
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Marco Socci | + 3634 word(s) | 3634 | 2021-06-26 11:39:53 | | | |
| 2 | Conner Chen | Meta information modification | 3634 | 2021-07-09 05:01:18 | | |
Video Upload Options
According to the World Health Organization (WHO), dementia is one of the more serious challenges of the future . Most countries have a variety of policies, institutions and financial aids implemented to ease the burden on families carrying out the bulk of care work for their relatives with dementia. However, due to the COVID-19 outbreak, some of these support systems have become much more difficult (or even impossible) to access or utilize, an effect mediated by the mandatory stringency measures adopted by governments during the first wave of the pandemic to mitigate its impact on the population. Both Italy and Hungary belong to clusters of countries showing challenges concerning the degree of resilience. However, Italy is part of a cluster having weak resilience in informal care and moderate resilience in formal care provision, while Hungary belongs to a cluster with weak resilience in both formal and informal care (i.e., with a higher share of older adults reporting difficulties in receiving formal care—i.e., home care—and a quite low share receiving informal care from people outside their home, being the supply of both types of care provision dramatically decreased compared to the pre-pandemic period).
1. Family Carers of Older People Living with Dementia
At present, around 50 million people live with dementia worldwide, and there are nearly 10 million new cases every year. The total number of people with this disorder is projected to reach 82 million in 2030, and 152 million in 2050. The estimated proportion of the population aged 60 and over with dementia at any given time is between 5–8 per cent [1]. Dementia ranges from mild (early stage) to severe (late stage), with the probability of a more severe stage increasing substantially with age, each stage requiring different types of care and services, according to their mental health needs [2][3].
Many studies highlighted that dementia care systems rely on work carried out by family carers [2][3], since a significant proportion of older people with dementia live at home, and are informally cared for (mostly by the women in their families) [4].
Dementia can be a great burden on families tasked with care responsibilities, often causing physical and emotional stress and financial problems [5]. Caregivers of people with dementia are more burdened than the caregivers of people with other diseases [6][7], and often experience high levels of anxiety, depression, stress, morbidity, physical problems and low quality of life [8][9]. In Italy, the burden of dementia caregivers appears to be especially heavy, with an average of 4.4 h of direct assistance and 10.8 h of supervision needed per day. This commitment has consequences on the caregivers’ personal and social life, and on their ability to work (the number of unemployed caregivers tripled since 2006, with those still working reporting repeated absences and, especially in the case of women, only being able to work part-time). Balancing care and paid work is also a difficulty family caregivers face [10][11]. Negative effects on health include feeling tired, lack of rest, and showing symptoms of depression [12][13], resulting in family caregivers being considered as the “hidden secondary patients” [14].
2. Changes Brought on by the COVID-19 Pandemic
The COVID-19 pandemic has affected the lives of people throughout the world. One of the population groups most affected by the still ongoing pandemic was that of frail older people [15], particularly those in very old age segments, among whom incidence rates of dementia are high [16]. Family carers were hit by the sudden removal of social support services, and this increased their burden substantially; they also reported concerns about when services would re-open [17]. A number of research papers focused on the diminishing sources of support in the first wave of the pandemic, and the challenges faced by carers. In the United Kingdom (UK), Barry and Hughes [18] appealed for support for family carers and healthcare professionals treating older people with dementia, as they have a critical role in the management of medicine intake. In Austria, due to a reduction in available therapies and support (e.g., rehabilitative) services for older people in need of care, symptoms of people cared for (including those with dementia) worsened, leading to an increased burden for family carers [19]. Vaitheswaran et al. [20] carried out a qualitative telephone survey in India with 31 caregivers of people living with dementia. Some respondents reported a need for immediate and others for long-term support during the pandemic, and they suggested methods to meet their needs, such as the use of video consultations, telephone-based support, clinic-based in-person visits and post-pandemic services. Lack of outpatient rehabilitation services and increased stress for family caregivers was found in Argentina [21]. Tsapanou et al. [22] reported that due to the limitation of available support sources, caregivers in Greece experienced a great increase in their psychological and physical burden. Simultaneous work commitments and growing care responsibilities were also challenging for Irish family members during the pandemic [23]. Other studies on COVID-19 seem to confirm a deterioration in well-being as a result of an increased burden as carers step in to fill in care gaps [24][25].
