Although radiological diagnostics have been progressing, pathological diagnosis remains the most reliable method for diagnosing liver tumors. In some cases, definite pathological diagnosis cannot be obtained by histological evaluation alone, especially when the sample is a small biopsy; in such cases, immunohistochemical staining is very useful. Immunohistochemistry is the most frequently used technique for molecular pathological diagnosis due to its broad application, ease of performance and evaluation, and reasonable cost. The results occasionally reflect specific genetic mutations. The immunohistochemical markers of hepatocellular carcinoma include those of hepatocellular differentiation—such as hepatocyte paraffin 1 and arginase-1—and those of malignant hepatocytes—such as glypican-3, heat shock protein 70, and glutamine synthetase (GS). To classify the subtypes of hepatocellular adenoma, examination of several immunohistochemical markers, such as liver fatty acid-binding protein, GS, and serum amyloid A, is indispensable. Immunohistochemical staining for GS is also important for the diagnosis of focal nodular hyperplasia. The representative immunohistochemical markers of intrahepatic cholangiocarcinoma include cytokeratin (CK) 7 and CK19.
1. Introduction
Although radiological diagnostics have been progressing, pathological diagnosis remains the most reliable method for diagnosing liver tumors, with accurate pathological diagnosis being essential for appropriate treatment. Liquid biopsy has been increasingly used, but traditional biopsy with immunohistochemistry still has its role. Histologic evaluation by microscopic observation of specimens stained with hematoxylin and eosin and other special stains, such as silver stains, is important in the pathological diagnosis of liver tumors. However, definite diagnosis cannot be obtained by histological evaluation alone in some cases, especially when the sample is a small biopsy; in such cases, immunohistochemical staining is very useful. Molecular pathological diagnosis involves various techniques—such as in situ hybridization, reverse transcription polymerase chain reaction (RT-PCR), and DNA sequencing; immunohistochemistry is the most frequently used technique due to its broad application, ease of performance and evaluation, and reasonable cost. The results of immunohistochemistry occasionally reflect specific genetic mutations. In this article, we provide an overview of the application of immunohistochemistry in the pathological diagnosis of liver tumors referring to the association with genetic alterations. Furthermore, we aimed to explain the practical points in the differential diagnosis of liver tumors by immunohistochemical staining.
2. Immunohistochemical Markers of Liver Tumors
2.1. Immunohistochemical Markers of Hepatocellular Carcinoma
2.1.1. Markers of Hepatocellular Differentiation
Hepatocyte Paraffin 1
Hepatocyte paraffin 1 (Hep Par 1) is a monoclonal antibody that was developed in 1993 using immunogens obtained from failed liver allografts ()
[1]. It was later elucidated that the antigen for Hep Par 1 is the urea cycle enzyme carbamoyl phosphate synthetase 1
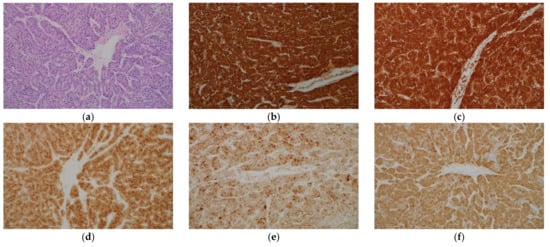
[2]. Hep Par 1 stains tumorous and non-tumorous hepatocytes and shows a diffuse cytoplasmic granular staining pattern (a,b). The sensitivity of Hep Par 1 for the diagnosis of hepatocellular carcinoma (HCC) is more than 70%, and the specificity is also high
[3][4][5][6][7]. However, there are several limitations in using this antibody for the diagnosis of HCC. First, it has a low sensitivity for diagnosing poorly differentiated HCC and scirrhous HCC
[8][9]. Second, adenocarcinomas of various organs may show immunohistochemical positivity with Hep Par 1, although the frequency is low
[4][6][10]. Finally, hepatoid carcinomas occurring in various organs often show immunohistochemical positivity with Hep Par 1
[11][12].
Figure 1. Histological appearance (a) and results of immunohistochemical staining (b–f) of hepatocellular carcinoma. (a) Tumor cells resembling hepatocytes proliferate, showing thick trabecular growth pattern. On immunohistochemistry, the tumor cells are positive for hepatocyte paraffin 1 (b), arginase-1 (c), glypican-3 (d), heat shock protein 70 (e), and glutamine synthetase (GS) (f). (Original magnification: ×200 for (a–f)).
