reaction to penicillin [19]. PST is indicated in patients with documented or suspected type I clinical penicillin hypersensitivity. Patients with a history of desquamating type IV hypersensitivity reactions, such as SJS, TEN, or DRESS or other non-IgE-related hypersensitivity, are not candidates for PST [18]. Implementing PST requires the consideration of several logistical factors such as the development of policies and protocols, specialized training for staff, storage and preparation of PST components, and determining whether PST should be offered in the inpatient versus outpatient setting [20].
PST involves epicutaneous skin testing, followed by intradermal testing, and is conducted using degradation products of penicillin, known as major and minor determinants. PST offers a negative predictive value of 97–99% [21] and a positive predictive value of approximately 50% [22].
In patients who have a negative PST, a test dose of the beta-lactam to which the patient reported allergy should be administered in order to confirm the absence of an allergy. The patient should then be observed for 1–2 h after the test dose to confirm no immediate reaction occurs. If no reaction occurs after the observation period, the patient can receive the beta-lactam and should have their allergy information updated accordingly.
References
- Patterson, R.A.; Stankewicz, H.A. Penicillin Allergy. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2020. Available online: (accessed on 2 January 2021).
- Parham, P. The Immune System, 4th ed.; Garland Science, Taylor & Francis Group, LLC: New York, NY, USA, 2021.
- Jones, B.M.; Jozefczyk, C.; Maguire, C.; Milliken, S.; Weisz, E.E.; Bland, C.M. Beta-lactam Allergy Review: Implications for Antimicrobial Stewardship Programs. Curr. Treat. Options Infect. Dis. 2019, 11, 103–114.
- Shenoy, E.S.; Macy, E.; Rowe, T.; Blumenthal, K.G. Evaluation and Management of Penicillin Allergy. JAMA 2019, 321, 188–199.
- Apter, A.J.; Schelleman, H.; Walker, A.; Addya, K.; Rebbeck, T. Clinical and genetic risk factors of self-reported penicillin allergy. J Allergy Clin Immunol. 2008, 122, 152–158.
- Nicoletti, P.; Carr, D.F.; Barrett, S.; McEvoy, L.; Friedmann, P.S.; Shear, N.H.; Nelson, M.R.; Chiriac, A.M.; Blanca-López, N.; Cornejo-García, J.A.; et al. Beta-lactam-induced immediate hypersensitivity reactions: A genome-wide association study of a deeply phenotyped cohort. J. Allergy Clin. Immunol. 2021, 147, 1830–1837.e15.
- Park, M.A.; Matesic, D.; Markus, P.J.; Li, J.T.-C. Female sex as a risk factor for penicillin allergy. Ann. Allergy Asthma Immunol. 2007, 99, 54–58.
- Kelkar, P.S.; Li, J.T. Cephalosporin allergy. N. Engl. J. Med. 2001, 345, 804–809.
- Zagursky, R.J.; Pichichero, M.E. Cross-reactivity in β-Lactam Allergy. J. Allergy Clin. Immunol. Pract. 2018, 6, 72–81.e1.
- Krey, S.C.; Waise, J.; Skrupky, L.P. Confronting the Challenge of Beta-Lactam Allergies: A Quasi-Experimental Study Assessing Impact of Pharmacy-Led Interventions. J. Pharm. Pr. 2017, 32, 139–146.
- Chaudhry, S.B.; Veve, M.P.; Wagner, J.L. Cephalosporins: A Focus on Side Chains and β-Lactam Cross-Reactivity. Pharmacy 2019, 7, 103.
- Kula, B.; Djordjevic, G.; Robinson, J.L. A systematic review: Can one prescribe carbapenems to patients with IgE-mediated allergy to penicillins or cephalosporins? Clin. Infect. Dis. 2014, 59, 1113–1122.
- Gaeta, F.; Valluzzi, R.L.; Alonzi, C.; Maggioletti, M.; Caruso, C.; Romano, A. Tolerability of aztreonam and carbapenems in patients with IgE-mediated hypersensitivity to penicillins. J. Allergy Clin. Immunol. 2015, 135, 972–976.
- Lee, Y.; Bradley, N. Overview and Insights into Carbapenem Allergy. Pharmacy 2019, 7, 110.
- Gueant, J.L.; Gueant-Rodriguez, R.M.; Viola, M.; Valluzzi, R.L.; Romano, A. IgE mediated hypersensitivity to cephalosporins. Curr. Pharm. Des. 2006, 12, 3335–3345.
- Chua, K.Y.L.; Vogrin, S.; Bury, S.; Douglas, A.; E Holmes, N.; Tan, N.; Brusco, N.K.; Hall, R.; Lambros, B.; Lean, J.; et al. The Penicillin Allergy Delabeling Program: A Multicenter Whole-of-Hospital Health Services Intervention and Comparative Effectiveness Study. Clin. Infect. Dis. 2020.
- Trubiano, J.; Phillips, E. Antimicrobial stewardship’s new weapon? A review of antibiotic allergy and pathways to “de-labeling”. Curr. Opin. Infect. Dis. 2013, 26, 526–537.
- Rose, M.T.; Salvin, M.; Trubiano, J. The democratization of de-labeling: A review of direct oral challenge in adults with low-risk penicillin allergy. Expert Rev Anti Infect Ther. 2020, 18, 1143–1153.
- Yates, A.B. Management of Patients with a History of Allergy to Beta-Lactam Antibiotics. Am. J. Med. 2008, 121, 572–576.
- Bland, C.M.; Bookstaver, P.B.; Griffith, N.C.; Heil, E.L.; Jones, B.M.; Justo, J.A.; Staicu, M.L.; Torney, N.P.; Wall, G.C. A practical guide for pharmacists to successfully implement penicillin allergy skin testing. Am. J. Health Pharm. 2019, 76, 136–147.
- Rimawi, R.H.; Cook, P.P.; Gooch, M.; Kabchi, B.; Ashraf, M.S.; Rimawi, B.H.; Gebregziabher, M.; Siraj, D.S. The impact of penicillin skin testing on clinical practice and antimicrobial stewardship. J. Hosp. Med. 2013, 8, 341–345.
- Sogn, D.D.; Evans, R.; Shepherd, G.M.; Casale, T.B.; Condemi, J.; Greenberger, P.A.; Kohler, P.F.; Saxon, A.; Summers, R.J.; VanArsdel, P.P.; et al. Results of the National Institute of Allergy and Infectious Diseases Collaborative Clinical Trial to Test the Predictive Value of Skin Testing with Major and Minor Penicillin Derivatives in Hospitalized Adults. Arch. Intern. Med. 1992, 152, 1025–1032.