Another research focus was the change in the role of the caregiver paid by the family, e.g., in Argentina [21]. Many families decided to discontinue paid carers entering the home due to the risk of infection, resulting in unpaid carers having to put in the care hours to support the person living with dementia [26]. According to the Alzheimer Society of Ireland, 77 per cent of family carers of people with dementia experienced an increase in the level of care they provide as they were forced to step in instead of the usually available care support. The fear of spreading the disease while assisting patients with instrumental activities was a major concern [27].
Even research that did not originally focus on family carers of older people with dementia unearthed some new information on the topic. In Hungary, Tróbert et al. [28] carried out an online survey among family carers of older people. They found that the burden of those caring for someone with dementia in their home increased significantly during lockdown, compared to those whose care recipient was unaffected by the disease.
Apart from its devastating effects, the pandemic also brought on a few positive changes in the care work carried out by families. In Spain, Goodman-Casanova et al. [29] found that telehealth could support adults with mild cognitive impairment/dementia living at home. Cuffaro et al. [30] pointed out that in Italy the pandemic is speeding up the use of telemedicine and digital technology in the care of people with dementia. Home-based care for people with Alzheimer’s disease and related dementias was the focus of Sm-Rahman et al. [31], who overviewed challenges specific to this group and their carers, and proposed solutions to these challenges on the structural and personal level. During the first months of the pandemic, remote interventions were also developed and refined in Italy [32], which helped identify risk situations, monitor the condition of people with dementia, provide support to caregivers, and ensure communication between patients, caregivers and health and social workers involved in the care network. The pandemic therefore contributed to the adoption of reliable and sustainable remote interventions, which could be an opportunity in the future to improve and simplify the process of taking charge and promoting continuity of care. In Hungary, the implementation of the e-receipt system made it easier to get prescriptions for necessary medication over the phone, which reduced doctor-patient encounters for examinations and medical interventions.
3. Dementia-Related Health and Social Services Supporting Older People with Dementia Living at Home
3.1. Italy
Around 1.3 million people were estimated to have dementia in Italy in 2018, representing 2.1% of the population, and 9% of those aged 65 or over [33]; about 80% are assisted directly by a family member [12].
With regard to support services, home healthcare in Italy (Assistenza Domiciliare Integrata or ADI) is funded by the National Health Service, and includes health services at home (home nursing, physiotherapy, specialist and doctors’ visits) to limit functional decline and to improve the quality of life of the person with dementia within the family environment, avoiding, as far as possible, hospitalization or care in a residential facility. Only 9.5 per cent of older people with dementia receive assistance via home healthcare [12]. The number of hours of care per recipient per year is 20 on average, showing the limitations of this public service [34]. Home care (Servizio di Assistenza Domiciliare, SAD) is provided and funded by the municipality, and consists of personal hygiene care and meals on wheels provided to non-self-sufficient older persons. Users partly pay for the service on an income basis and can receive a voucher from local authorities to be used for covering service costs.
SAD is considered inadequate to cover the daily needs of both people with dementia and their caregivers. Interventions represent a drop in the ocean since, regardless of need, solutions offered are always the same (services carried out during the day), while the overall management of the situation rests with the family or remains precarious [35]. Moreover, the service is extremely variable across Italian regions. The integration between home healthcare (ADI) and home care (SAD) is envisaged by regulation, but it has never been defined nationally, remaining a regional responsibility according to the division of competences between the national and regional level (i.e., health and social services planning and organisation is regulated on a regional level). Therefore, healthcare and social services (e.g., ADI and SAD), as well as social and health facilities for people with dementia like day care centres, are differently supplied among Italian areas (e.g., mostly in the North), and are only managed on an integrated basis in some regions [36]. The Italian long-term care (LTC) system also includes a care allowance element (indennità di accompagnamento), which amounted to EUR 520.29 per month in 2020. This cash-for-care benefit is intended to support the choice of keeping non-self-sufficient older persons at home, in their usual social and emotional environment—in line with the Italian “familistic” culture—as an alternative to permanent placement in a protected residence. The benefit mainly aims to co-fund the payment of private home helpers. Approximately 38 per cent of Italian families caring for their relatives with dementia are able to employ non-professional carers, mainly migrant care workers [12]. Migrant care workers are particularly relevant to older people with higher care needs, e.g., people with dementia, albeit their employers usually come from higher socio-economic backgrounds [37][38]. Cash-for-care allowances have resulted in families outsourcing care services to migrant paid carers [38]. However, only about one-third of those who have the help of a migrant paid carer receive public contributions, most of them in the form of a care allowance. The other two-thirds cover the cost of private assistance from the family budget. Due to this huge expense averaging EUR 800 per month, the majority of family carers (56%) reported having to make changes to make ends meet: 48% reduced consumption in order to keep the employee, 20% had to dip into their savings, and 3% of households even had to go into debt [12].