Table 1. Immunohistochemical markers of HCC.
| Marker |
Staining Pattern |
Characteristics |
| Markers of Hepatocellular Differentiation |
| Hepatocyte paraffin 1 |
Cytoplasmic |
The sensitivity decreases in the diagnosis of poorly differentiated HCC and scirrhous HCC. |
| Arginase-1 |
Cytoplasmic with variable nuclear reactivity |
This is the most sensitive marker of HCC and shows high sensitivity even in poorly differentiated HCC and scirrhous HCC. |
| pCEA |
Canalicular |
The sensitivity decreases in poorly differentiated HCC. The staining may be difficult to interpret. |
| CD10 |
Canalicular |
The sensitivity tends to be lower compared to pCEA. |
| Markers of Malignant Hepatocytes |
| Glypican-3 |
Cytoplasmic, membranous, and canalicular |
The sensitivity is low in well differentiated HCC and high in moderately and poorly differentiated HCC. |
| Heat shock protein 70 |
Nuclear and cytoplasmic |
The staining pattern is usually patchy. Benign hepatocytes may be stained. |
| Glutamine synthetase |
Cytoplasmic |
This cannot be used in the differential diagnosis between HCC and HCA, and between hepatocellular and non-hepatocellular neoplasms. |
| α-Fetoprotein |
Cytoplasmic |
The sensitivity is low. |
| CD34 |
Sinusoidal |
The evaluation is subjective. |
Arginase-1
Arginase-1 (Arg-1) is a binuclear manganese metalloenzyme mainly found in the liver that catalyzes the hydrolysis of arginine to ornithine and urea in the urea cycle
[8][13]. Immunohistochemistry for Arg-1 stains both tumorous and non-tumorous hepatocytes and shows diffuse cytoplasmic staining pattern with variable nuclear reactivity (c). Arg-1 is the most sensitive marker of HCC, with a high sensitivity even in poorly differentiated HCC and scirrhous HCC
[8][9]. The specificity of Arg-1 immunohistochemistry for HCC is also high
[13][14]. Positive staining is also observed in hepatoblastomas
[15]. However, adenocarcinomas in various organs may show positivity for Arg-1, although the frequency is low
[16], and hepatoid carcinomas occasionally exhibit positive staining for Arg-1
[12].
Polyclonal Carcinoembryonic Antigen
Carcinoembryonic antigen (CEA) is a glycoprotein found in the glycocalyx of fetal epithelial cells; a small amount of CEA is also observed in normal adult cells
[8][17]. Polyclonal anti-CEA antibody (pCEA) cross-reacts with biliary glycoprotein and shows a characteristic canalicular staining pattern in normal liver tissue
[18]. This canalicular staining pattern is maintained in many cases of HCC, with more than 70% cases showing positive staining
[5][19]. Conversely, many adenocarcinomas, including cholangiocarcinoma, show diffuse cytoplasmic, membranous, and/or luminal staining patterns. In case of poorly differentiated HCC, the diagnostic sensitivity decreases, and the staining pattern may be cytoplasmic; therefore, pCEA staining has limited ability to differentially diagnose poorly differentiated HCC and adenocarcinoma
[18][20]. Luminal or membranous staining in adenocarcinomas and canalicular staining in HCC may appear confusing to pathologists. In addition, canalicular staining patterns are occasionally difficult to recognize for unexperienced pathologists. Due to these shortcomings of pCEA, Hep Par 1, and Arg-1 are currently more frequently used than pCEA as immunohistochemical markers of HCC.
CD10, Villin, and Bile Salt Export Protein
CD10 shows a canalicular staining pattern in tumorous and non-tumorous hepatocytes, similar to that of pCEA staining; however, the sensitivity of immunohistochemical staining for CD10 for HCC diagnosis tends to be lower than that for pCEA
[6][21][22]. The interpretation of staining is easier for CD10 than for pCEA because cytoplasmic staining is less frequently observed
[18]. Immunohistochemistry for villin and bile salt export protein (BSEP) shows similar canalicular staining patterns in HCC
[4][12][17].