The official number of migrant care workers (the so-called “badanti”) stood at 407,000 in 2019 [39], which is only a fraction of the actual figures as this sector is heavily characterized by informal/undeclared work in Italy. This means that the sheer number of migrant care workers alone makes them an important stakeholder in dementia care in Italy. However, countries utilizing migrant healthcare workers tend not to even recognize the contribution and importance of skilled migrant healthcare workers at policy level [40], and “badanti” in Italy similarly remain largely absent in policy debates.
The dementia care voucher is another element of integrated health and social care and is provided by local health and social services. The purpose of the voucher is to help families adequately manage needs at the early stage of dementia, allowing for the acquisition of a psycho-educational intervention for the caregiver and family members. This benefit is not dispensed evenly throughout the country. Services supporting the family are the Alzheimer Day centres, consisting in semi-residential care facilities offering respite to the family, and providing cognitive stimulation to older persons living with dementia. Although these centres represent an essential level of assistance that each region must guarantee to older adults with dementia [41], in reality they are only available to 12.5% of families [12].
The Italian care model, based on a low supply of services and a high diffusion of the care allowance (used mostly as a contribution to the cost of paid family assistants, mainly “badanti”), places most of the responsibility on families to organize assistance for their relatives with dementia, acting, in most cases, as their own “case manager”. This setup requires direct commitment from families to care for their frail older members, as well as a significant economic effort. Family carers who are employed in Italy can request three days of paid leave per month, and two years unpaid leave. However, working carers find it difficult to combine paid work and caring responsibilities in many cases, since companies (especially small and medium enterprises) do not always provide work-life balance measures, such as flexible working time arrangements.
3.2. Hungary
Between 146,000 [33] and 250,000 [42] people were estimated to have dementia in Hungary in 2018, representing 1.5% of the population and 7.4% of those aged 65 or over (Alzheimer Europe 2019). The total number of family carers is estimated to be between 400,000–500,000 [42].
Social care in Hungary is regulated by the Social Welfare Act of 1993 [43], which divides services into basic and specialist care. All local governments have the mandatory task of providing home help to older people. This includes the following categories: home help/care (maximum four hours a day) such as cleaning, shopping, administration, medicine administration, delivering food, and conversation; alarm system-based home help (a device to be used for emergency calls to social services); meals on wheels (one hot meal a day); and access to services in villages with less than 600 inhabitants, and parts of the country where houses (mostly farms) are isolated from nearby settlements. Local governments covering over 3000 inhabitants are also obliged to provide a specialist service (day care centre for older people) [44]. Day care centres specifically for dementia patients are not very common, although their numbers are increasing.
Residential settings, nursing homes and respite care services are not part of the basic social care system for older people, and their number is low. These institutions are either private, public, or belong to churches or non-governmental organizations.
Apart from various types of pensions and benefits, the only financial aid available to family carers is the nursing fee. This social benefit amounted to around EUR 81.42 per month in 2020 (11.5% of the average monthly wage) and is insufficient to be of any meaningful help towards increased living expenses. The nursing fee’s main target group is not family carers of older people, but those caring for disabled children.
Some services (especially home nursing) are available through the healthcare system, which is regulated by the Healthcare Act of 1997 [45]. Generally, the healthcare and social care systems are not harmonized. They work on different principles and communication between professionals working in the two fields is insufficient, even when justified by the interests of the user. Home nursing financed by health insurance is a short-term support (14 days, with an option to be extended to a maximum of 56 days). Getting a family member diagnosed with dementia is a very difficult process, and information is lacking.