2.1.2. Markers of Malignant Hepatocytes
Glypican-3
Glypican-3 (GPC-3) is a heparan sulfate proteoglycan that is attached to the cell surface by a glycosyl-phosphatidylinositol anchor; it is highly expressed in embryonic tissues but has a low expression in normal adult tissues
[23]. Positive staining for GPC-3 is observed in approximately 80–90% of HCC cases (d), but negative in the normal liver, hepatocellular adenoma (HCA), focal nodular hyperplasia (FNH), and large regenerative nodule
[24][25][26]. It has cytoplasmic, membranous, and canalicular staining patterns. It may be stained diffusely or focally, and the sensitivity of GPC-3 immunohistochemistry for the diagnosis of HCC is as low as approximately 50% with needle biopsy specimens
[16][27]. The sensitivity for the diagnosis of moderately and poorly differentiated HCC exceeds 80%, whereas that for the diagnosis of well differentiated HCC is as low as approximately 60%
[25]. This finding is important because Hep Par 1 immunostaining has a low sensitivity for diagnosing poorly differentiated HCC. It was reported that 100% of poorly differentiated HCCs could be detected by combining GPC-3 and Arg-1
[8]. The positive rate in scirrhous HCC is as high as approximately 80%
[9]. However, the fact that cirrhotic nodules and active hepatitis C cases may stain positively for GPC-3 requires attention
[24][28][29]. Furthermore, GPC-3 expression is frequently observed in hepatoblastoma and undifferentiated embryonal sarcoma
[30][31], and dysplastic nodule (DN) may also show positive staining
[25][32]. In addition to liver tumors, the expression of GPC-3 is frequently observed in squamous cell carcinoma of the lung, testicular non-seminomatous germ cell tumors, and liposarcoma
[33].
Heat Shock Protein 70
Heat shock protein (HSP) 70 is an anti-apoptotic regulator that promotes cell survival and may be associated with tumorigenesis
[34]. In a study of gene expression profiles in HCC, HSP70 was the most abundantly upregulated gene in early HCC
[35]. Immunohistochemical examination showed that HSP70 expression was the highest in progressed HCC, followed by early HCC, and then, precancerous lesions, in that order
[35]. The sensitivity and specificity of HSP70 immunostaining in the diagnosis of early and grade 1 HCC were 78% and 95%, respectively
[36]. The staining pattern is usually patchy, and the nucleus and cytoplasm are stained; diffuse staining is observed in only one-third of the cases (e)
[18][36]. The bile duct epithelium is also stained, which can serve as an internal control. Special attention is required during pathologic evaluation since benign hepatocytes may also be stained. When non-tumorous tissue is also sampled, more intense staining in the tumorous tissue than in the non-tumorous tissue should be interpreted as positive staining. HCA cases show no immunostaining for HSP70
[37][38]. HSP70 is not useful in differentiating hepatocellular from non-hepatocellular neoplasms as it is frequently expressed in intrahepatic cholangiocarcinoma (ICC) and metastatic liver tumors
[39].
Glutamine Synthetase
Glutamine synthetase (GS) catalyzes the synthesis of glutamine by promoting the condensation of glutamate and ammonia in the liver
[34][40]. GS is the target of β-catenin and is upregulated when this pathway is activated. In the normal liver, the expression of GS is confined in two to three cell-thick hepatocytes around the central veins
[41]. In a cirrhotic liver, this characteristic staining pattern is not maintained
[18]. GS is a marker of HCC and immunostaining for GS is positive in 80% of low-grade HCC cases (f)
[37]. As described below, immunohistochemical staining for GS is also useful in the diagnosis of FNH and a certain type of HCA. GS immunostaining is not useful in differentiating hepatocellular from non-hepatocellular neoplasms as GS expression is observed in 76% of ICCs and 71% of metastatic liver tumors
[39].
α-Fetoprotein
α-Fetoprotein (AFP) is an oncofetal protein produced by the liver and visceral endoderm of the yolk sac
[17][20]. Although it is a marker of HCC, germ cell tumors, such as yolk sac tumor, also express this protein. Although serum AFP levels often increase in patients with HCC, the sensitivity of immunohistochemical staining for AFP for diagnosing HCC is as low as approximately 30%, and the staining pattern is patchy in many cases
[4][6]. Therefore, immunohistochemical staining for AFP has limited utility in HCC diagnosis. Presently, immunohistochemical staining for AFP is less frequently performed for the diagnosis of HCC, because better diagnostic markers have been developed.