According to estimates, less than half the people living with dementia have access to any kind of health or social service [42]. Due to the care deficit and inadequacy of the nursing fee, family carers who are not already retired are usually forced to remain in the labour market even if they are full-time carers. Employed family carers are entitled to a maximum of two years of unpaid leave from work.
There is no official data on the number of migrant care workers in the Hungarian LTC system, although it is known from qualitative studies that informal caregivers coming from the Hungarian minorities of neighbouring Romania and Ukraine do provide live-in care for frail older people, including those with dementia [46].
4. Severity of Health Crisis and Public Measures Implemented to Face the Pandemic
Figure 1 shows new coronavirus-related deaths in Italy and Hungary (three-day smoothing window) between January and July 2020 [5].
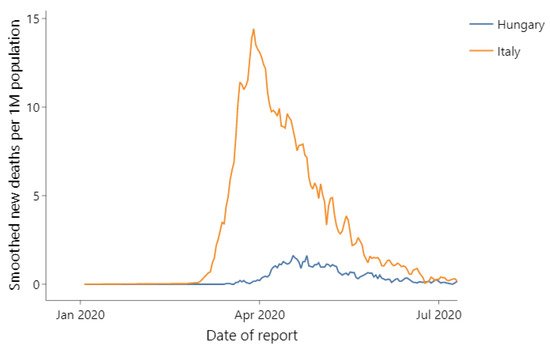
Figure 1. New coronavirus-related deaths in Italy and in Hungary.
European governments implemented a wide range of responses and measures to tackle the pandemic which served, in part, to shield older adults from the virus. However, these also had adverse side effects, including increased social isolation, economic difficulties, delayed medical treatment and challenges to get basic needs met [16]. Several countries reported a reduction in community services, either in order to protect care recipients from contracting SARS-CoV-2 virus, or due to general regulations to close down certain services for the pandemic period [24].
These measures may also have affected the mental health and well-being of family carers, the population group providing the bulk of care to older people. This problem might have been exacerbated due to the fact that migrant care workers in many cases reduced or stopped providing support to family carers [47][48].
The Government Response Stringency Index [49] is used here to indicate the strictness of “lockdown-style” policies adopted in Italy and Hungary (Figure 2). The index provides a systematic, cross-national, cross-temporal measure aimed at understanding how government responses evolved over the period of the disease’s spread. The index, which has a value from 0 to 100 (100 = strictest response), is a composite measure of nine response indicators including school closures, workplace closures and travel bans, recording the strictness of government policies.
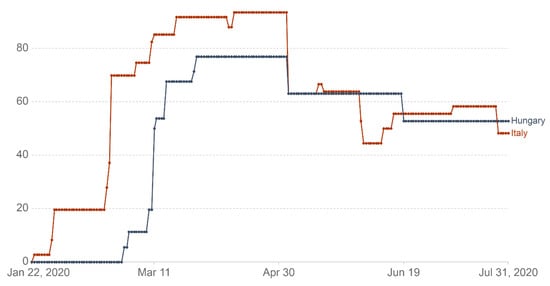
Figure 2. COVID-19: Government Response Stringency Index.
On the date the WHO declared COVID-19 a pandemic (11 March 2020), Italy was the only country in Europe with a high stringency index score (85.9), with the next four countries (including Hungary) having scores between 40 and 50, while other European states had even lower scores.
Figure 2 shows that the Italian government adopted a more restrictive set of measures between January and July 2020, being the first European country to put a comprehensive lockdown in place. The stringency of measures enacted by governments increased sharply in both countries, reaching a peak in April 2020 and then dropping significantly in early May, to substantially stabilize in the following months, albeit with some fluctuations. Table 1 details the measures taken by the Italian and Hungarian governments [50][51][52].
Table 1. Detailed measures for tackling the COVID-19 outbreak in Italy and Hungary between January and July 2020.
| Month | Italy | Hungary |
|---|---|---|
| January 2020 | 1. Highlighted potential risks associated with new coronavirus 2. Declaration of the emergency situation for six months |
1. Draft Action Plan |
| February 2020 | 1. Lockdown of 11 municipalities having outbreaks (the so called “red zones”) 2. Prohibition of access and removal from these municipalities 3. Closing of schools, cultural settings, commercial activities—excluding those for the sale of basic goods 4. Prohibition of meetings, etc. |
|
| March 2020 | 1. In Lombardy and other 14 Italian provinces: (1) Prohibition of access and removal from these territories (2) Shutdown of schools: switch to digital education (3) Ban of cultural, sports events, etc. (4) Restriction of opening hours of restaurants (5) Limitation of visits to residential/nursing homes 2. The above limitations extended to the whole territory: national lockdown (1) Prohibited all persons from moving with public or private means of transport to municipalities, except for proven working needs, health reasons or necessity (2) Parks closed, sport only in the vicinity of home |
1. Shutdown: social institutions 2. Set up the National Operational Team 3. Declaration of pandemic by the WHO: (1) Epidemical emergency situation (2) Border control, quarantine (3) Shutdown of higher education (4) Prohibition of meetings 4. Stringency package: (1) Restrictions of opening hours: restaurants, shops (exemption e.g., Food stores, pharmacies) (2) Ban of cultural, sports events, etc. (3) “Stay at home” request for 70 + (4) Shut down of schools: switch to digital education 5. Lockdown, exemptions: (1) Go to work, pharmacy, food store, market (2) Go to health institutions) (3) Handle essential administration, religious practice (4) Sport activities, alone or living in the same household (5) Shopping: 9 to 12 a.m. Only 65 years old 6. Prolongation of emergency situation 7. Detailed measures of daily life |
| April 2020 | 1. Prolongation of lockdown (1) Hospital: 60 per cent of patients discharged (2) Restart life except the capital (3) Keeping digital education (4) Shopping limitation for 65 + |
|
| May 2020 | 1. “Phase 2”—loosening of containment measures/making life easier: (1) Resumption of work for some categories of employees (2) Possibility of meeting relatives and loved ones (3) Reopening of parks (4) End of national lockdown |
1. End of lockdown |
| June 2020 | 1. “Phase 3”—coexistence with the virus/further loosening of containment measures: (1) Reopened bathing establishments, cultural and social centers, etc. |
1. End of emergency situation. 2. Introduction of transitional arrangements |
| July 2020 | 1. Extension of the emergency situation (initially until 15 October 2020, then to 31 January 2021 (and then, due to the “second wave” of the pandemic, to 31 July 2021) |
As shown in Table 1, several measures were similar in Italy and Hungary, and correspond to different components of the stringency index (e.g., schools closing, public events cancelled, restrictions on gatherings and staying at home). However, there was no limitation on the use of transportation between municipalities in Hungary. In Italy, sports activities were not allowed outside the vicinity of one’s home, while in Hungary, individuals and persons living in the same household were allowed to exercise outside. Shopping from 9 a.m. until 12 a.m. was only permitted for those over 65 years of age in Hungary. In both countries, due to the spread of the virus and the related dramatic consequences especially affecting frail and older people, specific restrictions and limitations to the access of relatives and visitors to residential/nursing homes were established.
The declared state of emergency was much longer in Italy, initially spanning six months from 31 January until 31 July, then extended to 15 October and subsequently, to 31 January 2021 (and then, due to the “second wave” of the pandemic, to 31 July 2021). A state of emergency was declared in Hungary on 11 March 2020 and lasted until 18 June of the same year. The Italian responses might have been considered by the Hungarian government as it introduced a comprehensive stringency package, the instructions of which came into force simultaneously on 16 March 2020 instead of being gradually phased in.
In short, stringency measures during the first wave of the pandemic covered a shorter period in Hungary, concentrated mostly on the capital and the surrounding counties and, in general, citizens enjoyed more freedom than in Italy.
References
- World Health Organization. Dementia: A Public Health Priority; WHO: Geneva, Switzerland, 2012; Available online: (accessed on 18 January 2021).
- Zarit, S.; Orr, N.K.; Zarit, J.M. The Hidden Victims of Alzheimer’s Disease: Families Under Stress; New York University Press: New York, NY, USA, 1995; p. 238.