CD34
CD34 is useful for the diagnosis of liver tumors because it shows different staining patterns between tumorous and non-tumorous liver tissues. In a normal liver or a cirrhotic liver, immunohistochemistry for CD34 stains the endothelial cells of blood vessels in the portal tracts and the fibrous septa; however, the sinusoidal endothelial cells are not stained, except in the areas adjacent to the portal tracts and fibrous septa. Arterialization in HCC, HCA, and FNH induces the capillarization of sinusoids and sinusoidal endothelial cells stain positively for CD34. Diffuse staining of the sinusoidal endothelial cells is observed in almost all cases of HCC
[26]. Many cases of HCA and FNH show incomplete staining patterns, with rare instances of diffuse staining patterns
[26].
2.1.3. Subtypes of Hepatocellular Carcinoma That Show Special Immunohistochemical Staining Patterns
Scirrhous Hepatocellular Carcinoma
Scirrhous HCC is a rare subtype of HCC characterized by prominent stromal fibrosis
[9][42]. Other characteristics of scirrhous HCC include its subcapsular location, contiguous multinodular-type gross appearance, absence of capsule and necrosis, preserved portal tracts in the tumor, remarkable lymphocytic infiltration, clear cell change, and presence of hyaline bodies
[42][43]. It was reported that the sensitivity of immunostaining with Hep Par 1 and pCEA for diagnosing scirrhous HCC was as low as 26% and 37%, respectively, while that of epithelial cell adhesion molecule (EpCAM), cytokeratin (CK) 19, and CK7 immunostaining was as high as 63%, 26%, and 53%, respectively
[9]. Scirrhous HCC is prone to be misdiagnosed as ICC or metastatic adenocarcinoma due to the abundant stroma and the abovementioned immunohistochemical features. The sensitivity of GPC-3 and Arg-1 immunostaining for diagnosing scirrhous HCC have been reported to be as high as 79% and 85%, respectively, and it was 100% when these two markers were used in combination
[9]. Therefore, immunohistochemical staining for GPC-3 and Arg-1 is useful for the diagnosis of scirrhous HCC.
Fibrolamellar Hepatocellular Carcinoma
This subtype of HCC is characterized by a lamellar pattern of fibrosis and presence of large tumor cells with abundant eosinophilic cytoplasm
[44][45], and almost all cases express CK7
[46][47][48]. Fibrolamellar HCC usually demonstrates positive immunostaining with anti-Arg-1, Hep Par 1, and pCEA antibodies, but the positivity rate of GPC-3 immunostaining is rather low (17–64%)
[25][44][45][47][48]. Although almost all fibrolamellar HCC cases show a distinctive granular, dot-like, or stippled pattern of cytoplasmic staining for CD68, the positivity rate in control HCCs was reported to be approximately 25% when the background liver was non-cirrhotic, and approximately 10% when the background liver was cirrhotic
[49]. Therefore, the diagnosis of fibrolamellar HCC should be established cautiously when immunohistochemical staining for CK7 and CD68 is negative. The
DNAJB1-PRKACA fusion gene, a result of ~400-kilobase deletions on chromosome 19, is characteristically found in fibrolamellar HCC; RT-PCR, fluorescence in situ hybridization, and RNA in situ hybridization are useful for its detection
[50][51]. These molecular pathological techniques are useful in cases where fibrolamellar HCC is suspected but definite diagnosis cannot be made based on the histologic and immunohistochemical findings alone. However, it was recently reported that
DNAJB1-PRKACA fusion is also observed in oncocytic pancreatic and biliary neoplasms and is not specific to fibrolamellar HCC
[52].