- United Kingdom Department of Health. Living Well With Dementia: A National Dementia Strategy; Department of Health: London, UK, 2009; p. 102.
- Oliveira, D.; Vass, C.; Aubeeluck, A. Quality of Life on the Views of Older Family Carers of People with Dementia. Dementia 2017, 18, 990–1009.
- World Health Organization. WHO COVID-19 Explorer; WHO: Geneva, Switzerland, 2020; Available online: (accessed on 23 January 2021).
- Ory, M.G.; Hoffman, R.R.; Yee, J.L.; Tennstedt, S.; Schulz, R. Prevalence and impact of caregiving: A detailed comparison between dementia and nondementia caregivers. Gerontologist 1999, 39, 177–185.
- Brodaty, H.; Donkin, M. Family caregivers of people with dementia. Dialogues Clin. Neurosci. 2009, 11, 217–228.
- Hooker, K.; Bowman, S.; Coehlo, D.P.; Lim, S.R.; Kaye, J.; Guariglia, R.; Li, F. Behavioral Change in Persons With Dementia: Relationships With Mental and Physical Health of Caregivers. J. Gerontol. B Psychol. Sci. Soc. Sci. 2002, 57, 453–460.
- Vitaliano, P.P.; Zhang, J.; Scanlan, J.M. Is Caregiving Hazardous to One’s Physical Health? A Meta-Analysis. Psychol. Bull. 2003, 129, 946–972.
- Kröger, T.; Yeandle, S. Combining Paid Work and Family Care: Policies and Experiences in International Perspective; Policy Press: Bristol, UK, 2013; p. 264.
- Socci, M.; Principi, A.; Di Rosa, M.; Carney, P.; Chiatti, C.; Lattanzio, F. Impact of working situation on mental and physical health for informal caregivers of older people with Alzheimer’s disease in Italy. Results from the UP-TECH longitudinal study. Aging Ment. Health 2021, 25, 22–31.
- Italian Alzheimer’s Disease Association and CENSIS Foundation (Associazione Italiana Malattia di Alzheimer and Fondanzione CENSIS). L’impatto Economico E Sociale Della Malattia Di Alzheimer: Rifare Il Punto Dopo 16 Anni; Fondazione CENSIS: Rome, Italy, 2016; p. 16.
- Ikeda, S. Family Care Leave and Job Quitting Due to Caregiving: Focus on the Need for Long-Term Leave. Japan Labor. Rev. 2017, 14, 25–44.
- Smith, G.C.; Tobin, S.S.; Robertson-Tchabo, E.A.; Power, P.W. (Eds.) Strengthening Aging Families: Diversity in Practice and Policy, 1st ed.; Sage Publications, Inc.: Thousand Oaks, CA, USA, 1995; p. 304.
- Cacciapaglia, G.; Cot, C.; Sannino, F. Second wave COVID-19 pandemics in Europe: A temporal playbook. Sci. Rep. UK 2020, 10, 15514.
- Miller, E.A. Protecting and Improving the Lives of Older Adults in the COVID-19 Era. J. Aging Soc. Policy 2020, 32, 297–309.
- Giebel, C.; Cannon, J.; Hanna, K.; Butchard, S.; Eley, R.; Gaughan, A.; Komuravelli, A.; Shenton, J.; Callaghan, S.; Tetlow, H.; et al. Impact of COVID-19 related social support service closures on people with dementia and unpaid carers: A qualitative study. Aging Ment. Health 2020, 1–8.
- Barry, H.E.; Hughes, C.M. Managing medicines in the time of COVID-19: Implications for community-dwelling people with dementia. Int. J. Clin. Pharm. Net. 2020, 43, 1–5.
- Rodrigues, R.; Simmons, C.; Schmidt, A.E.; Steiber, N. Care in times of COVID-19: The impact of the pandemic on informal caregiving in Austria. Eur. J. Ageing 2020, 1–11.
- Vaitheswaran, S.; Lakshminarayanan, M.; Ramanujam, V.; Sargunan, S.; Venkatesan, S. Experiences and Needs of Caregivers of Persons with Dementia in India During the COVID-19 Pandemic—A Qualitative Study. Am. J. Geriatr. Psychiatry 2020, 28, 1185–1194.
- Cohen, G.; Russo, M.J.; Campos, J.A.; Allegri, R.F. COVID-19 Epidemic in Argentina: Worsening of Behavioral Symptoms in Elderly Subjects with Dementia Living in the Community. Front. Psychiatry 2020, 11, 866.
- Tsapanou, A.; Papatriantafyllou, J.D.; Yiannopoulou, K.; Sali, D.; Kalligerou, F.; Ntanasi, E.; Zoi, P.; Margioti, E.; Kamtsadeli, V.; Hatzopoulou, M.; et al. The impact of COVID-19 pandemic on people with mild cognitive impairment/dementia and on their caregivers. Int. J. Geriatr. Psychiatry 2020, 36, 583–587.
- Family Carers Ireland. Caring Through Covid: Life in Lockdown; Family Carers Ireland: Dublin, Ireland, 2020; p. 20.
- Carers UK. Caring behind Closed Doors: Forgotten Families in The Coronavirus Outbreak; Carers UK: London, UK, 2020; p. 30.
- Rothgang, H.; Wolf-Ostermann, K.; Domhoff, D.; Franziska, H.; Heß, M.; Kalwitzki, T.; Ratz, K.; Schmidt, A.; Seibert, K.; Stolle, C.; et al. How Covid-19 Has Affected Informal Caregivers and Their Lives in Germany. 2020. Available online: (accessed on 27 January 2021).
- Giebel, C.; Hanna, K.; Cannon, J.; Eley, R.; Tetlow, H.; Gaughan, A.; Komuravelli, A.; Shenton, J.; Rogers, C.; Butchard, S.; et al. Decision-making for receiving paid home care for dementia in the time of COVID-19: A qualitative study. BMC Geriatr. 2020, 20, 333.
- Cohen, G.; Russo, M.J.; Campos, J.A.; Allegri, R.F. Living with dementia: Increased level of caregiver stress in times of COVID-19. Int. Psychogeriatr. 2020, 32, 1377–1381.
- Tróbert, A.; Bagyura, M.; Széman, Z. Családi gondozók és idősellátás a COVID-19 idején (Family Carers and the care for older people in the time of COVID 19), 2020. In Proceedings of the XXIV conference of Apáczai Csere Days, Győr, Hungary, 19 November 2020.
- Goodman-Casanova, J.M.; Dura-Perez, E.; Guzman-Parra, J.; Cuesta-Vargas, A.; Mayoral-Cleries, F. Telehealth Home Support During COVID-19 Confinement for Community-Dwelling Older Adults With Mild Cognitive Impairment or Mild Dementia: Survey Study. J. Med. Internet. Res. 2020, 22, e19434.
- Cuffaro, L.; Di Lorenzo, F.; Bonavita, S.; Tedeschi, G.; Leocani, L.; Lavorgna, L. Dementia care and COVID-19 pandemic: A necessary digital revolution. Neurol. Sci. 2020, 41, 1977–1979.
- sm-Rahman, A.; Lo, C.H.; Ramic, A.; Jahan, Y. Home-Based Care for People with Alzheimer’s Disease and Related Dementias (ADRD) during COVID-19 Pandemic: From Challenges to Solutions. Int. J. Env. Res. Pub. Health 2020, 17, 9303.
- Gabbrielli, F.; Bertinato, L.; De Filippis, G.; Bonomini, M.; Cipolla, M. Interim Provisions on Telemedicine Healthcare Services During COVID-19 Health Emergency. Version of April 13, 2020; Istituto Superiore di Sanità (Italian National Institute of Health): Rome, Italy, 2020; p. 38.
- Alzheimer Europe. Dementia in Europe Yearbook 2019: Estimating the Prevalence of Dementia in Europe; Alzheimer Europe: Luxembourg, 2019; p. 108.
- Vetrano, D.L.; Vaccaro, K. Home Care in Italy: Who Does It, How to Do it and Good Practices; Italia Longeva: Rome, Italy, 2018; p. 72.