2.2. Immunohistochemical Characteristics of Focal Nodular Hyperplasia
FNH is considered to be a hyperplastic lesion of the hepatocytes due to increased blood flow associated with vascular malformation
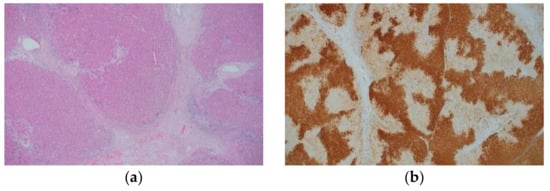
[53]. FNH is characterized by nodular architecture, thick fibrous septa with or without a central scar, thick-walled abnormal blood vessels, and ductular reaction (a and )
[17][45][54]. FNH shows a characteristic map-like pattern in the immunohistochemical staining for GS (b). Namely, large areas with positively stained hepatocytic cytoplasm anastomose, often surrounding the hepatic veins, and intermingle with small unstained areas that are close to the fibrous bands containing arteries and ductules
[55]. This map-like pattern must be differentiated from the diffuse GS staining pattern, a characteristic of β-catenin activation; however, this differentiation may be difficult with small biopsy specimens. On the contrary, as aforementioned, the expression of GS is restricted to two to three cell-thick hepatocytes around the central veins in a normal liver. Positive staining for serum amyloid A (SAA) is observed in approximately 20% of FNH cases
[56], and the map-like GS staining pattern is useful in differentiating FNH from inflammatory hepatocellular adenoma (IHCA) (described later). In FNH, activating mutations of
CTNNB1 (encoding β-catenin) are not observed despite the fact that the β-catenin pathway is activated
[57][58]. The expansion of areas with GS-positive hepatocytes in FNH is attributed to this phenomenon.
Figure 2. Histological appearance (a) and results of immunohistochemical staining (b) of focal nodular hyperplasia. (a) The lesion is characterized by thick fibrous septa with a central scar, thick-walled abnormal blood vessels, and ductular reaction. (b) Immunohistochemistry for GS shows a map-like staining pattern. (Original magnification: ×100 for (a,b)).
Table 2. Molecular findings, histological features, and immunohistochemical findings of FNH and HCA.
| Item |
FNH |
H-HCA |
IHCA |
b-HCA |
| Molecular findings |
Activation of the β-catenin pathway without mutations of CTNNB1 |
Biallelic mutations of HNF1A |
Activation of the IL-6 signaling pathway due to mutations in IL6ST, FRK, STAT3, GNAS, and JAK1 |
Activation of the WNT signaling pathway due to mutation or deletion of CTNNB1 |
| Histological features |
Thick fibrous septa with or without a central scar, abnormal blood vessels, and ductular reaction |
Prominent steatosis |
Sinusoidal dilation, patchy inflammatory cell infiltration, and variable steatosis |
Cellular and structural atypia and pseudoglands |
| Immunohistochemical findings |
| LFABP |
(+) |
(−) |
(+) |
(+) |
| β-catenin |
Membranous |
Membranous |
Membranous |
Nuclear |
| GS |
Map-like |
Patchy with perivascular accentuation |
Patchy with perivascular accentuation |
Diffuse homogenous or heterogenous staining depending on the mutation type |
| SAA/CRP |
Usually (−) |
(−) |
Strong and diffuse |
(−) |
| OATP1B3 |
(+) |
(−) |
(−) |
(+) |
2.3. Immunohistochemical Characteristics of Hepatocellular Adenoma
HCA is a relatively rare benign tumor of hepatocytic origin. The risk factors for HCA include female sex, exposure to steroid sex hormones (oral contraceptives, anabolic steroids, and pregnancy), glycogenosis types 1 and 3, maturity onset diabetes of the young type 3 (MODY3), and familial polyposis coli
[34][59][60]. Currently, advancements in molecular pathological studies have enabled the classification of HCA into several types (). Each type has unique morphological features, but examination using several immunohistochemical markers is indispensable for accurate classification.
2.3.1. Hepatocyte Nuclear Factor 1A-Inactivated Hepatocellular Adenoma
This subtype is characterized by mutations in the
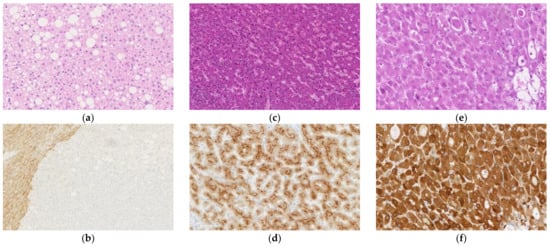
hepatocyte nuclear factor (HNF) 1A gene. It mostly occurs in young women and presents with prominent steatosis (a), although some cases lack this feature. Sinusoidal dilation and cellular atypia do not usually occur, and it rarely progresses to HCC
[54][60][61]. Liver fatty acid-binding protein (LFABP) is downregulated, and immunohistochemistry for LFABP is negative because of mutation in the
HNF1A gene, which encodes hepatocyte nuclear factor 1 (b). In the normal liver and other types of HCA, the hepatocyte cytoplasm is stained in the immunohistochemistry for LFABP. Immunohistochemical staining for LFABP is not useful for differentiating HCA from HCC since the expression of LFABP may also be downregulated in HCC
[62][63]; it is only useful for subclassification after a definite diagnosis of HCA. Immunohistochemical staining for SAA and C-reactive protein (CRP) as well as nuclear accumulation of β-catenin is usually negative, and GS immunostaining does not show a map-like or diffuse pattern
[54].
Figure 3. Histological appearance (a,c,e) and results of immunohistochemical staining (b,d,f) of hepatocellular adenoma (HCA). (a) Hepatocyte nuclear factor (HNF) 1A-inactivated HCA (H-HCA) shows prominent steatosis. (b) Immunohistochemical staining for liver fatty acid-binding protein is negative in the H-HCA lesion but positive in the surrounding liver tissue. (c) Inflammatory HCA (IHCA) is characterized by sinusoidal dilation and patchy inflammatory cell infiltration. (d) On immunohistochemistry, tumor cells of IHCA are positive for serum amyloid A. (e) β-catenin-activated HCA (b-HCA) may be associated with cellular and structural atypia, and pseudoglands may be observed. (f) b-HCAs with CTNNB1 gene mutations that lead to strong β-catenin pathway activation show a strong/homogenous staining pattern for GS. (Original magnification: ×150 for (a,d), ×100 for (b,c), and ×200 for (e,f)).
2.3.2. Inflammatory Hepatocellular Adenoma
This subtype is characterized by gene mutations that activate the interleukin (IL)-6 signaling pathway, and mutation of the
IL6ST gene, which encodes the signaling co-receptor, gp130, occurs most frequently
[17]. Mutations in
FRK,
STAT3,
GNAS, and
JAK1 have also been reported. Histologically, IHCA is characterized by sinusoidal dilation, patchy inflammatory cell infiltration, and variable steatosis (c)
[54][60]. Differentiation between IHCA and FNH based on the histologic features alone is difficult as IHCA often possesses features common to FNH, such as fibrous septa and ductular reaction
[56]. For this reason, IHCA was formerly called “telangiectatic FNH.” Almost all IHCA cases show strong and diffuse cytoplasmic immunostaining for SAA (d) and CRP, both of which are proteins associated with inflammation
[17][56][60]. However, 15% of FNH cases show diffuse staining for CRP
[56]. IHCA is suggested if a map-like staining pattern is not observed on GS immunostaining and a diffuse staining pattern is observed for CRP immunostaining.
2.3.3. β-Catenin-Activated Hepatocellular Adenoma
This subtype shows activation of the WNT signaling pathway, resulting from mutation or deletion of the
CTNNB1 gene, which encodes β-catenin
[58]. This subtype may be associated with cellular and structural atypia, and pseudoglands may be observed (e). The degree of β-catenin activation is associated with the mutation pattern of the
CTNNB1 gene: (1) S45, K335, and N387 mutations cause weak activation; (2) T41 mutations cause moderate activation; and (3) exon 3 deletions and amino acid substitutions within the β-TRCP binding site (D32-S37) cause a high degree of activation
[64]. This is associated with the immunohistochemical staining pattern for GS. Tumors with mutations that lead to strong β-catenin activation show a strong/homogenous immunostaining pattern (f), while tumors with mutations that lead to weak activation show a heterogeneous pattern, with the former being associated with malignancy
[58]. Many cases of β-catenin-activated HCA (b-HCA) show nuclear staining in immunohistochemistry for β-catenin; however, the staining pattern is only focal and is not observed in some cases
[58]. In the normal hepatocytes, β-catenin staining is observed at the sub-membranous location. Tumors with both IHCA and b-HCA features are called β-catenin-activated IHCA (b-IHCA), and the risk of malignant transformation of b-IHCA is similar to that of b-HCA with mutations in exon 3 of the
CTNNB1 gene
[58]. Our group found that all HCA cases with nuclear accumulation of β-catenin showed preserved or increased expression of organic anion-transporting polypeptide (OATP) 1B3, while almost all HCA cases without nuclear accumulation of β-catenin showed decreased expression of OATP1B3
[65]. OATP1B3 is an organic anion transporter that contributes to the hepatocytic uptake of gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid (Gd-EOB-DTPA), a hepatocyte-specific contrast agent used in magnetic resonance imaging (MRI)
[66]. In accordance with the results of our previous study, the frequency of low signal intensity in the hepatobiliary phase of Gd-EOB-DTPA-MRI is lower in b-HCA than in other HCA subtypes
[67].