- Tidoli, R. Domicialirity. In Care of Non Self-Sufficient Older People in Italy. 6th Report, 2017–2018; NNA Network Non Autosufficienza, Ed.; Maggioli, S.p.A.: Sant’Arcangelo di Romagna, Italy, 2017; pp. 77–100.
- Barbabella, F.; Poli, A.; Chiatti, C.; Pelliccia, L.; Pesaresi, F. The compass of NNA: The state of the art based on data. In Care of Non Self-Sufficient Older People in Italy, 6th Report, 2017–2018; NNA Network Non Autosufficienza, Ed.; Maggioli, S.p.A.: Sant’Arcangelo di Romagna, Italy, 2017; pp. 33–54.
- Barbabella, F.; Chiatti, C.; Rimland, J.M.; Melchiorre, M.G.; Lamura, G.; Lattanzio, F. Up-Tech Research Group. Socioeconomic Predictors of the Employment of Migrant Care Workers by Italian Families Assisting Older Alzheimer’s Disease Patients: Evidence from the Up-Tech Study. J. Gerontol. B Psychol. Sci. Soc. Sci. 2016, 71, 514–525.
- Schmidt, A.E. Analysing the importance of older people’s resources for the use of home care in a cash-for-care scheme: Evidence from Vienna. Health Soc. Care Community 2017, 25, 514–526.
- De Luca, M.; Tronchin, C.; Di Pasquale, E. 2nd Annual Report on Domestic Work. Analysis, Statistics, National and Local Trends; Osservatorio Nazionale DOMINA sul Lavoro Domestico: Rome, Italy, 2020; p. 294.
- Kuhlmann, E.; Greer, S.L.; Burau, V.; Falkenbach, M.; Jarman, H.; Pavolini, E. The migrant health workforce in European countries: Does anybody care? Eur. J. Public Health 2019, 29, ckz185-565.
- Italian Presidency of the Council of Ministers. Definizione dei Livelli Essenziali di Assistenza (Definition of Essential Levels of Assistance). Gazzetta Ufficiale della Repubblica Italiana, Suppl. Ordinario alla Gazzetta Ufficiale n.33 del 08-02-2002—Serie Generale (Italian Official Gazette). 2002. Available online: (accessed on 25 January 2021).
- Gyarmati, A. Ageing and Care for the Elderly in Hungary; Friedrich-Ebert-Stiftung, Budapest Office: Buadapest, Hungary, 2019.
- Hungarian Parliament. 1993 III. Act on Social Administration and Social Benefits; Cabinet of Prime Minister: Budapest, Hungary, 1993.
- National Center for Disability Affairs and Social Policy. Unified Disability Information Portal. 2021. Available online: (accessed on 26 January 2021).
- Hungarian Parliament. 1997 CLIV. Act on Healthcare; Cabinet of Prime Minister: Budapest, Hungary, 1997.
- Széman, Z. Family Strategies in Hungary: The Role of Undocumented Migrants in Eldercare. J. Popul. Ageing 2012, 5, 97–118.
- Lorenz-Dant, K. Germany and the COVID-19 long-Term Care Situation; International Long Term Care Policy Network; CPEC-LSE: London, UK, 2020.
- Schmidt, A.E.; Leichsenring, K.; Staflinger, H.; Litwin, C.; Bauer, A. The Impact of COVID-19 on Users and Providers of Long-Term Care Services in Austria; International Long Term Care Policy Network. CPEC-LSE, London, UK. 2020. Available online: (accessed on 25 January 2021).
- Hale, T.; Angrist, N.; Cameron-Blake, E.; Hallas, L.; Kira, B.; Majumdar, S.; Petherick, A.; Phillips, T.; Tatlow, H.; Webster, S. Oxford COVID-19 Government Response Tracker, Blavatnik School of Government. 2020. Available online: (accessed on 23 January 2021).
- Hungarian Government. Information Page on the Coronavirus. 2020. Available online: (accessed on 8 August 2020).
- Hungarian Ministry of Justice. Hungarian Official Gazette. 2020. Available online: (accessed on 8 August 2020).
- Italian Presidency of the Council of Ministers. Information Page on the Coronavirus. 2021. Available online: (accessed on 26 January 2021).