2.3.4. Other Types of Hepatocellular Adenoma
HCAs without characteristic pathological or genetic findings are diagnosed as unclassified HCA (UHCA). Henriet et al.
[68] reported an upregulation of the arginine synthesis pathway, which is associated with the overexpression of argininosuccinate synthase 1 and arginosuccinate lyase in UHCA. Nault et al.
[69] reported a subgroup of UHCA in which the sonic hedgehog signaling was activated by deletions that fused the promoter of
INHBE with
GLI1, and these tumors were associated with obesity and bleeding. The classification of HCA might change in the future through further molecular investigations.
2.4. Immunohistochemical Characteristics of Intrahepatic Cholangiocarcinoma
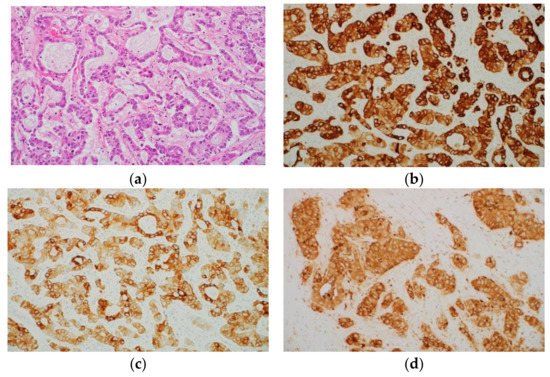
Normal bile duct epithelial cells express CK7 and CK19, and almost all ICC cases also express these proteins (a–c)
[23][70]. Accordingly, CK7 and CK19 can be regarded as markers of biliary differentiation; however, morphologically pure HCC may show positive staining for CK7 and CK19
[71][72][73]. In other words, CK7 and CK19 are not specific markers of ICC. Immunostaining with Hep Par 1 is usually not observed in ICC. However, it was reported that the mucus-secreting cells in approximately 15% of ICC cases showed positive immunostaining with Hep Par 1
[74]. ICC tumor cells often show cytoplasmic and luminal positivity on immunohistochemical staining with monoclonal and polyclonal antibodies against CEA (d). In addition, ICC and metastatic adenocarcinoma frequently show positive staining for EpCAM
[4][5]. However, HCC cases rarely show positive staining for EpCAM
[5][75][76].
Figure 4. Histological appearance (a) and results of immunohistochemical staining (b–d) of intrahepatic cholangiocarcinoma (ICC). (a) Histologically, ICC is an adenocarcinoma. Immunohistochemically, tumor cells are positive for cytokeratin (CK) 7 (b), CK19 (c), and carcinoembryonic antigen (monoclonal antibody) (d). (Original magnification: ×200 for (a–d)).
ICC is classified into large and small duct types. The large duct type ICC is characterized by immunohistochemical expression of MUC5AC and MUC6, and
KRAS mutations, while the small duct type ICC is characterized by immunohistochemical expression of CD56 and CRP, and
IDH1/2 mutations
[58]. Recent studies on ICC suggest that there are molecular subclasses of proliferation and inflammation types in ICC that have different clinicopathological features and gene mutations
[77], some of which may be candidates for targeted, personalized therapy. Furthermore, there appear to be associations between the inflammation subclass and the large duct type, and between the proliferation subclass and the small duct type. Cholangiolocellular carcinoma (CoCC) is a carcinoma characterized by the proliferation of small glands, resembling the bile ductules, and its status in the classification of liver tumors is not definite. Balitzer et al.
[78] reported that results of immunohistochemical staining for CK19, SALL4, CD56, CD117, and epithelial membrane antigen (EMA) as well as the molecular features based on next-generation sequencing results were similar between ICC and CoCC; they argued that CoCC should be classified as a subtype of ICC. In fact, CoCC is classified as a subtype of ICC in the current World Health Organization (WHO) classification, although it was classified as a subtype of combined hepatocellular-cholangiocarcinoma in the previous WHO classification
[58]. However, in our previous study, immunohistochemical staining for β6, β4, and α3 integrins was negative to weakly positive in most cases of CoCC and HCC and strongly positive in most cases of ICC, suggesting that the features of CoCC were similar to those of HCC but not ICC
[79]. It is conceivable that further examination is necessary to determine the position of CoCC.